Abstract
Recent successes with monoclonal antibody cocktails ZMappTM and MIL77 against Ebola virus (EBOV) infections have reignited interest in antibody-based therapeutics. Since the production process for monoclonal antibodies can be prolonged and costly, alternative treatments should be investigated. We produced purified equine antisera from horses hyperimmunized with EBOV virus-like particles, and tested the post-exposure efficacy of the antisera in a mouse model of infection. BALB/c mice were given up to 2 mg of purified equine antisera per animal, at 30 minutes, 1 or 2 days post-infection (dpi), in which all animals survived. To decrease the possibility of serum sickness, the equine antisera was digested with pepsin to generate F(ab′)2 fragments, with in vitro neutralizing activity comparable to whole immunoglobulin. Full protection was achieved with when treatment was initiated at 1 dpi, but the suboptimal protection observed with the 30 minute and 2 dpi groups demonstrate that in addition to virus neutralization, other Fc-dependent antibody mechanisms may also contribute to survival. Guinea pigs given 20 mg of antisera or F(ab′)2 at or starting at 1 or 2 dpi were also fully protected from EBOV infection. These results justify future efficacy studies for purified equine products in NHPs.
Similar content being viewed by others
Introduction
Ebola virus (EBOV) is a pathogen from the Filoviridae family, and is capable of causing severe hemorrhagic fever in humans and non-human primates. Past outbreaks of EBOV disease (EVD) were sporadic, unpredictable and localized to remote regions of central Africa, with the death toll reaching up to 90%1. EBOV is one of the most lethal viruses known to humans and a licensed prophylactic or therapeutic still remains unavailable. In a clinical setting, there is currently little that can be done for infected patients outside of supportive care, which includes fluid replenishment, administration of antivirals, and management of secondary symptoms2,3. The combination of these reasons means that there are high personal risks involved with working on EBOV in a laboratory setting, and as such it is classified as a Biosafety Level 4 (BSL-4) agent.
In the spring of 2014, a new EBOV variant emerged in the West African nation of Guinea4, an area in which the virus had not been previously reported. The outbreak soon spread to neighbouring Sierra Leone and Liberia. Occasionally, cases have been exported into other countries through travel; with countries located in Africa, Europe and North America all having recorded EBOV cases imported by travel, or repatriation of infected citizens. As of mid-December 2015, there are over 11,000 fatalities and 28,000 infections5, the largest EVD outbreak in history. Although the outbreak is now largely under control with no reported cases since the week of November 29th, 20155, the virus had shown itself at the peak of the outbreak to be extremely resistant to traditional containment methods designed to curb EBOV transmission.
Passive immunotherapy with sera of animal origin has been used for over 120 years to treat bacterial and viral infections, envenomations and drug intoxications. In 2012, a report demonstrated that the passive transfer of IgG from nonhuman primate (NHP) survivors of EBOV disease to naive NHPs was sufficient to confer post-exposure protection against EBOV challenge in all animals6. Building on these findings, cocktails of monoclonal antibodies (mAbs) raised against the EBOV glycoprotein (GP) were soon shown afterwards to be effective in the treatment of EBOV disease7,8. This culminated in the development of ZMappTM, a combination of three mAbs produced in genetically modified tobacco plants, which were shown to reverse advanced EBOV disease in experimentally-infected NHPs9, and may have provided a survival benefit when administered to EBOV-infected patients10. A second antibody cocktail (MIL-77), which was based on ZMappTM and produced in modified CHO cells, were later shown to have similar efficacy to ZMappTM in NHPs11. Therefore, passive immunotherapy is an extremely promising approach to control EBOV disease.
Due to the ease of management, high antibody yield and low risk of human contamination by virus or adventitious agents, horses are the most commonly used animal species in the production of hyperimmune sera. Immunization itself is standardized and performed under optimal conditions for both personnel and animals. Passive immunotherapy is still commonly used in countries that are still resource-poor medically, and treatment with immune globulin against rabies virus12 and Clostridium tetani13 infections remains frequent in Africa, Asia and Latin America.
