Abstract
Sepsis is a life-threatening condition in preterm infants. Neonatal microbiota plays a pivotal role in the immune system maturation. Changes in gut microbiota have been associated to inflammatory disorders; however, a link with sepsis in the neonatal period has not yet been established. We aimed to analyze gut microbiota and mucosal gene expression using non-invasively obtained samples to provide with an integrative perspective of host-microbe interactions in neonatal sepsis. For this purpose, a prospective observational case-control study was conducted in septic preterm dizygotic twins and their non-septic twin controls. Fecal samples were used for both microbiota analysis and host genome-wide expression using exfoliated intestinal cells. Gene expression of exfoliated intestinal cells in septic preterm showed an induction of inflammatory and oxidative stress pathways in the gut and pro-oxidant profile that caused dysbiosis in the gut microbiota with predominance of Enterobacteria and reduction of Bacteroides and Bifidobacterium spp.in fecal samples, leading to a global reduction of beneficial anaerobic bacteria. Sepsis in preterm infants induced low-grade inflammation and oxidative stress in the gut mucosa, and also changes in the gut microbiota. This study highlights the role of inflammation and oxidative stress in neonatal sepsis on gut microbial profiles.
Similar content being viewed by others
Introduction
Early microbial gut colonization after birth strongly influences the maturation of the immune system1,2. The establishment of different bacterial populations will depend on maternal health status, antibiotic treatment, type of birth, but also from gestational age and the type of feeding3,4. Conditions causing alteration of the microbial balance in the neonatal period could expand their negative influence into later periods of life5.
Diseases of inflammatory nature have been directly associated to specific microbial signatures or with dysbiosis and conversely changes in the composition of the gut microbiota may have effects on the host and contribute to the development of diseases that involve inflammatory disorders6,7,8,9. Furthermore, the existence of a crosstalk between gut microbiota and the brain mediated by specific signaling pathways has been established10,11,12,13.
Sepsis is an extremely severe condition in the neonatal period. In preterm infants, the incidence ranges between 2% for vertical sepsis (mother-transmitted) and 20% for nosocomial (hospital-acquired) sepsis. Overall mortality is close to 18%14. Moreover, many survivors will suffer from neurodevelopmental and sensorial sequels15. Signs and symptoms of neonatal sepsis are extremely subtle rendering clinical diagnosis very difficult16,17,18. The etiologic diagnosis is based upon the isolation of a microorganism in the blood culture. Coagulase-negative staphylococci (CONS) followed by gram-negative bacteria are the most frequently identified pathogens14. However, blood culture frequently yields negative results due to low degree bacteremia, small inoculation volumes, and/or antibiotics supplied to the mother during labor19,20,21. Remarkably, sepsis affects gut homeostasis and consequently the gut microbiota. Moreover, following a septic process preterm infants exhibit a distorted microbiome with predominance of Staphylococcus species and reduced diversity with no specific enrichment of potential pathogens22,23.
Genome-wide expression profiles can discriminate septic from non-septic preterm infants in the neonatal period24. Gene expression analysis of exfoliated intestinal cells (EIC) and the transcriptional information obtained could disclose non-invasively relevant information about the biologic situation of the intestinal epithelial tissue16. However, studies of gene expression in EIC and microbiota in septic preterm infants have not been yet conducted.
The aim of the present study was to get an insight into the processes taking place in the gut of preterm infants during sepsis compared to their non-septic twins searching for possible relationships between changes in the gut microbiota and gene expression of EIC.
Results
Population
Five pairs of preterm twins (≈30 weeks’ gestation) were enrolled. Each pair included one twin who developed sepsis and a non-septic control. No other differences were observed between cases and controls (Table 1). Two of the neonates with sepsis had a positive blood culture test. The causal agent was identified as coagulase-negative Staphylococcus strain.
Transcriptomic analysis of exfoliated epithelial cells
Total RNA from the fecal samples of the infants was hybridized with whole human genome microarrays (28,000 annotated genes). Three-dimensional unsupervised principal component analysis (PCA) showed two clustered groups that included the septic and non-septic control samples (Fig. 1a). Further analysis yielded 819 differentially expressed probe sets (ANOVA, p-value < 0.05) between septic and non-septic infants (Tables S1 and S2). Only 510 annotated genes were considered from which 343 genes were up-regulated and 167 were down-regulated. The unsupervised hierarchical clustering showed sensitive differences in gene expression between septic infants and non-septic controls (Fig. 1b). Table 2A shows the most up and down-regulated genes in both groups. Proteins encoded in the list reflect certain degree of inflammation and infiltration of immune cells in the gut mucosa (fecal up-regulation of CD40LG during sepsis). These data are in agreement with gene expression in peripheral blood cells of preterm infants with sepsis24 (Table 2B).
