Abstract
Novel Staphylococcus aureus clones continue to emerge that cause infections in otherwise healthy people. One example is the sequence type (ST) 398 lineage, which we show here is increasing in importance as a significant cause of community-associated (CA) human infections in China. We have a profound lack of understanding about what determines the considerable virulence potential of such newly emerging clones. Information about the contribution to virulence of the more recently discovered ESAT-6 secretion system (ESS) has remained particularly scarce. The Chinese ST398 isolates exhibited significantly increased expression of ESS genes as compared to predominant hospital-associated clones, which we found is likely due to increased expression of the accessory gene regulator (Agr) system and control of ESS by Agr. Importantly, deletion of essB in ST398 resulted in significantly reduced resistance to neutrophil killing and decreased virulence in murine skin and blood infection models. Our results demonstrate a key function of ESS in promoting virulence and mechanisms of resistance to innate host defense in an important emerging CA-S. aureus lineage. They suggest that ESS has a so far underestimated role in promoting aggressive virulence and epidemiological success of S. aureus.
Similar content being viewed by others
Introduction
Staphylococcus aureus is an important pathogen that causes a variety of infections, ranging from localized skin and soft-tissue infections (SSTIs) to life-threatening severe infections such as necrotizing pneumonia or sepsis1. There are reports indicating that hospital-associated infections due to methicillin-resistant S. aureus (MRSA) are decreasing, at least in the U.S. and Western Europe2,3. On the other hand, the considerable morbidity and mortality that is due to community-associated infections, caused by both methicillin-resistant and methicillin-sensitive S. aureus isolates, is increasing on a worldwide scale2,4,5,6.
By contrast with hospital-associated S. aureus (HA-SA) infections, for which there are predisposing risk factors, community-associated S. aureus (CA-SA) infections can occur in otherwise healthy individuals, suggesting that these bacterial strains have greater virulence than HA-SA strains7. In China, HA-SA has been extensively studied during the past years with ST239 and ST5 MRSA as the predominant clones. In comparison, data on CA-SA in China are still limited, but studies in children suggest predominance of isolates belonging to sequence type (ST) 598.
The ST398 lineage was originally described in livestock and sporadically causes infections in humans working in close proximity to animals9,10. However, in the Americas, it is now also recognized as a causative agent of infections in humans living in animal-free environments11. Whole genome sequencing of human CA-SA ST398 revealed that it represents a human-adapted lineage that is different in genetic composition from animal-associated ST398 clones11. The molecular processes underlying the capacity of CA-SA ST398 to infect healthy individuals and spread sustainably in the population are poorly understood, but recent results obtained with ST398 isolates from Brazil that caused fatal pneumonia indicate an important role of Agr-controlled toxins, in particular α-toxin, in ST398 virulence12.
The ESAT-6 secretion system (ESS), originally described in Mycobacterium tuberculosis, has recently been discovered in S. aureus13. While there are strain-dependent differences, the system includes as core genes the esaA, esaB, essA, essB, essC, esxA and esxB genes14. The Ess proteins are membrane-located components of the secretion machinery, EsaB is a regulator, and the EsxA, EsxB, and EsaC are exported effector proteins13,14,15. Mutants in esxA, esxB, and essC have been shown to contribute to abscess formation in S. aureus Newman13. Furthermore, the ESS has also been shown to impact nasal colonization and pneumonia, albeit in a strain-dependent fashion14. The mechanistic function in pathogenesis of secreted ESS substrates is poorly understood, but results from a recent study indicate a role of EsxA and EsxB in the modulation of apoptosis and release of ingested S. aureus from epithelial cells16.
In the present study, we show that there is a considerable increase of CA-SA infections in China that are due to ST398 and demonstrate increased virulence of CA-SA ST398 as compared to predominant HA-SA strains. We then sought to determine yet unknown factors that contribute to the enhanced virulence potential of CA-SA ST398 and discovered increased expression of ESS factors in ST398 isolates, pointing to a potential key role of ESS in ST398 virulence. By construction and analysis of an essB deletion mutant in ST398, we demonstrate a significant role of ESS in acute ST398 infection, which our results indicate may be due to a previously unrecognized role of ESS in the evasion of destruction by human neutrophils.