The lower manufacturing costs of hyperimmune equine antisera therefore represents an attractive alternate avenue of treatment, especially to developing and third-world countries, compared to the more costly production process of EBOV GP-specific mAbs. To investigate further, we first prepared purified anti-EBOV antisera via the immunization of horses with EBOV enveloped virus-like particles (eVLP), which consists of EBOV viral protein 40 (VP40) and GP. The equine antisera was then tested in vitro using a neutralization assay with recombinant EBOV expressing eGFP (EBOV-eGFP), as well as in vivo against a lethal challenge with mouse-adapted EBOV (MA-EBOV) in immunocompetent BALB/c mice. To investigate whether EBOV infections can be controlled by virus neutralization alone, and to prevent the possible induction of serum sickness in humans that would be administered antisera, the post-exposure efficacy of F(ab′)2 (immunoglobulin treated with pepsin to remove the Fc regions of the antibody) were also investigated side-by-side with equine antisera in all experiments as a potential alternate treatment. Guinea pigs then were used to confirm the efficacy results from mouse studies, due to their status as a higher phylogenic species which more closely models hallmarks of EVD in humans. Additionally, prior to efficacy studies both the equine antisera and F(ab′)2 had been evaluated for safety in the Peking Union Medical College Center for New Drug Safety Evaluation, Chinese Academy of Medical Sciences, which is certified by the Food and Drug Agency of the People’s Republic of China. Both equine-derived products were found to meet safety standards for clinical use in China.
Results
Immunization of horses and production of equine antibody products
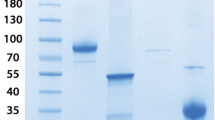
The horses were immunized with eVLP produced from the infection of Sf9 cells with rBV-VP40-GP. The filamentous eVLP were observed under an electron microscope (Supplementary Figure 1) and confirmed to be morphologically similar to EBOV. Immunoblotting of rBV-VP40-GP infected Sf9 cell lysates demonstrated that the eVLP contained EBOV GP and VP40 (Supplementary Figure 2). Three horses were immunized intramuscularly (IM) with 7 injections of eVLP over 11 weeks and the hyperimmune sera were collected from each animal at specified timepoints (Fig. 1A) to determine the serum titers by neutralization assay against a recombinant HIV-1 virus pseudotyped with EBOV GP. A pseudotyped-virus was used for these studies to confirm the in vitro efficacy of the antisera preparations under Biosafety Level 2 (BSL-2) conditions, before subsequent studies in the BSL-4 laboratory. Neutralizing serum titers were detectable after the 5th immunization at week 6, and increased until the 7th immunization at week 11 (Fig. 1B). The serum neutralizing antibody titers of two horses were 1:40,960 after seven immunizations, and was 1:20,480 for the third animal. The equine antisera (purified by ammonium sulphate-based precipitation) was then digested with pepsin at a concentration of 5–10 U/ml for 45 to 90 min and purified to generate F(ab′)2 fragments. The purity of the antisera and F(ab′)2 preparations, as determined by SDS-PAGE followed by thin layer chromatography, was determined to be 95% and 83%, respectively (Fig. 2). Approximately 2000 mL of purified antisera could be obtained from each horse during each collection, with the stock concentration between 20–25 mg/mL. Up to 3–5 collections can be performed on each horse, therefore each hyperimmunized horse yields between 120 to 250 g of purified antisera.
(A) Horses (70#, 395#, 399#) were vaccinated IM with 3 mg of eVLP (at 0 and 2 weeks) or 5 mg of eVLP (at 4, 5, 6, 7, 9 weeks), and horse 15# was vaccinated with equal quantity of insect cell protein, and hyperimmune sera were collected at 11 weeks after the first vaccination. (B) An inhibition assay with EBOV GP-pseudotyped HIV-1 virus was conducted to determine the neutralizing antibody titers of 0, 1, 3, 5, 6, 7, 8, 11 weeks. Numbers 70, 395 and 399 represent individual horses that were vaccinated, and number 15 represents a control horse. Assays were repeated three times in triplicate, and the results presented (from one assay) are representative of all three assays.
Coomassie blue staining of antisera and F(ab′)2 preparations. 10 μg of antisera and F(ab′)2 were mixed with non-reducing (without β-mercaptoethanol) protein sample buffer, heated at 95 °C for 5 min, and then subjected to SDS-PAGE followed by Coomassie blue staining. (A) antisera preparations (lane 1–2). The purity was determined to be 95%. (B) F(ab′)2 preparations (lane 1–5). The purity was determined to be 83%.