(Panel a) Principal component analysis (PCA) of the gene expression profiles of exfoliated intestinal cells of septic preterm twins (in red) and their non-septic controls (in green). The 3D plot shows the correlation of each sample with respect to the first three principal components. (Panel b) Represents the unsupervised hierarchical cluster analysis. Significantly regulated genes (p < 0.05) were used for 2-D hierarchical clustering of sepsis and control samples. Each row represents the expression of an individual probe set and each column of an individual sample, summarizing control samples with a green bar and sepsis samples with a red bar. Upregulated genes are represented in red and downregulated genes in blue.
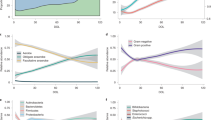
Functional annotations, upstream regulators and signaling pathways
According to Pathway Studio (PS) most of the induced gene expression changes were related to regulation of transcription (Table 3A). The most significant were DNA-dependent regulation of transcription (P = 2.53E-08) representing typical interaction modules with DNA and RNA (Table S3), and HDAC2 encoding for histone acetylase 225. The annotation term metabolic process entailed a large number of genes encoding different enzymes involved in ATB-binding (Table S3) and oxidative stress ((glutathione peroxidase 1 (GPX1); glutathione S-transferase mu2 (GSTM2))26,27.
Further, protein-protein networks and signaling pathways could be inferred from expression data. Annotated genes showing significant up- and down-regulation with greater fold changes (FC > 2 and FC < −2) were selected for the PS analysis. They revealed interaction pathway related to Oxidative Stress (Fig. 2, Panel a) and its connection to the canonical NF-κB inflammatory pathway (Fig. 2, Panel b). Upstream regulator analysis (Table 3B) identified FOXN4 and SP1 as most significant transcription regulators.
Ingenuity Pathway Analysis (IPA) provided a functional analysis with gene Networks conceptually complementary to the biological processes and master regulators described above (Table 3C). The most significant interaction network related a collection of genes to the molecular functions Cell Death and Survival, Cancer and Inflammatory Response (Fig. 3, Panel a). In agreement with PS, using the upstream regulator analysis tool of the IPA software a contribution to regulatory role could be again attributed to IL1-β, which predicts IL1-β to be activated as transcriptional regulator (z-score 2.368), although, due to the low number of activated genes in the pathway there was a low significance score (P = 0.18) (Fig. 3, Panel b).
IPA analysis: (Panel a) Top Network Cell Death and Survival, Inflammatory Response, Cancer. (Panel b) Upstream regulation: evidence of the activation of IL1B pathway. IL1B predicted to be activated (z-score 2.368) p-value = 1.84E-01: 6 out of 6 genes have expression direction consistent with activation of IL1B.
Microbial diversity and composition determined by molecular methods
A primary analysis of the main bacterial groups performed by qPCR of 16S rDNA showed differences between septic and control twins (Fig. 4a). Healthy controls exhibited higher amounts and prevalence of Bifidobacterium species (P = 0.050 and P = 0.055, respectively) and lower levels of Enterobacteriaceae (P = 0.093). Although Enterobacteriaceae, Enterococcus and Staphylococcus groups were common in the septic group, prevalence had low significance scores (P > 0.05).
(Panel a) Relative abundance of bacterial distribution at class level in the Sepsis and Control groups. (Panel b) Rarefaction curves at level of 90% for families. The graphs shows rarefaction curve relating the sequencing effect compared with an estimate of the number of bacterial families, as inferred by the number of OTUs.
By pyrosequencing, we obtained an average of 10.265,5 (SD ± 4957.04) sequences per infant sample. The average length per sequence was 425 nucleotides (range 300–455). Table S4 shows the predominant phyla present in all samples. Thus while Lactobacillales and Enterobacteriales showed higher frequency in septic patients Bacillales were lower. Pseudomonadales and Vibrionales were found only in the septic group.
At family level, Enterobacteriaceae proportions were higher (72.2% vs. 30.4%, respectively) and Bacteroides were lower in sepsis (18.6% vs. 21.7%, p-value = 0.192) than in controls. A greater proportion of Enterococcaceae was found in sepsis (5.5%) than in the control group (<0.1%). We found a significantly higher percentage of Staphylococcaceae sequences in control (4.2%) than in sepsis cases (<1%); however, proportions were low.
We observed that the septic group showed higher bacterial diversity than the control group although differences were not significant (Fig. 4b). Moreover, taxons of twin neonates suffering sepsis included predominantly aerobic or aerotolerant species with a decrease of strict anaerobes.