Results
Prevalence of CA-SA ST398 is increasing in China
Laboratory-based surveillance in Shanghai teaching hospitals indicated a considerable number of CA infections that were due to ST398 isolates, with the number of cases increasing over time and reaching ~1/3 of all CA infections in 2014 (Fig. 1A, Table 1). During the entire surveyed time frame (2005–2014), the corresponding numbers for HA ST398 cases were extremely low (overall ~1%), suggesting a community origin of the surge in ST398 cases. Data from a pediatric hospital obtained in 2012 painted a similar picture (Table 1). The majority of the CA-SA ST398 isolates belonged to spa types t034 and t571. They were mostly associated with skin, blood, and lung infections (Table 1). The lukSF genes encoding the Panton-Valentine leukocidin (PVL), a leukocidin often epidemiologically associated with CA-MRSA infections17, were present in only 27.5% of CA-SA ST398 isolates from adults and absent from pediatric isolates. The vast majority of CA-SA ST398 isolates (90%) were methicillin-sensitive. Finally, of the patients that could be reached to provide the respective information (42/69), only 3 (7%) reported contact with livestock within the last month, indicating that the surge in ST398 infections in Shanghai did not originate from livestock.
(A) Percentage of CA- and HA-SA infections caused by ST398 among adult patients at Renji hospital, Shanghai. See Table 1 for absolute numbers. (B,C) Mouse abscess model with randomly selected isolates of CA-SA ST398 and HA-SA ST239 obtained from the same hospital and during the same time frame. Analyzed were n = 8 mice/group. Abscess development was measured at day 2 after infection. (C) Representative abscesses. (D) Concentration of TNF-α in the blood of animals at the time of euthanasia. (B,D) ***p < 0.001 (unpaired t-test). The empty circle represents the data corresponding to the isolate selected for genetic deletion.
CA-ST398 is more virulent than HA-ST239
SSTIs are the most frequent type of infections caused by CA-SA6. Therefore, we used a mouse abscess model to compare the virulence of randomly selected clinical CA-SA ST398 with that of randomly selected isolates of ST239, a predominant HA-SA clone in China18. The ST398 isolates were significantly more virulent in the skin infection model compared with the ST239 isolates, inasmuch as the skin lesions of mice infected with ST398 isolates were significantly larger (Fig. 1B,C) and concentrations of the inflammatory cytokine TNF-α in abscess tissue significantly higher (Fig. 1D) than in mice infected with ST239 isolates.
In a previous study, in which we compared the genetic composition of ST398 versus ST239 and ST5 isolates, we only found minor differences in the presence of virulence genes19. Genes for the surface proteins SdrC and SdrE and those encoding PVL were significantly more prevalent, while a series of exotoxin genes were less prevalent in ST398. However, as mentioned above for PVL, these were not sufficiently widespread among ST398 isolates to explain for an overall difference in virulence of the lineage.
CA-SA ST398 isolates show high expression of genes belonging to ESS
Increased expression of Agr-controlled toxins, in particular α-toxin, has recently been made responsible for the high virulence of ST398 isolates that caused fatal pneumonia12. In our previous study19, we showed that Agr (as measured by expression of RNAIII), α-toxin, and phenol-soluble modulins (PSMs) α also showed increased expression in our isolates. In contrast, the non-Agr-regulated exopolysaccharide biosynthesis locus ica20,21 did not show differential expression, and several of the often Agr-down-regulated surface protein genes showed the expected opposite mode of expression19. Here, we analyzed expression of genes belonging to ESS and found that also several of those (essA, essB, essC, esxA) showed significantly increased expression as compared to ST239 isolates (Fig. 2A, Supplementary Fig. S1). We confirmed increased expression of the protein EssB, which is an essential membrane-located component of ESS22, by Western blotting using antiserum developed against a purified glutathion-S-transferase (GST)-EssB fusion protein (Fig. 2B). These results demonstrated enhanced expression of several key ESS genes and proteins in ST398 clinical isolates and suggested that ESS is Agr-regulated in ST398. To directly verify that hypothesis, we constructed an agr mutant of a ST398 isolate and measured expression of ESS genes, which confirmed that ESS is under Agr control in that lineage (Fig. 2C).
(A) Quantitative RT-PCR analysis of essB gene expression in randomly selected clinical CA-SA ST398, HA-SA ST239, and HA-SA ST5 isolates, at 4 and 8 h of in-vitro growth. ****p < 0.0001 (1-way ANOVA with Dunnett’s post-test versus ST398). (B) Production of EssB, Western blot with EssB-specific antibodies. Production of constitutively expressed sortase A (SrtA), measured with specific anti-SrtA antibodies, was used for normalization. Densitometric values of the Western blot signals shown at the right were determined and compared. ****p < 0.0001 (Mann-Whitney). (C) Control of ESS gene expression by Agr, qRT-PCR. *p < 0.05; (Mann-Whitney). Four biological replicates per group were analyzed. The empty circles in (A,B) represent the data corresponding to the isolate selected for genetic deletion.