In vitro characterization of equine antisera and F(ab‘)2
The equine antisera and F(ab′)2 products were first characterized against a laboratory generated EBOV-eGFP for their potential to neutralize EBOV. Equine antisera and F(ab′)2 were found to possess levels of similar neutralizing activity, with the half effective maximal concentration (EC50) of the products to be 1.07 μg/mL and 2.12 μg/mL, respectively (Fig. 3). Moreover, the neutralization activities of both the equine antisera and F(ab′)2 were complete at a concentration of 12.5 μg/mL, indicating that the two products were indistinguishable from each other in terms of neutralization at high concentrations. EBOV-specific IgG in the equine antisera preparations were also determined by ELISA. Serial 2-fold dilutions of stock antisera with a concentration of 18–20 mg/mL were assayed in triplicate over three independent experiments, and the titer was determined to be between 10,240 and 20,480 endpoint dilutions.
The neutralizing activities of equine antisera and F(ab′)2 against EBOV-eGFP were compared over different concentrations (x-axis). Total fluorescence from infected VeroE6 cells at 3 dpi were shown as a percentage of the fluorescence observed with the PBS control, which is set at 100% (y-axis). Samples were processed in triplicate, and error bars indicate standard error. Data shown in this figure are representative of three independent neutralization studies with F(ab′)2 or antisera.
In vivo characterization of equine antisera and F(ab‘)2
The half-life of the F(ab′)2 and equine antisera were first assessed in guinea pigs, and found to be 8–12 hours and 3–4 days, respectively (Supplementary Table 1). The protective efficacy of equine antisera and F(ab′)2 were assessed over three experiments in BALB/c mice. The first experiment was to compare the efficacy of antisera and F(ab′)2 treatments side-by-side. Groups of 8 mice were given intraperitoneal (IP) injections of F(ab′)2 at 200 μg per dose, twice daily for 3 days (b.i.d. × 3d), starting at either 1 or 2 days post-infection (dpi) with a uniformly lethal dose of MA-EBOV. For comparison, groups of 8 mice were administered an IP injection of equine IgG at 200 μg per dose (q.d. × 1d), at either 1 or 2 dpi. Control mice were given an equal volume of PBS in place of the treatment (q.d. × 1d) at 1 dpi. PBS was used instead of non-specific immunoglobulin or F(ab′)2, because previous studies involving passive transfer of non-specific antisera in mice and NHPs did not result in protection14,15, and thus survival due to the non-specific effects of serum proteins is considered unlikely. Control mice lost approximately 23% of its body weight over the course of the experiment and none survived, with a mean time to death (MTD) of 6.4 ± 0.5 dpi. Five of eight mice given F(ab′)2 starting at 1 dpi survived (p-value < 0.0001, compared with PBS group), with an average weight loss of 18.7% and a MTD of 8.3 ± 0.6 dpi; however, none of the mice given F(ab′)2 starting at 2 dpi survived the challenge (p-value = 0.9777, compared with PBS group), with an average weight loss of 19.0% and a MTD of 5.8 ± 1.8 dpi (Fig. 4A,B). Five of eight mice given antisera at 1 dpi survived (p-value < 0.0001, compared with PBS group), with an average weight loss of 14.6% and a MTD of 8.3 ± 0.6 dpi (Fig. 4C). Three of eight mice given antisera at 2 dpi survived (p-value = 0.0446, compared with PBS group), with an average weight loss of 12.3% and a MTD of 6.6 ± 0.6 dpi (Fig. 4D). Comparing groups with equal treatment times, there was no statistical difference between F(ab′)2 at 1 or 2 dpi (p-value 1.0000 and 0.0613, respectively). However, given that multiple administrations of F(ab′)2 were required to achieve similar protection levels demonstrated by a single injection of antisera, the results suggest that equine antisera is a superior product to F(ab′)2 in terms of efficacy, possibly due to a longer in vivo half-life of equine antiseras.
Groups of 8 BALB/c mice were administered IP with either F(ab′)2, twice daily for 3 days starting at 1 or 2 dpi with MA-EBOV, or one injection of antisera at 1 or 2 dpi. Injections contained 200 μg of antisera or F(ab′)2. (A) The survival and (B) percentage weight change are shown for mice administered F(ab′)2, whereas (C) the survival and (D) percentage weight change are shown for animals given equine antisera.