Associations between microbes and neonatal intestinal gene expression
First we analyzed both the sets of genes involved in inflammation and oxidative stress (except SLC19A1 and OR2H2) to establish a correlation between these and the most prominent bacterial clades in septic patients (Fig. 2). Pearson’s correlation of the expression of oxidative stress-related genes with significant clades revealed a significant inverse correlation between the order Bacteroidales, family Bacteroidaceae and genus Bacteroides and 8 of 21 genes in the oxidative stress pathway (11 of 21 genes if we include “Other Bacteroidales”) (Fig. 5a, Table S5A). Results were confirmed with data obtained by qPCR, as a significant inverse correlation with the Bacteroides/Prevotella group was confirmed with 4 of 21 genes. Interestingly, qPCR data also indicated a significant inverse correlation between the calculated reads of the genus Bifidobacterium and the expression of oxidative stress genes (8 of 21) (Fig. 5b, Table S5A). Both genera Bifidobacterium and Bacteroides include strict anaerobic species. Other bacterial groups decreased significantly when signal transduction pathways controlled by the master regulator NF-κB were active such as the order Mycoplasmatales and the genus Staphylococcus with significant correlation with 6 and 5 genes respectively out of 15 (Fig. 5b, Table S5B). Enterobacteria counts obtained by qPCR directly correlated with a moderate activation of the NF-κB and IL-1β pathways (6 and 5 of 15 genes, respectively).
Depicts the colored representation of the correlation between bacterial groups (reads of pyrosequencing of numbers estimated by qPCR) and expression (signal intensity) of the differentially expressed genes in the Oxidative Stress pathway (panel a) and in the NF-κB pathway and IL-1β pathways (panel b). Red represents significant inverse correlation and blue cells’ significant direct correlation. Genes with white cells gave no significant correlation with the corresponding bacterial taxon and genes not shown had no significant correlation with any bacterial taxa.
Discussion
The analysis of intestinal cells and gut microbiota in the present study offers an integrative perspective of the events occurring in the gut of preterm infants during sepsis considering that inter-individual differences were minimized by the selection of dizygotic twin pairs with and without sepsis. Gene expression differences between septic and non-septic infants were moderate, between 2 and −2, because EIC integrate pools of various types of cells –epithelial cells, lymphocytes- at different physiological conditions, including anoikis. Despite this variability, our data demonstrated that EIC from septic patients significantly expressed more genes bound to inflammatory pathways and oxidative stress than non-septic controls. Of note, none of the analysis performed showed significant differences between culture positive samples and those with clinical diagnostic.
Some pro-inflammatory genes were up-regulated in EIC revealing the implication of inflammatory regulators; however, these genes do not participate in canonical responses to gut bacteria as pathogen-associated molecular patterns. The infiltration of lymphocytes in feces may partially explain finding of just some differentially expressed genes in exfoliated cells similar to those reported in blood of septic preterm infants24 (Table 2) as expected in the case of inflammatory organ crosstalk. Genes showing a similar trend in EIC and peripheral blood – like OSCAR, ARID5A SMYD2 and CD3e- may probably reveal the presence of circulating immune cells in feces. OSCAR encodes a collagen receptor that in monocytes and neutrophils plays a role in the release of pro-inflammatory cytokines and oxidative stress mediators28. ARID5A contributes to the stabilization of the mRNA encoding the pro-inflammatory cytokine IL-629,30. SMYD2 encodes a mono-methyl-transferase that methylates acceptor lysine residues on histones31,32 and other proteins like tumor suppressor proteins p53 and pRb relevant to tumor progression and/or undetermined epigenetic events33,34,35. Finally, CD3E down-regulation may indicate that antigen recognition may be uncoupled during sepsis in CD4+ T lymphocytes and T-cells36.
Functional annotation analysis offered intriguing clues on possible connections to epigenetic modifications. In septic infants we found activated biological processes like gene transcription that involved down-regulation of HDAC2 a histone acetylase34,35 and PARP137 but also up-regulation of SMYD2 that methylates histones31,32, and DNA methyltransferase associated protein (DMAP1). Histone deacetylases can modulate gene expression through endogenous factors, but also through dietary components, synthetic inhibitors, and bacteria-derived signals38,39, thereby underlining the mutualistic relationship that exists between gut microbiota and host.