ESS of ST398 has a significant impact on acute virulence in experimental blood and skin infection
Our results suggest that the observed rise in ST398 infections is due to enhanced virulence of the ST398 isolates and associated with enhanced expression of determinants of acute virulence. Based on our expression analyses, we hypothesized that ESS may represent a previously underestimated component contributing to acute virulence of emerging CA-SA strains such as ST398. To evaluate that hypothesis, we constructed an isogenic gene deletion mutant in essB, an essential component of ESS, in a representative (based on our gene expression and animal virulence data, Figs 1 and 2) ST398 isolate. We then compared the virulence potential of that mutant to that of the isogenic wild-type strain in mouse models of skin infection and bacteremia. In the skin infection model, the wild-type strain caused significantly larger abscesses than the essB mutant strain (Fig. 3A,B). Furthermore, histological examination showed increased infiltration of neutrophils and skin tissue destruction in the mice infected with the wild-type strain (Fig. 3C). In a high-dose (109 CFU) bacteremia model, the mice infected with the wild-type strain died significantly faster than those infected with the essB mutant (Fig. 4A). In a low-dose (108 CFU) bacteremia model, CFU counts in the blood and kidneys of mice 4 days after infection were higher in the mice infected with the wild-type strain than in those infected with the essB mutant strain (Fig. 4B,C). Furthermore, the kidneys of mice infected with the wild-type strain showed increased abscess formation (Fig. 4D). Moreover, histological examination showed more extensive inflammation accompanied by an increased number of infiltrating inflammatory cells in the kidneys of those mice (Fig. 4E). These results showed that ESS is a significant contributor to acute virulence in ST398.
Mouse abscess model with essB deletion mutant versus isogenic wild-type representative ST398 isolate. Number of mice used: n = 11/group. (A) Abscess areas on day 2 after infection. **p < 0.01 (unpaired t-test). (B) Representative abscesses on day 2 after infection. (C) H&E staining of abscess skin tissue harvested on day 4. (–), control without challenge. Note considerable infiltration of inflammatory cells and damage of the subcutaneous structure in the wild-type and essB mutant samples, noticeably stronger in the wild-type sample (arrows).
Mouse bacteremia model with essB deletion mutant versus isogenic wild-type representative ST398 isolate. (A) Survival analysis. Mice were injected with 109 CFU live S. aureus or PBS. Survival curves were compared using a log-rank (Mantel-Cox) test. Number of mice used: n = 11 (wild-type); n = 10 (essB mutant and PBS). (B-D) Mice (n = 10/group) were infected with 108 CFU live S. aureus and euthanized 4 days after injection. CFU in blood (B) and kidneys (C) were assessed by plating on TSB agar. *p < 0.05; **p < 0.01 (unpaired t-tests). For CFU determination, n = 9/group (two mice had to be excluded due to blood coagulation and resulting difficulties in CFU determination). (D,E) Photographs of kidneys (D) and corresponding H&E stained sections harvested from mice 4 days after injection (E). Note formation of macroscopic abscesses in kidneys of mice infected with wild-type and essB mutant strains (D) (arrows), with the abscess being bigger in the wild-type-infected kidney. In (E), note considerable infiltration of inflammatory cells in the wild-type and essB mutant samples, noticeably stronger in the wild-type sample (arrows).
ST398 ESS is responsible for the secretion of EsxA and EsxB
To gain insight into how the ESS of ST398 contributes to virulence, we first analyzed whether it is involved in the secretion of EsxA and EsxB, which have been previously described as virulence factors that are secreted by ESS in other S. aureus strains13. According to LC-MS/MS analysis of ST398 wild-type versus essB deletion mutant culture filtrates, EsxA and EsxB are secreted in ST398 in an ESS-dependent fashion (Fig. 5). Then, to rule out that the impact of ESS on ST398 virulence is mediated by a regulatory influence on major toxins and toxin regulators previously associated with ST398 virulence, we measured expression of hla, psmα, and Agr in the essB mutant versus the wild-type ST398 isolate, showing that ESS of ST398 does not have such a regulatory effect (Supplementary Fig. S2). Thus, our results indicated that the impact of ESS on virulence is mediated predominantly by virulence factors whose secretion depends on ESS, such as EsxA and EsxB.