Since F(ab′)2 appear to be promising early in MA-EBOV infection, the dosage of this treatment was increased for a second experiment. Groups of 9–10 mice were given IP injections of F(ab′)2 at 1 or 2 mg per dose, twice daily for 3 days (b.i.d. × 3d), starting at either 30 minutes or 1 dpi with MA-EBOV. Control mice were treated with PBS (q.d. × 1d) at 1 dpi. Control mice lost approximately 17.3% of its body weight over the course of the experiment and none survived, with a MTD of 6.3 ± 1.0 dpi. Partial survival was observed when treatment began 30 minutes after challenge. Four of nine mice in the 1 mg group survived (p-value < 0.0001, compared with PBS group), with an average weight loss of 6.8% and a MTD of 11.6 ± 1.5 dpi, whereas four of ten mice in the 2 mg group survived (p-value < 0.0001, compared with PBS group), with an average weight loss of 6.2% and an MTD of 12.5 ± 1.4 dpi (Fig. 5A,B). In contrast, all mice survived if treatment was initiated at 1 dpi, with negligible weight loss (less than 5%) observed in both the 1 and 2 mg groups (p-value < 0.0001, compared with PBS group), indicating that protection was complete. These results indicate that F(ab′)2 can contribute to protection from MA-EBOV, but only within a certain timeframe after challenge.
The efficacy of equine antisera at higher doses was then investigated in a third experiment. Groups of 10 mice were given IP injections of antisera at 2 mg per dose (q.d. × 1d), at 30 minutes, 1 or 2 dpi with MA-EBOV. Control mice were treated with PBS (q.d. × 1d) at 1 dpi. Control mice lost approximately 17.3% of its body weight over the course of the experiment and none survived, with a MTD of 6.3 ± 1.0 dpi. All mice treated with antisera at 30 minutes and at 1 dpi survived with negligible weight loss (p-value < 0.0001, compared with PBS group). Nine of ten mice treated with antisera at 2 dpi also survived the challenge (p-value < 0.0001, compared with PBS group), with the lone non-survivor dying at 7 dpi and the average peak weight loss determined to be 7.9% within this treatment group (Fig. 6A,B). These results again indicate that equine antisera, compared to F(ab′)2 is able to offer a greater contribution to protection from MA-EBOV in the mouse model due to the need for fewer administrations to achieve a similar level of protection.
Guinea pigs were then used to confirm the protective effects from antisera and F(ab′)2 in a higher phylogenic species for EBOV challenge, since these animals better mimic hallmarks of human EBOV infections, such as coagulation abnormalities16. Groups of 6 animals were given a single IP injection of antisera (q.d. × 1d) starting at 1 or 2 dpi with GA-EBOV, or twice-daily IP injections of F(ab′)2 for three days (b.i.d. × 3d), starting at 1 or 2 dpi. Each injection dose contained 20 mg antisera or F(ab′)2. A group of five control animals were given a single injection of PBS at 1 dpi. Control guinea pigs lost approximately 17.9% of its body weight over the course of the experiment and none survived, with a MTD of 8.2 ± 0.6 dpi. All guinea pigs that were given antisera at 1 or 2 dpi survived (p-values = 0.0011 for both groups, compared with PBS group), with no clinical signs of disease or significant weight loss (Fig. 7A,B). In addition, animals that were given F(ab′)2 starting at 1 or 2 dpi survived GA-EBOV challenge (p-values = 0.0011 for both groups, compared with PBS group) without signs of disease or significant weight loss (Fig. 7A,B). The disparity between the efficacy of F(ab′)2 between mice and guinea pigs may be attributed to a much higher dosage of F(ab′)2 administered per weight: each F(ab′)2 dose for guinea pigs was 100× higher than those given to mice, but the guinea pigs used in this experiment were only 10–20 times bigger than the mice by weight.
Discussion
The lack of BSL-4 laboratories globally, trained personnel as well as the rigors of working under high biocontainment conditions have severely hampered basic research with EBOV, leading to a dearth of vaccines and therapeutics for use in humans. These weaknesses were exposed with the 2014–15 EBOV crises, and highlight the value and need for basic and translational science that occurs prior to an impending threat. In an effort to save lives, several experimental candidate treatments that had been tested for efficacy in mice or NHPs, in addition to approved or nearly-approved drugs developed against unrelated pathogens, were expedited for use in humans under compassionate circumstances, with varying degrees of success17. Of these, antibody-based treatments appear to hold the most promise in the clinic and thus should be further investigated for use in humans.