The finding of active oxidative stress pathways in exfoliated cells led us to reanalyze data obtained from peripheral blood cells of VLBW infants, and we found significant values for the oxidative stress pathway (p = 0.0015) that involved the genes BCL2, LCN2, MMP9, EPAS1, BTG1, TOR1 and VNN124. The activation of the oxidative pathways in gut cells could be initiated by the circulating inflammatory mediators or by reactive oxygen (ROS) or nitrogen (RNS) species secreted by blood lymphocytes40. Metabolomic analysis has shown that sepsis in the neonatal period is associated to an increase in oxidative stress biomarkers41. ROS and RNS intermediates are powerful antimicrobials and major components of the innate defense frontline; however, beyond a threshold they have deleterious effects. Remarkably, oxidative stress has been related to changes in the microbial patterns in the gut42,43. Thus, we have observed a decrease of strict anaerobes (Bacteroides, Bifidobacterium) in the septic group, followed by the proliferation of aerobes (Enterobacteriaceae). The genera belonging to this family include species equipped with specialized enzymes such as tetrathionate reductase44 and other versatile cytochrome related enzymes that allow the use of ROS-oxidized molecules as electron acceptors45. Other bacterial groups found in the sepsis samples can reduce nitrate and nitrite to NO, or have catalase or pseudo-catalase enzymes46. Altogether these properties would grant them competitive advantage. A general model can be inferred in septic preterm infants that would allow understanding of the likely relationship between blood lymphocyte inflammatory signals during sepsis, with expression of inflammatory and oxidative stress genes, as well as changes in the gut microbiota (Fig. 6). In blood cells, master regulators induce canonical inflammatory pathways24 and oxidative stress elicited by bacterial septic invasion, leading to the secretion of abundant pro-inflammatory cytokines. Through inflammatory organ crosstalk that led to low but significant expression of inflammatory networks and oxidative stress genes in the gut mucosa –exfoliated epithelial cells- that drives the secretion of ROS and NOS to the lumen, hence affecting the viability of sensitive bacterial species, like Bacteroides and Bifidobacterium species.
Circulating lymphocytes expressed high levels of inflammatory markers (TNF-α, NF-κB, IL-1β and SP1). High amounts of innate immune mediators secreted to the bloodstream would be reaching the mucosae of the small and large intestine of VLBW infants with sepsis. This would activate master regulators TNF-α and IL-1β, inducing the expression of pro-inflammatory signaling and innate immune defense systems, such as oxidative stress pathway in the gut mucosal cells. The secretion of ROS and NOS would then correlate with bacterial profiles richer in Enterobacteriaceae and with the lower presence of Bifidobacteriaceae and Bacteroides, due to the lack in the latter of the enzymatic armor to survive in the presence of ROS, RNS and derived toxic compounds.
To summarize, this pilot study shows that sepsis in preterm infants induces inflammation in the gut mucosa and changes in gut microbiota extending inflammation-associated damage to sensitive organs. Our results also support the relevance of oxidative stress in sepsis, which may cause the reduction of Bifidobacterium spp. and other beneficial anaerobes in the gut lumen. These data will open new possibilities to reduce the neonatal sepsis using the knowledge and potential role of human breast milk acting as a “gut protector” and antioxidant47.
Methods
Patients and Design
We conducted a prospective, observational, cohort study in the NICU of the University and Polytechnic Hospital La Fe from April 2011 to September 2012. Eligible patients were twin pairs with a birth weight ≤ 1.500 g. When one of the twins exhibited clinical signs of sepsis, the other was simultaneously recruited as control if lacking signs of sepsis to homogenize the genetic background. Sepsis was considered clinical signs such as the presence of 3 or more of the following: (i) temperature instability (rectal temp. >38 °C or <36 °C); (ii) respiratory symptoms (respiratory distress, apnoea or cyanosis);
(iii) cardiovascular symptoms: hypotension (blood pressure <5th percentile for age), tachycardia (HR > 0180/min), bradycardia (HR < 100/min) or poor perfusion;
(iv) neurological symptoms: clinical or electrical seizures, hypotonia or lethargy; and (v) gastrointestinal symptoms: vomiting, poor feeding or feeding intolerance and/or
abdominal distension, without identification of a bacterial pathogen from a sterile site. Exclusion criteria were: maternal immunodeficiency; Apgar 0 at 1 min; chromosomal abnormalities or major gastro-intestinal malformation; congenital infection; concomitant diagnosis of necrotizing enterocolitis.
The clinical interventions included in the study protocol were designed according to the Clinical Guidelines approved by the Spanish Neonatal Society (SENeo) and the Ethical Guidelines of the Comité de Ética e Investigación Médica (CEIM) of the Health Research Institute La Fe. The study protocol was approved by the CEIM. The inform consent was signed by parents of all the enrolled patients.