ESS of ST398 promotes resistance to elimination by human neutrophils
The mechanism by which ESS contributes to virulence has remained mostly unclear. In a previous study, ESS was found to impact colonization14, during which staphylococci are believed to grow in a biofilm mode of growth23. We therefore measured the impact of ST398 ESS on biofilm formation. However, no impact of ST398 ESS on biofilm formation was found (Supplementary Fig. S3). Recently, EsxA and EsxB were reported to delay apoptosis and contribute to release of S. aureus from epithelial cells16. These results prompted us to investigate whether ESS impacts S. aureus interaction with professional phagocytes, in particular neutrophils, which represent the first line of defense against an S. aureus infection. An interaction with this key part of innate host defense would explain the impact of ESS on acute virulence that we observed in the animal infection models. Thus, we analyzed the degree of bacterial survival and lysis of neutrophils upon incubation of wild-type versus essB mutant bacteria with human neutrophils. Bacterial survival was significantly higher and lysis of neutrophils significantly greater with wild-type as compared to essB mutant bacteria (Fig. 6A,B). In contrast to PSMs, which are lytic to a variety of cells including neutrophils24, the cytolytic effect of ESS was specific, as the ESS did not influence lysis of erythrocytes (Supplementary Fig. S4). Furthermore, microscopic analysis indicated that ESS contributes to lysis after ingestion (Fig. 6C). These results revealed that ESS is an important factor determining interaction of ST398 with neutrophils as main effectors of innate host defense.
Human neutrophils were isolated from heparinized venous blood of healthy individuals. Bacteria from mid-logarithmic growth phase were washed and incubated with human neutrophils at a 10:1 ratio. (A) Neutrophil lysis was determined by measuring release of LDH. (B) Bacterial survival was measured by CFU plating. **p < 0.01; ***p < 0.001 (unpaired t-tests, deletion mutant versus wild-type, and complemented mutant versus deletion mutant harboring control plasmid). (C) Microscopic evaluation of lysis after phagocytosis. Blood smears were obtained at different time points of incubation of bacteria with neutrophils, and ingestion and lysis were analyzed by light microscopy using a modified Wright-Giemsa stain. The number of lysed among all (=100) neutrophils that had ingested bacteria is shown on the right for two different donors. *p < 0.01 (unpaired t-tests).
Discussion
The recent decline in S. aureus hospital infections, which is likely due to increased hygienic measures, unfortunately is accompanied by an ongoing global surge of CA-SA infections2,6. CA-SA infections are commonly caused by clones that are entirely different from those encountered in hospitals6. While the ST398 lineage has only sporadically and to a minor extent been known to cause such infections, our present study reveals that it has grown to a considerable problem in China, representing the source for about one third of CA-SA infections in Shanghai. Notably, our data also indicate that the ST398 cases are not related to contact with livestock, which is in accordance with data from New York and Brazil11,12.
The molecular underpinnings of what underlies the epidemiological success of CA-SA have remained poorly understood. The methicillin-resistant CA-SA clone USA300, the main source of CA-MRSA infections in the United States, has received much attention6,7. In that clone, epidemiological success has been linked to the acquisition of factors encoded on mobile genetic elements, such as the Panton-Valentine leukocidin (PVL), the arginine catabolic mobile element (ACME), and a comparatively small methicillin resistance element, SCCmec IV (or V)7. With PVL only present in a minority of CA-SA ST398 isolates in our study, this leukocidin cannot be made responsible for the surge in ST398 CA-SA infections that we observed in Shanghai. Rather, our results showing increased expression in ST398 of genome-encoded toxins such as PSMs and α-toxin, and increased expression of the Agr global virulence regulator, which controls many of the corresponding genes, is in accordance with the hypothesis that enhanced production of those toxins has an important role in the virulence potential of CA-SA19.
The present study focused on ESS and adds ESS to the Agr-controlled factors that increase pathogenic success and acute virulence potential in S. aureus. Furthermore, our data indicate that increased expression of ESS may have contributed to the surge in ST398 infections that we observed. Whether ESS has a similarly important role in other CA-SA strains remains to be investigated. Of note, our findings that ESS is Agr-regulated and ST398 isolates show exceptionally high expression of Agr and other Agr-controlled toxins help to explain reports on strain dependency, such as the reported lack of contribution of ESS to virulence in the functionally Agr-negative strain SA11314.
Finally, our data give important insight into how ESS and the ESS-dependent secreted virulence determinants EsxA and EsXB promote acute virulence. Namely, the observed impact of ESS on neutrophil killing provides a valid explanation of that influence, inasmuch as neutrophils represent the cornerstone of human innate defenses against S. aureus infection.
In conclusion, our study reveals ST398 as an epidemiologically important CA-SA lineage in China. Furthermore, it provides evidence for a previously unrecognized role of ESS in acute virulence of CA-SA strains and links that phenomenon to a role of ESS in resistance to elimination by neutrophils as a pivotal component of innate immunity. In general, our findings support the notion of a key contribution of enhanced production of toxins to the evolution of virulent CA-SA strains.
Materials and Methods
Ethics statement
Heparinized venous blood was obtained from healthy human volunteers in accordance with a protocol approved by the ethics committee of Renji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai (protocol RJ-H-2014-0213). All individuals gave informed consent prior to donating blood. All animal experiments were performed following the Guide for the Care and Use of Laboratory Animals of the Chinese Association for Laboratory Animal Sciences (CALAS) and approved by the ethics committee of Renji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai (protocol RJ-M-2014-0109).