Passive immunotherapy against EBOV had been tried in the past. Towards the end of the 1995 EBOV outbreak in Kikwit, Zaïre (presently Democratic Republic of the Congo), the passive transfer of whole blood from EBOV survivors to patients resulted in the survival of seven out of eight recipients18. However, safety concerns with blood transfusions, such as the spreading of blood-borne diseases, allergic reactions and concerns of inefficacy19 mean that this approach is controversial and will likely not be used unless a better alternative was unavailable. In the 1990s, Russian investigators had prepared hyperimmunized antisera from horses vaccinated with inactivated EBOV, which were shown to be effective when administered at a dose of 1 mg/kg to baboons, with 100% survival (2 survivors out of 2) when given 2 hours before challenge, and 67% (2 survivors out of 3) when given immediately after challenge20, although baboons are known to be more resistant to EBOV infection compared to other NHP species21. The survival benefits of the equine antisera were limited to a delay in the onset of viremia clinical symptoms when tested in cynomolgus macaques immediately after challenge, at a dose of 60 mg for an animal weighing between 5–6 kg22. Comparing to successful passive immunotherapy studies with purified IgG from NHPs (80 mg/kg), as well as ZMapp and MIL-77 (50 mg/kg), the dosage for the cynomolgus macaque experiment was likely too low at the time. Use of equine antisera as an emergency post-exposure treatment against EBOV has been approved in Russia, and several investigators that had been accidentally exposed to the virus have been administered this treatment, although it is not clear if they had actually been infected23.
The results of this study show that both equine antisera and F(ab′)2 preparations, which can be rapidly produced in large quantities at a lower cost compared to mAbs, are effective in the post-exposure treatment of MA-EBOV challenged mice and GA-EBOV infected guinea pigs. F(ab′)2 was developed in this study due to past documented issues with antisera administrations, in which equine botulinum toxin and anti-snake venom antisera was shown to produce serum sickness at high doses24. However, mice that were given a single dose of antisera demonstrated more complete protection over a greater period of time compared to multiple injections of F(ab′)2. This suggests that F(ab′)2 has a shorter half-life compared to IgG (which has been confirmed in this study), and/or that virus neutralization plays a partial role in survival from EBOV. The observation that administering F(ab′)2 at 1 dpi is more efficacious than when the same treatment was given at 30 minutes post-exposure (Fig. 5A) was also observed in past studies with therapeutic EBOV GP-specific monoclonal antibodies25,26, and suggests that virus neutralization may play a bigger role in protection at a later timepoint after EBOV challenge. With regards to neutralization, past reports have shown that while elevated antisera levels in NHPs vaccinated against EBOV correlated with survival, levels of specific neutralizing antibodies did not27. It is a possible explanation as to why mAb KZ52, which was originally selected for its ability to neutralize EBOV28, failed to protect NHPs when given at a dose of 50 mg/kg starting 1 day before challenge29, and suggests that in the future, the screening of potentially efficacious antibodies against EBOV should not be based solely on the ability of the antibody to neutralize virus.
Fc-dependent antibody functions, which include antibody dependent cellular cytotoxicity, complement-dependent cytotoxicity, and neonatal Fragment crystallizable receptor (FcR)-mediated cross-presentation, likely play a role in protection. For instance, studies in mice against Yellow Fever virus and West Nile virus infections have shown that the protective mechanisms of monoclonal antibodies are dependent on FcR30,31. Furthermore, complement component C1q has been previously shown in Influenza virus and West Nile virus infections to directly enhance the neutralizing activities of antibodies32,33. These mechanisms are not mutually exclusive, but determining their relative importance of each proposed mechanism to efficacy and survival will yield further insight into the specific mechanisms in which antibodies help protect against EBOV disease. Furthermore, the findings of this study justify the testing of equine IgG in a higher phylogenic species for EBOV, such as NHPs, and may result in the development of a safe and economical method for the production of an effective EBOV therapeutic.