Diagnosis of sepsis
A standard blood culture was performed (BacT/Alert® PF; Biomérieux®, Durham, NC; USA) only in patients with suspected sepsis. Microbiologic positive diagnosis was considered when a microorganism was isolated from blood culture together with clinical signs and risk factors48. Two positive blood cultures were required to diagnose CONS sepsis. Cultures obtained from other sterile sites were not considered for diagnosis of sepsis.
Samples
Stool samples from both twins were collected immediately after sepsis was suspected. Samples were frozen and stored at −80 °C for later analysis.
RNA extraction and cDNA microarray analysis
Total RNA of EIC was isolated from fecal samples using the Trizol reagent (TRIzol, Invitrogen.), followed by an polyA+ RNA enrichment step in order to eliminate contaminating DNA and bacterial RNA using the mRNA-ONLY™ Eukaryotic mRNA Isolation Kit (Epicentre) according to the manufacturers´ instructions. RNA integrity was assessed using the Agilent 2100 Bioanalyzer (Agilent, Palo Alto, CA, USA). Hybridization was performed if the RNA integrity number was ≥7.
Microarray experiments were performed at the Central Research Unit (University of Valencia) using GeneChip Human Gene 1.0 ST Array (Affymetrix®, Santa Clara, CA, USA) following the manufacturer’s protocol. The files obtained (.CEL) were used to analyze significant changes in gene expression profiles using Partek Genomic Suite 6.6 (Partek Inc., St. Louis, MO, USA). Data were normalized using robust multiple-array average (RMA) algorithm. Principal Component Analysis (PCA) determined global transcriptome differences between samples. Next, 1-way ANOVA (p-value < 0.05) was applied to identify significantly different expressed genes between bacterial sepsis and control groups, and were ordered according to their expression levels in an unsupervised hierarchical clustering. To obtain insights about the pathways, biological processes and molecular functions differentially expressed in the sepsis group were investigated through functional annotation analysis with specialized computer packages Pathway Studio 9 (Ariadne Genomics® software, Elsevier® Inc, Rockville, MD, USA) and Ingenuity Pathway Analysis (Qiagen, Redwood City, CA, USA) that are based on different algorithms and concept definitions and would offer a wider perspective49.
DNA extraction and microbial composition by quantitative PCR (qPCR)
DNA was extracted from 200–300 mg fecal samples using a modified Qiagen stool DNA extraction kit (QIAgen, Hilden, Germany), and qPCR amplification and detection were performed in a LightCycler® 480 Real-Time PCR System (Roche) as previously described50. The bacterial concentration in each sample was calculated by comparing the Ct values obtained from standard curves. These were created using serial 10-fold dilution of pure culture-specific DNA fragments corresponding to 10 to 109 number of gene copies/ml. For statistical analysis, SPSS 15.0 (SPSS Inc, Chicago, IL) software was used. Due to non-normal distribution, microbial data are expressed as medians with interquartile ranges (IQR). The Kruskall-Wallis test was used to compare data of more than two groups of babies, while Mann-Whitney U test was used for comparing data of two groups. The χ-square test was used to establish differences in the prevalence of bacteria between the groups. A p < 0.050 was considered statistically significant. The possible correlation between variables was studied by applying the Pearson correlation coefficient and significance was established at 0.5%.
Microbial diversity and composition estimated by pyrosequencing total 16S rRNA genes in feces
A barcoded primer set based on universal primers 27F and 533R was used to amplify 500 bps of the 16S rRNA genes encompassing the V1-V3 region. PCR was carried out using a high-fidelity KAPA-HiFi polymerase (Kappa Biosystems, US) with an annealing temperature of 52 °C and 30 cycles. Amplicons were checked and measured using the Agilent High Sensitivity DNA assay in Agilent 2100 Expert. Purified PCR products were pyrosequenced from the forward primer end only using a GS-Junior sequencer with Titanium chemistry (Roche) at the Scientific Platform unit SCSIE (University of Valencia, Spain).
From the resulting raw data set, low quality sequences or sequences with a length less than 150 nucleotides were discarded and also, chimeric sequences were removed. The QIIME pipeline (version 1.8.0 and green genes data base 13_5) was used for identifying representative sequences for each operational taxonomic unit (OTU) generated from complete linkage clustering with a 97% similarity. Alpha diversity indices were determined from rarefied tables using the Shannon-Wiener index for diversity and the Chao1 index for species richness; Observed Species (number of unique OTUs) and Phylogenetic Distance (PD_whole) were also determined. An OTU was a cluster of 16S rRNA sequences that were >95% identical, a conservative estimate for the boundary between species, established at 97% (species) and 95% (genus) for full-length 16S gene sequences. A beta diversity distance matrix was computed from the previously constructed OTU table using UniFrac analysis. Unweighted (presence/absence matrix) and weighted (presence/absence/abundance matrix) UniFrac distances were used to construct two- and three-dimensional Principal Coordinates Analysis (PCoA) plots. Biplots were generated as part of the beta diversity analysis in QIIME, using genus level OTU tables showing principle coordinate sample clustering alongside weighted taxonomic group data. Data on assigned sequences at genus level shared between samples were used to generate a Venn diagram51,52,53,54,55,56,57,58,59,60.