Bacterial strains, plasmids, oligonucleotides, and growth conditions
Laboratory-based surveillance for the molecular characterization of clinical S. aureus infection was performed in one comprehensive teaching hospital for adult patients in Shanghai, China (Renji Hospital affiliated to Shanghai Jiao Tong University) and one teaching hospital for pediatric patients (Shanghai Children’s Medical Center affiliated to Shanghai Jiaotong University). Bacteria were identified as staphylococci by classic microbiological methods: Gram’s stain, catalase and coagulase activity on rabbit plasma. S. aureus strains were further categorized by biochemical characterization using the Api-Staph test (BioMérieux, France). CA-SA was defined as an isolate that was obtained either from an outpatient or from an inpatient ≤24 h after hospital admission and without the patient having any of the following risk factors: contact with the hospital environment in the preceding 6 months, residence in a long-term care facility in the preceding 12 months, S. aureus infection in the preceding 12 months, presence of a central vascular catheter at the time of infection. HA-SA was defined as an isolate that was obtained from an inpatient >24 h after hospital admission, or from an outpatient or inpatient ≤24 h after hospital admission, but with the risk factors listed above. Laboratory strains and plasmids used in this study are listed in Table 2. Escherichia coli was routinely grown in Luria-Bertani medium, S. aureus was grown in tryptic soy broth (TSB) (Oxoid) with 0.25% glucose or agar plates at 37 °C. Antibiotics were used at the following concentrations: ampicillin, 100 μg/ml; chloramphenicol, 10 μg/ml. All oligonucleotides used in the present study are listed in Table 3.
Molecular typing
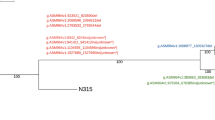
Molecular typing was performed using multi-locus sequence typing (MLST) as previously described25. PCR amplicons of seven S. aureus housekeeping genes (arcC, aroE, glpF, gmk, pta, tpi, and yqiL) were obtained from chromosomal DNA. The sequences of the PCR products were compared with the existing sequences available at the MLST website (http://www.mlst.net).
Allelic gene replacement by homologous recombination and genetic complementation
To delete the essB gene from the genome of S. aureus ST398, a representative clinical isolate (RJ-ST398) was chosen, which was recovered from the abscess of a patient with skin infection. The homologous recombination procedure was performed as described26, using plasmid pKOR1. DNA fragments for upstream and downstream sequences of essB were PCR amplified from chromosomal DNA of RJ-ST398, and overlap PCR was used to obtain a fused PCR product. This product was cloned into pKOR1 using clonase reaction and attB sites, yielding plasmid pKOR1ΔessB. The resulting plasmid was transferred via electroporation first to S. aureus RN4220 and then RJ-ST398. The allelic replacement procedure was performed as described27. Proper integration was verified by analytical PCR and sequencing of the genomic DNA at the borders of the PCR-derived regions. For genetic complementation, the essB gene was amplified by PCR with primers EssB-SmaI-F and EssB-BamHI-R. The essB complementation plasmid was generated by cloning the essB gene in vector pOS1. Growth of the essB deletion and complemented mutants was comparable to that of the wild-type strain (Supplementary Fig. S5). Deletion of the agr system in RJ-ST398 was performed in principle as described for essB.
Quantitative reverse-transcription (RT) PCR
Complementary DNA was synthesized from total RNA using the QuantiTect reverse transcription system (Qiagen) according to the manufacturer’s instructions. Oligonucleotide primers were designed using Primer Express. The resulting complementary DNA and negative control samples were amplified using the QuantiTect SYBR green PCR kit (Qiagen). Reactions were performed in a MicroAmp Optical 96-well reaction plate using a 7500 Sequence Detector (Applied Biosystems). Standard curves were determined for each gene, using purified chromosomal DNA at concentrations of 0.005–50 ng/ml. All quantitative reverse-transcription polymerase chain reaction (qRT-PCR) experiments were performed in duplicate, unless noted otherwise, with gyrB as control.
Construction and purification of GST-Tag fusion protein and antiserum
The essB gene was cloned and overexpressed as glutathione-S-transferase (GST) fusion. The PCR products were purified and digested with BamHI and EcoRI. The genes were cloned into the GST gene fusion vector pGEX-4T-1 (Amersham Biosciences). The recombinant vector pGEX-essB was maintained in E. coli strain BL21 (Amersham Biosciences) for overexpression. Cultures were grown at 30 °C with aeration to an OD600 of 1.0. IPTG was subsequently added to a final concentration of 0.5 mM, and the culture was incubated with aeration for an additional 5 h. Then the cells were harvested. The fusion protein was purified using a GST-Tag purification Kit (Chemicon) according to the manufacturer’s instructions. The purified fusion protein was concentrated in Centriprep-10 concentrators (Amicon) and dialysed against 10 mM sodium phosphate buffer (pH 7.5) using PD-10 desalting columns (Amersham Biosciences). The size of the GST fusion protein was confirmed by SDS–PAGE. The purified protein was used to immunize rabbits by Xiangtai Biotech Ltd (Changzhou, China) according to their standard immunization program.