Materials and Methods
Ethics statement
Mice and guinea pig experiments were performed at the BSL-4 laboratory in the National Microbiology Laboratory (NML) in Winnipeg, Canada. All rodent experiments have been approved by the Animal Care Committee (ACC) at the Canadian Science Center for Human and Animal Health (CSCHAH), in accordance with the guidelines outlined by the Canadian Council on Animal Care (CCAC). Horse studies were conducted with prior approval from the Animal Welfare and Ethics committee of the Institute of Military Veterinary, Academy of Military Medical Sciences (permit number SCXK-2012-017), according to Horse Quarantine and Immunization Protocols for Equine Serum Production.
Animals
BALB/c mice and Hartley guinea pigs were purchased from a commercial supplier (Charles River). The animals were kept in sterile, autoclaved cages and provided sterilized food and water ad libitum. Animals were also provided red, plastic shelters inside the cages as an added source of stimulation. Horses were purchased from a commercial supplier (Red Hill Military horse farm) and provided food and water ad libitum.
Construction and generation of recombinant baculoviruses
The sequences of EBOV GP and VP40, with lengths of 2,031 and 981 bp, respectively, were derived from GenBank (Zaire ebolavirus strain Zaire 1995, complete genome; GenBank accession No. AY354458). The GP and VP40 genes were cloned into the pUC-57 vector, named pUC-GP and pUC-VP40, and then inserted into pFastBac Dual vector (Life technologies) under the polyhedrin promoter and p10 promoter respectively, resulting in plasmid pFastBac Dual-VP40-GP. The purified plasmid was transformed into DH10™Bac E. coli (Life technologies) for transposition into a bacmid. A Cellfection® II Reagent (Life technologies) was used according to manufacturer instructions to generate recombinant baculoviruses co-expressing Ebola VP40 and GP (rBV-VP40-GP).
eVLP production and inspection
To produce eVLP, Sf9 cells were infected with rBV-VP40-GP at a multiplicity of infection (MOI) of 1, and incubated at 27 °C for 4 days. Culture supernatants were harvested and centrifuged at 2000 × g for 30 min to remove cells, and then pelleted by ultracentrifugation at 30,000 × g for 60 min at 4 °C. The pellets were re-suspended in PBS and purified through a 10–30–50% discontinuous sucrose gradient at 25,000 × g for 90 min at 4 °C. The eVLP band obtained between 30% and 50% density range was collected, washed, and re-suspended in PBS34.
For immunoblotting, eVLP and control sample (cell culture supernatant) were separated by 12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis under denaturing conditions, transferred onto a polyvinylidene fluoride (PVDF) membrane (Whatman, Kent, UK) and then probed with mouse anti-EBOV GP polyclonal antibody (Prokaryotic expression GP protein immunized mice) or mouse anti-EBOV VP40 monoclonal antibody (ab1918, abcam) at a dilution of 1:200 overnight at 4 °C. The sample was then incubated with horseradish peroxidase (HRP)-conjugated goat anti-mouse secondary antibody at a dilution of 1:4000 (Millipore, Boston, MA, USA) for 60 min at 37 °C. The PVDF membrane was colored with a chemiluminescence solution (Pierce Biotechnology, Rockford, IL, USA).
For electron microscopy, eVLP were applied onto a carbon-coated formvar grid, which was immediately stained with 1% phosphotungstic acid and then observed by a transmission electron microscope.
Horse immunizations
Horses (n = 3) were vaccinated intramuscularly (subcutaneous multi-point injection) with either 3 or 5 mg of eVLPs emulsified in Freund’s complete adjuvant/Freund’s incomplete adjuvant at weeks 0, 2, 4, 5, 6, 7 and 9 (7 times). Blood samples were collected from the jugular vein at 1 week prior to the first immunization and 1 week after each immunization, and the sera were stored at −80 °C until further analysis.