Additional Information
How to cite this article: Cernada, M. et al. Sepsis in preterm infants causes alterations in mucosal gene expression and microbiota profiles compared to non-septic twins. Sci. Rep. 6, 25497; doi: 10.1038/srep25497 (2016).
References
Collado, M. C., Cernada, M., Bauerl, C., Vento, M. & Perez-Martinez, G. Microbial ecology and host-microbiota interactions during early life stages. Gut Microbes 3, 352–65 (2012).
Zeissig, S. & Blumberg, R. S. Life at the beginning: perturbation of the microbiota by antibiotics in early life and its role in health and disease. Nat Immunol 15, 307–10 (2014).
La Rosa, P. S. et al. Patterned progression of bacterial populations in the premature infant gut. Proc Nat Acad Sci (PNAS) 111, 12522–7 (2014).
Cabrera-Rubio, R. et al. The human milk microbiome changes over lactation and is shaped by maternal weight and mode of delivery. Am J Clin Nutr 96, 544–51 (2012).
De Vos, W. M. & De Vos, E. A. J. Role of the intestinal microbiome in health and disease: from correlation to causation. Nutr Rev 70, S45–S56 (2012).
Gruber, L., Lichti, P., Rath, E. & Haller, D. Nutrigenomics and nutrigenetics in inflammatory bowel diseases. J Clin Gastroenterol 46, 735–47 (2012).
Kelly, D. & Mulder, I. E. Microbiome and immunological interactions. Nutr Rev 70, 1753–4887 (2012).
Blaut, M. & Klaus, S. Intestinal microbiota and obesity. Handb Exp Pharmacol 209, 251–73 (2012).
Tremaroli, V. & Backhed, F. Functional interactions between the gut microbiota and host metabolism. Nature 489, 242–9 (2012).
Heijtz, R. D. et al. Normal gut microbiota modulates brain development and behavior. Proc Nat Acad Sci (PNAS) 108, 3047–52 (2011).
Clarke, G. et al. The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol Psychiatry 18, 666–73 (2013).
Bercik, P. et al. The anxiolytic effect of Bifidobacterium longum NCC3001 involves vagal pathways for gut–brain communication. Neurogastroenterol Motil 23, 1132–9 (2011).
Bravo, J. A. et al. Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Nat Acad Sci (PNAS) 108, 16050–5 (2011).
Stoll, B. J. et al. Late-Onset Sepsis in Very Low Birth Weight Neonates: The Experience of the NICHD Neonatal Research Network. Pediatrics 110, 285–91 (2002).
Mitha, A. et al. Neonatal Infection and 5-year Neurodevelopmental Outcome of Very Preterm Infants. Pediatrics 132, e372–e80 (2013).
Cornell, T. T., Wynn, J., Shanley, T. P., Wheeler, D. S. & Wong, H. R. Mechanisms and Regulation of the Gene-Expression Response to Sepsis. Pediatrics 125, 1248–58 (2010).
Tang, B., Huang, S. & McLean, A. Genome-wide transcription profiling of human sepsis: a systematic review. Crit Care 14, 1–11 (2010).
Tang, B. M. P., McLean, A. S., Dawes, I. W., Huang, S. J. & Lin, R. C. Y. The Use of Gene-Expression Profiling to Identify Candidate Genes in Human Sepsis. American Journal of Respiratory and Crit Care Med 176, 676–84 (2007).
Chiesa, C., Panero, A., Osborn, J. F., Simonetti, A. F. & Pacifico, L. Diagnosis of neonatal sepsis: a clinical and laboratory challenge. Clin Chem 50, 279–87 (2004).
Kumar, Y., Qunibi, M., Neal, T. J. & Yoxall, C. W. Time to positivity of neonatal blood cultures. Arch Dis Child Fetal Neonatal Ed 85, F182–6 (2001).
Towers, C. V., Carr, M. H., Padilla, G. & Asrat, T. Potential consequences of widespread antepartal use of ampicillin. Am J Obstet Gynecol 179, 879–83 (1998).
Madan, J. C. et al. Gut microbial colonisation in premature neonates predicts neonatal sepsis. Arch Dis Child Fetal Neonatal Ed 97, F456–F62 (2012).