Western blot analysis
Overnight cultures were diluted 1:100 into 50 ml of TSB and incubated at 37 °C with shaking at 200 rpm until grown to an OD600 nm of 1.5–2.0 (mid-logarithmic growth phase). 500 μl bacterial culture was then collected, cells were harvested and resuspended in 50 μl TE buffer (10 mM Tris-HCl, 1mM EDTA, pH 8.0), lysostaphin (100 μg/ml) was added, and cells were incubated for 30 min at 37 °C. Samples were mixed with protein loading buffer and boiled for 10 min. Equivalent amounts of proteins were separated by SDS-PAGE and transferred onto nitrocellulose membranes (Invitrogen). After blocking, the membranes were incubated with EssB antiserum at 4 °C overnight and then incubated with horseradish peroxidase-conjugated secondary antibody at room temperature for 1 h. Images of Western blots were acquired using a Tanon-5200 system. Intensities of reactions with SrtA antibody (kindly provided by Taeok Bae, Indiana University School of Medicine-Northwest, Gary, Indiana) were used as controls to determine loading amounts.
Analysis of hemolytic capacity
Strains were grown to early stationary growth phase (4 h), and equal amounts (2 μl) of cells were spotted on sheep blood agar plates and incubated at 37 °C for 24 h.
Semiquantitative biofilm assay
Semiquantitative biofilm assays were performed as described elsewhere27. Subsequently, cells were fixed by Bouin’s fixative. The fixative was removed after 1 h and wells were washed with PBS. Organisms in the wells were then stained with crystal violet, and the floating stain was washed off with slow- running water. After drying, the stained biofilm was read with a MicroELISA autoreader (BioRad) at 570 nm (crystal violet stain).
Mass spectrometric analysis
Filtrates of cultures grown to an OD600 nm of 5.0 were precipitated with 10% trichloroacetic acid (TCA), washed with ice-cold acetone, and then resuspended in 50 mM Tris-HCl pH 8.0, 4% sodium dodecylsulfate (SDS). Samples were mixed with protein loading buffer and boiled for 10 min. 12% SDS-PAGE was used to pre-fractionate the secreted proteins. Protein samples were subjected to in-gel digestion. Finally, the extracted peptides were vacuum-dried prior to LC-MS/MS analysis on a nanoflow liquid chromatography instrument (EASY-nLC 1000, Thermo Scientific) coupled to an ion trap mass spectrometer (LTQ Velos Pro. Thermo Scientific) in data-dependent mode. Detailed LC-MS/MS settings have been described elsewhere28.
Neutrophil lysis and bacterial survival assays
Neutrophil lysis by whole bacteria was measured using a lactate dehydrogenase (LDH) cytotoxicity detection kit according to the manufacturer’s protocol (Roche) as described elsewhere18. Bacteria were grown to mid-logarithmic growth phase (4 h). Neutrophils and bacteria were used at a 1:10 ratio (MOI 10) and incubated for 3 h before detection of LDH activity. Samples were diluted 1:50 for the assays. To determine survival rates, 100 μl of the culture above was plated on TSA containing 5% sheep blood for S. aureus CFU detection.
For microscopic evaluation of neutrophil killing after phagocytosis, overnight cultures were diluted 1:100 into 50 ml of TSB and incubated at 37 °C with shaking at 200 rpm to late logarithmic growth phase (4 h), washed, and resuspended in sterile phosphate-buffered saline (PBS) at 107 CFU/μl. S. aureus cells were mixed with heparinized venous blood at a ratio of blood/bacterial solution of 1:10 (v/v) and incubated at 37 °C. Blood smears were prepared after the indicated times of incubation and cells were stained with a modified Wright-Giemsa stain. The number of neutrophils lysed by S. aureus among the total number of neutrophils that had ingested S. aureus (n = 100 were analyzed) was calculated by microscopic examination.