Fragmentation and purification of equine antibody products
The equine antisera and F(ab′)2 were produced at Changchun Institute of Biological Products Co., Ltd., using the large-scale, Current Good Manufacturing Practice compatible equine antiserum manufacturing platform. Equine antisera and F(ab′)2 preparations were characterized according to guidelines set forth by Chinese Pharmacopoeia (2010 edition), including appearance, color, visible foreign matter, pH value, F(ab′)2 and immunoglobulin content, and sterility. For equine antisera, the blood was taken from the jugular vein of immunized horses, and the sera were separated 2 h later. The horse sera were diluted 8-fold with PBS, centrifuged at 12,000 rpm for 30 min, and supernatants were subjected to filtration through a 0.45 μm filter. The antisera were purified by ammonium sulphate precipitation35, followed by salt column, and then stored in 0.9% NaCl solution. For F(ab′)2: horse sera were diluted 3-fold and the pH was adjusted to 3.2 using 1 M HCl, and then the antisera were subjected to shock digestion at 37 °C for 30 min with pepsin, and 0.4 M NaOH was added to terminate digestion. The digestion products were subjected to salt column purification, followed by Protein A column. The flow-through fluid was harvested and subjected to ultrafiltration to remove the pepsin and small molecular proteins, and the F(ab′)2 was stored in 0.9% NaCl solution.
SDS-PAGE and thin layer chromatography
The purified equine antisera and F(ab′)2 samples were mixed with non-reducing (without β-mercaptoethanol) protein sample buffer, heated at 95 °C for 5 min, and then subjected to SDS-PAGE (12% gel, staining for 3 h and destaining for 2 h); and then the target fractions in the gel were examined by thin layer chromatography scanner (CS-9301, Shimadzu), (transmission, zigzag scan, dual wavelength, swing width: 8 mm, delta Y: 0.1 mm) to determine the purity of equine antisera and F(ab′)2.
ELISA
EBOV GP expressed by E. coli BL-21 was diluted with 0.1 M bicarbonate buffer pH 9.6 to a final concentration of 10 μg/mL, and coated on 96-well ELISA plates overnight at 4 oC (100 μL/well). After blocking with Angiotensin Converting Enzyme (ACE) buffer (Bio-Rad, California, USA) at 37 °C for 2 h, the plates were incubated with 100 μL of serial 2-fold dilutions of stock equine antisera in triplicate at 37 °C for 1.5 h. After washing, 100 μL of HRP-conjugated goat anti-horse IgG (ComWin Biotech Co., Ltd. Beijing, China) diluted 1:20000 in PBS-0.5% Tween was added to the wells and incubated at 37 °C for 50 min. After washing, 100 μL of substrate 3′,5,5′-Tetramethylbenzidine (TMB, Sigma) was added and incubated at room temperature for 30 min. The reaction was stopped by adding 50 μL of 0.5 M H2SO4, and the absorbance was measured at 450 nm. A dilution was considered positive if the absorbance reading was at least twice that of the negative control (PBS) at the same dilution. The IgG endpoint titer was calculated as the highest dilution still showing a positive result. The assay was performed independently three times.
Half-life studies in guinea pigs
Group of 4 guinea pigs were administered an IP injection of 1 mL purified equine antisera (neutralization titer 1:20480) or F(ab′)2 (neutralization titer 1:20480). Blood samples were collected at 0, 1, 4, 8, 12, 24, 48, 72, 96, 120, 144 h post-injection, and sera were used for determination of neutralization titer against a recombinant HIV-1 virus pseudotyped with EBOV GP. The time range post-infection in which the titer decreases by 50% is considered the half-life. Each sample was performed in triplicate.
Determining the protective efficacy of equine antisera
BALB/c mice, 4–6 week old, female and weighing between 15–19 g, were randomly assigned into groups of 8–10 mice. All animals were challenged intraperitoneally (IP) with a dose of 1000 × LD50 mouse-adapted EBOV (MA-EBOV, USAMRIID/BALB/c-lab/COD/1976/Mayinga-MA-p3) in 200 μL DMEM. The treatment was given IP (q.d. × 1d) at 1 or 2 days post-infection (dpi) with 0.2 mg equine anti-EBOV antisera per mouse, or in a subsequent experiment, given IP at 30 minutes, 1 or 2 dpi with 2 mg equine anti-EBOV antisera per mouse. The control group was given the same volume of PBS as mock treatment. All animals were monitored for signs of disease, survival and weight change for 16 days, and survival was monitored for 12 additional days. Female strain Hartley guinea pigs, 4–6 week old and weighing between 200 and 300 g, were randomly assigned into groups of 6 animals. All animals were challenged IP with 1000 × LD50 guinea pig-adapted EBOV (GA-EBOV, VECTOR/C.porcellus-lab/COD/1976/Mayinga-GPA-p7) in 1 mL DMEM. The treatment was given IP (q.d. × 1d) at 1 or 2 dpi with 20 mg equine anti-EBOV IgG per animal. A control group of 5 guinea pigs were given the same volume of PBS as mock treatment. All animals were monitored for signs of disease, survival and weight change for 15 days, and survival was monitored for 13 additional days.