Mai, V. et al. Distortions in Development of Intestinal Microbiota Associated with Late Onset Sepsis in Preterm Infants. PLoS ONE 8, e52876 (2013).
Cernada, M. et al. Genome-Wide Expression Profiles in Very Low Birth Weight Infants With Neonatal Sepsis. Pediatrics 133, e1203–11 (2014).
Goldstein, B., Giroir, B. & Randolph, A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediat Crit Care Med 6, 2–8 (2005).
Bäuerl, C. et al. Lactobacillus paracasei and Lactobacillus plantarum strains downregulate proinflammatory genes in an ex vivo system of cultured human colonic mucosa. Genes Nutr 8, 165–80 (2013).
Collado, M. C., Laitinen, K., Salminen, S. & Isolauri, E. Maternal weight and excessive weight gain during pregnancy modify the immunomodulatory potential of breast milk. Pediatr Res 72, 77–85 (2012).
Futosi, K., Fodor, S. & Mócsai, A. Neutrophil cell surface receptors and their intracellular signal transduction pathways. Int Immunopharmacol 17, 638–50 (2013).
Masuda, K. et al. Arid5a controls IL-6 mRNA stability, which contributes to elevation of IL-6 level in vivo . Proc Nat Acad Sci (PNAS) 110, 9409–14 (2013).
Saito, Y. et al. AT-Rich–Interactive Domain–Containing Protein 5A Functions as a Negative Regulator of Retinoic Acid Receptor–Related Orphan Nuclear Receptor γt–Induced Th17 Cell Differentiation. Arthritis Rheumatol 66, 1185–94 (2014).
Abu-Farha, M. et al. The Tale of Two Domains: Proteomics and Genomics Analysis of SMYD2, A New Histone Methyltransferase. Mol Cell Proteomics 7, 560–72 (2008).
Graves, T., Harr, M., Crawford, E. & Willey, J. Stable low-level expression of p21WAF1/CIP1 in A549 human bronchogenic carcinoma cell line-derived clones down-regulates E2F1 mRNA and restores cell proliferation control. Mol Cancer 5, 1 (2006).
Wu, J. et al. Biochemical Characterization of Human SET and MYND Domain-Containing Protein 2 Methyltransferase. Biochemistry 50, 6488–97 (2011).
Blackledge, N. P. & Klose, R. J. Histone lysine methylation: an epigenetic modification? Epigenomics 2, 151–61 (2010).
Huang, C., Xu, M. & Zhu, B. Epigenetic inheritance mediated by histone lysine methylation: maintaining transcriptional states without the precise restoration of marks? Phil Trans R Soc Lond B Biol Sci 368, 20110332 (2013).
Bello, R., Feito, M. J., Ojeda, G., Portolés, P. & Rojo, J. M. Loss of N-terminal Charged Residues of Mouse CD3ϵ Chains Generates Isoforms Modulating Antigen T Cell Receptor-mediated Signals and T Cell Receptor-CD3 Interactions. J Biol Chem 282, 22324–34 (2007).
Beck, C., Robert, I., Reina-San-Martin, B., Schreiber, V. & Dantzer, F. Poly(ADP-ribose) polymerases in double-strand break repair: Focus on PARP1, PARP2 and PARP3. Exp Cell Res 329, 18–25 (2014).
Brigelius-Flohe, R. & Maiorino, M. Glutathione peroxidases. Biochim Biophys Acta 1830, 3289–303 (2012).
Baez, S., Segura-Aguilar, J., Widersten, M., Johansson, A. S. & Mannervik, B. Glutathione transferases catalyse the detoxication of oxidized metabolites (o-quinones) of catecholamines and may serve as an antioxidant system preventing degenerative cellular processes. Biochem J 324, 25–8 (1997).
Rittirsch, D., Flierl, M. A. & Ward, P. A. Harmful molecular mechanisms in sepsis. Nat Rev Immunol 8, 776–87 (2008).
Chapkin, R. S. et al. Noninvasive stool-based detection of infant gastrointestinal development using gene expression profiles from exfoliated epithelial cells. Am J Physiol Gastrointest Liver Physiol 298, G582–9 (2010).
Schwartz, S. et al. A metagenomic study of diet-dependent interaction between gut microbiota and host in infants reveals differences in immune response. Genome Biol 13, r32 (2012).
Donovan, S. M. et al. Noninvasive molecular fingerprinting of host–microbiome interactions in neonates. FEBS Letters 588, 4112–9 (2014).
Knight, J. M. et al. Non-invasive analysis of intestinal development in preterm and term infants using RNA-Sequencing. Sci Rep 4, 5453 (2014).