Mouse bacteremia and skin abscess models
BALB/c female mice were used for the bacteremia model. Outbred, immunocompetent hairless female mice were used for the abscess model. All mice were between 4 and 6 weeks of age at the time of use. S. aureus strains were grown to mid-logarithmic phase, washed once with sterile phosphate buffered saline (PBS), then resuspended in PBS. For the bacteremia model, the BALB/c female mice were infected with live S. aureus. Mice of group I were injected with 100 μl PBS containing 109 CFU and used for survival analysis; mice of group II were injected with 108 CFU. Control animals received PBS only. After inoculation, mouse health and disease advancement were monitored every day, and mice were euthanized immediately if they showed signs of respiratory distress, mobility loss, or inability to eat and drink. All surviving animals in group I were euthanized at 48 h. The surviving animals in group II were euthanized 4 days after injection. In group II, S. aureus CFU in blood were assessed by plating 10 μl blood on TSB agar. Serum samples were used for TNF-α detection. Kidneys were excised, washed with saline, and one kidney was fixed in 4% formalin (Sigma). Paraffin embedding and hematoxylin & eosin (H&E) staining were performed as previously described18. The other kidney was homogenized in 0.5 ml of TSB, the homogenized kidney tissue diluted and plated on TSB agar for determination of CFU.
For the abscess model, mice were anesthetized with isoflurane and inoculated with 50 μl PBS containing 107 live S. aureus or saline alone in the left flank by subcutaneous injection. Animals were examined at 24-h intervals for a total of 4 d. Abscess length (L) and width (W) values were measured to calculate the area of abscesses with the formula area (A) = π (L × W)/2. All animals were euthanized 4 days after injection. Abscess material samples of 0.05 g were homogenized in 0.5 ml PBS for the measurement of the cytokine TNF-α (Bio-Plex Pro Mouse Cytokine; Bio-Rad Laboratories).
Statistics
Statistical analysis was performed using Graph-Pad Prism, version 6.02. Error bars in all graphs show the standard deviation (±SD).
Additional Information
How to cite this article: Wang, Y. et al. Role of the ESAT-6 secretion system in virulence of the emerging community-associated Staphylococcus aureus lineage ST398. Sci. Rep. 6, 25163; doi: 10.1038/srep25163 (2016).
References
Lowy, F. D. Staphylococcus aureus infections. N Engl J Med 339, 520–532 (1998).
Dantes, R. et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med 173, 1970–1978 (2013).
Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United States, 2013. Atlanta: CDC (2013) (Date of access: 18/11/2015). Available from: http://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf.
Tong, S. Y., Davis, J. S., Eichenberger, E., Holland, T. L. & Fowler, V. G., Jr. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev 28, 603–661 (2015).
Chuang, Y. Y. & Huang, Y. C. Molecular epidemiology of community-associated meticillin-resistant Staphylococcus aureus in Asia. Lancet Infect Dis 13, 698–708 (2013).
DeLeo, F. R., Otto, M., Kreiswirth, B. N. & Chambers, H. F. Community-associated meticillin-resistant Staphylococcus aureus . Lancet 375, 1557–1568 (2010).
Otto, M. Basis of virulence in community-associated methicillin-resistant Staphylococcus aureus . Annu Rev Microbiol 64, 143–162 (2010).
Geng, W. et al. Community-acquired, methicillin-resistant Staphylococcus aureus isolated from children with community-onset pneumonia in China. Pediatr Pulmonol 45, 387–394 (2010).
Fluit, A. C. Livestock-associated Staphylococcus aureus . Clin Microbiol Infect 18, 735–744 (2012).
Graveland, H., Duim, B., van Duijkeren, E., Heederik, D. & Wagenaar, J. A. Livestock-associated methicillin-resistant Staphylococcus aureus in animals and humans. Int J Med Microbiol 301, 630–634 (2011).
Uhlemann, A. C. et al. Identification of a highly transmissible animal-independent Staphylococcus aureus ST398 clone with distinct genomic and cell adhesion properties. mBio 3, doi: 10.1128/mBio.00027-12 (2012).
Bonesso, M. F. et al. Key Role of alpha-Toxin in Fatal Pneumonia Caused by Staphylococcus aureus Sequence Type 398. Am J Respir Crit Care Med 193, 217–220 (2016).
Burts, M. L., Williams, W. A., DeBord, K. & Missiakas, D. M. EsxA and EsxB are secreted by an ESAT-6-like system that is required for the pathogenesis of Staphylococcus aureus infections. Proc Natl Acad Sci USA 102, 1169–1174 (2005).
Kneuper, H. et al. Heterogeneity in ess transcriptional organization and variable contribution of the Ess/Type VII protein secretion system to virulence across closely related Staphylococcus aureus strains. Mol Microbiol 93, 928–943 (2014).
Burts, M. L., DeDent, A. C. & Missiakas, D. M. EsaC substrate for the ESAT-6 secretion pathway and its role in persistent infections of Staphylococcus aureus . Mol Microbiol 69, 736–746 (2008).
Korea, C. G. et al. Staphylococcal Esx proteins modulate apoptosis and release of intracellular Staphylococcus aureus during infection in epithelial cells. Infect Immun 82, 4144–4153 (2014).
Tristan, A. et al. Global distribution of Panton-Valentine leukocidin–positive methicillin-resistant Staphylococcus aureus, 2006. Emerg Infect Dis 13, 594–600 (2007).
Li, M. et al. MRSA epidemic linked to a quickly spreading colonization and virulence determinant. Nat Med 18, 816–819 (2012).
Zhu, Y., Li, T., Wang, Y., Hong, X. & Li, M. Community-associated Staphylococcus aureus ST398 isolates compared with hospital-associated ST5 and ST239 isolates in terms of virulence and antimicrobial resistance. Chin J Infect Chemother 15, 295–301 (2015).
Cheung, G. Y., Wang, R., Khan, B. A., Sturdevant, D. E. & Otto, M. Role of the accessory gene regulator agr in community-associated methicillin-resistant Staphylococcus aureus pathogenesis. Infect Immun 79, 1927–1935 (2011).
Cramton, S. E., Gerke, C., Schnell, N. F., Nichols, W. W. & Gotz, F. The intercellular adhesion (ica) locus is present in Staphylococcus aureus and is required for biofilm formation. Infect Immun 67, 5427–5433 (1999).
Chen, Y. H., Anderson, M., Hendrickx, A. P. & Missiakas, D. Characterization of EssB, a protein required for secretion of ESAT-6 like proteins in Staphylococcus aureus . BMC Microbiol 12, 219 (2012).
Otto, M. Staphylococcal biofilms. Curr Top Microbiol Immunol 322, 207–228 (2008).
Peschel, A. & Otto, M. Phenol-soluble modulins and staphylococcal infection. Nat Rev Microbiol 11, 667–673 (2013).
Enright, M. C., Day, N. P., Davies, C. E., Peacock, S. J. & Spratt, B. G. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus . J Clin Microbiol 38, 1008–1015 (2000).
Bae, T. & Schneewind, O. Allelic replacement in Staphylococcus aureus with inducible counter-selection. Plasmid 55, 58–63 (2006).
Vuong, C., Gerke, C., Somerville, G. A., Fischer, E. R. & Otto, M. Quorum-sensing control of biofilm factors in Staphylococcus epidermidis . J Infect Dis 188, 706–718 (2003).
Hu, M., Liu, Y., Yu, K. & Liu, X. Decreasing the amount of trypsin in in-gel digestion leads to diminished chemical noise and improved protein identifications. J Proteomics 109, 16–25 (2014).
de Azavedo, J. C. et al. Expression of the cloned toxic shock syndrome toxin 1 gene (tst) in vivo with a rabbit uterine model. Infect Immun 50, 304–309 (1985).
Bubeck Wardenburg, J., Williams, W. A. & Missiakas, D. Host defenses against Staphylococcus aureus infection require recognition of bacterial lipoproteins. Proc Natl Acad Sci USA 103, 13831–13836 (2006).
Acknowledgements
This study was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases (M.O.), the National Natural Science Foundation of China (grants 81322025, 81421001 and 81371875, M. L.), the Shanghai Shuguang Talent Project (grant 12SG03, M. L.), and the Shanghai Committee of Science and Technology, China (grants 14140901000, 15411960500, M. L.).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: M.O., X.L. and M.L. Performed the experiments Y.W., M.H., J.Q., Y.D., T.L., F.Z. and K.Y. Analyzed the data: Y.W., Q.L., L.H., B.Z., M.O., X.L. and M.L. Contributed reagents/materials/analysis tools: J.F. and X.L. Wrote the paper: Y.W., M.O. and M.L.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Wang, Y., Hu, M., Liu, Q. et al. Role of the ESAT-6 secretion system in virulence of the emerging community-associated Staphylococcus aureus lineage ST398. Sci Rep 6, 25163 (2016). https://doi.org/10.1038/srep25163
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep25163
This article is cited by
-
The pro-inflammatory effect of Staphylokinase contributes to community-associated Staphylococcus aureus pneumonia
Communications Biology (2022)
-
The type VII secretion system protects Staphylococcus aureus against antimicrobial host fatty acids
Scientific Reports (2020)
-
Complete genome sequencing of three human clinical isolates of Staphylococcus caprae reveals virulence factors similar to those of S. epidermidis and S. capitis
BMC Genomics (2018)
-
Distinct virulent network between healthcare- and community-associated Staphylococcus aureus based on proteomic analysis
Clinical Proteomics (2018)
-
Phylogenetic analysis and virulence determinant of the host-adapted Staphylococcus aureus lineage ST188 in China
Emerging Microbes & Infections (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.