Cavaillon J. M. & Annane D. Invited review: Compartmentalization of the inflammatory response in sepsis and SIRS. J Endotox Res 12, 151–70 (2006).
Beck, C., Robert, I., Reina-San-Martin, B., Schreiber, V. & Dantzer, F. Poly(ADP-ribose) polymerases in double-strand break repair: Focus on PARP1, PARP2 and PARP3. Exp Cell Res 329, 18–25 (2014).
Alenghat, T. et al. Histone deacetylase 3 coordinates commensal-bacteria-dependent intestinal homeostasis. Nature 504, 153–7 (2013).
Kim, G., Gocevski, G., Wu, C. & Yang, X. Dietary, metabolic, and potentially environmental modulation of the lysine acetylation machinery. Int J Cell Biol 2010, 632739 (2010).
Fanos, V. et al. Urinary 1H-NMR and GC-MS metabolomics predicts early and late onset neonatal sepsis. Early Hum Dev 90, Supplement 1, S78–S83 (2014).
Flohé, L., Brigelius-Flohé, R., Saliou, C., Traber, M. G. & Packer, L. Redox Regulation of NF-kappa B Activation. Free Radic Biol Med 22, 1115–26 (1997).
Bogdan, C., Röllinghoff, M. & Diefenbach, A. Reactive oxygen and reactive nitrogen intermediates in innate and specific immunity. Curr Opin Immunol 12, 64–76 (2000).
Gostner, J. M., Becker, K., Fuchs, D. & Sucher, R. Redox regulation of the immune response. Redox Report 18, 88–94 (2013).
Jones, R. M. et al. Symbiotic lactobacilli stimulate gut epithelial proliferation via Nox‐mediated generation of reactive oxygen species. EMBO J 32, 3017–28 (2013).
Espey, M. G. Role of oxygen gradients in shaping redox relationships between the human intestine and its microbiota. Free Radic Biol Med 55, 130–40 (2013).
Hensel, M., Hinsley, A. P., Nikolaus, T., Sawers, G. & Berks, B. C. The genetic basis of tetrathionate respiration in Salmonella typhimurium. Mol Microbiol 32, 275–87 (1999).
Macdonald, J., Galley, H. F. & Webster, N. R. Oxidative stress and gene expression in sepsis. Brit J Anaesth 90, 221–32 (2003).
Winter, S. E. et al. Host-Derived Nitrate Boosts Growth of E. coli in the Inflamed Gut. Science 339, 708–11 (2013).
Sobko, T. et al. Gastrointestinal bacteria generate nitric oxide from nitrate and nitrite. Nitric Oxide 13, 272–8 (2005).
Langhorst, J. & Choi K.-E. The role of human defensins in gastrointestinal diseases. Expert Rev Clin Immunol 7, 779–87 (2011).
Ledo, A. et al. Human milk enhances antioxidant defenses against hydroxyl radical aggression in preterm infants. Am J Clin Nutr 89, 210–5 (2009).
Acknowledgements
M.C. acknowledges a Research Grant Fellowship “Rio Hortega” and M.V. a RD12/0022/0012 (Red SAMID) and FIS PI14/0443 grants from the Instituto Carlos III (Spanish Ministry of Economy and Competitiveness) and Fondos FEDER from the European Union. C.B., M.C.C. and G.P.M. acknowledge the grant AGL2013-47420-R and by the Fun-C-Food CSD2007-00063 project from the Consolider-Ingenio program, both from the Spanish Ministry of Science and Innovation.
Author information
Authors and Affiliations
Contributions
M.C. and M.V. conceived the study, designed the experiments and supervised all research. E.S. supervised and performed the genomic studies. C.B., M.C.C. and G.P.M. designed the microbial experiments and performed the microbial studies. M.C. and G.P.M. prepared the draft of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Cernada, M., Bäuerl, C., Serna, E. et al. Sepsis in preterm infants causes alterations in mucosal gene expression and microbiota profiles compared to non-septic twins. Sci Rep 6, 25497 (2016). https://doi.org/10.1038/srep25497
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep25497
This article is cited by
-
Modulation of intestinal TLR4 expression in infants with neonatal opioid withdrawal syndrome
Journal of Perinatology (2023)
-
The infant gut microbiome as a microbial organ influencing host well-being
Italian Journal of Pediatrics (2020)
-
The gut microbiome’s role in the development, maintenance, and outcomes of sepsis
Critical Care (2020)
-
Immunometabolic approaches to prevent, detect, and treat neonatal sepsis
Pediatric Research (2020)
-
Urine metabolomics in neonates with late-onset sepsis in a case-control study
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.