Determining the protective efficacy of F(ab′)2
BALB/c mice, 4–6 week old, female and weighing between 15–19 g, were randomly assigned into groups of 8–10 mice. All mice were challenged IP with a dose of 1000 × LD50 MA-EBOV in 200 μL DMEM. The treatment was given IP at 1 or 2 dpi with 200 μg F(ab′)2 per mouse, or in a subsequent experiment, given IP at 30 minutes, 1 or 2 dpi with either 1 mg or 2 mg of F(ab′)2 per mouse. The treatment was given via IP twice a day for 3 days (b.i.d. × 3d). The control group was given the same volume of PBS as a mock treatment. All animals were monitored for signs of disease, survival and weight change for 16 days, and survival was monitored for 12 additional days. Female strain Hartley guinea pigs, 4–6 week old, were randomly assigned into groups of 6 animals. All animals were challenged IP with 1000 × LD50 guinea pig-adapted EBOV in 1 mL DMEM. The treatment was given IP at 1 or 2 dpi with 20 mg F(ab′)2 per animal. The treatment was given via IP twice a day for 3 days (b.i.d. × 3d). A control group of 5 guinea pigs were given the same volume of PBS as mock treatment. All animals were monitored for signs of disease, survival and weight change for 15 days, and survival was monitored for 13 additional days.
Pseudotyped virus neutralization assay
Titers of equine antisera and F(ab′)2 from horses was tested in an neutralization assay in Huh-7 cells against recombinant HIV-1 virus pseudotyped with EBOV GP. The method for generating pseudotyped viruses was described in a previous publication36. Briefly, pseudotyped virus containing supernatants were incubated either with serially diluted horse sera at 37°C for 1 h, before addition to pre-plated target cells in 96-well culture plates (density of 104 cells/well). Cells were re-fed fresh medium 4 h after addition, and followed by lysing cells at 48 h using cell lysis buffer (Promega) and transferring the lysates into 96-well luminometer plates. Luciferase substrate (Promega) was added to the plates, and the relative luciferase activity was determined. The inhibition of pseudotyped was presented as % inhibition. The highest serum dilution giving over 50% reduction of luciferase activity was regarded as the neutralizing antibody titer.
EBOV-eGFP neutralization assay
Serial two-fold dilutions of F(ab′)2 or antisera (between 12.5 to 0.097656 μg/mL) were incubated with 100 plaque forming units (PFU) of EBOV expressing eGFP (EBOV-eGFP, NML/H.sapiens-lab/COD/1976/Mayinga-eGFP-p3) at 37 °C for 1 h, transferred to Vero E6 cells and incubated at 37 °C for 1 h, and then replaced with DMEM supplemented with 2% fetal bovine serum. Control wells contained PBS instead of F(ab′)2 or antisera, and all samples were repeated in triplicate. The plates were fixed with 10% phosphate buffered formalin at 72 h after infection, and scored for the intensity of eGFP using the BioTek Synergy HT microplate reader. The results were expressed as a percentage of the fluorescence reading with the control (which is set at 100%), and fitted to a 4-parameter logistic curve (Graphpad).
Statistical analysis
The p-values for rodent studies were determined using the Log-rank (Mantel-Cox) test. Calculated values of less than 0.05 were considered statistically significant. All in vivo studies were performed once.
Additional Information
How to cite this article: Zheng, X. et al. Treatment with hyperimmune equine immunoglobulin or immunoglobulin fragments completely protects rodents from Ebola virus infection. Sci. Rep. 6, 24179; doi: 10.1038/srep24179 (2016).
References
CDC.gov. Outbreaks Chronology: Ebola Virus Disease, http://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html (2015). (Date of access: 06/01/2016).
Clark, D. V., Jahrling, P. B. & Lawler, J. V. Clinical management of filovirus-infected patients. Viruses 4, 1668–1686, doi: 10.3390/v4091668 (2012).
Guimard, Y. et al. Organization of patient care during the Ebola hemorrhagic fever epidemic in Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis 179 Suppl 1, S268–273, doi: 10.1086/514315 (1999).
Baize, S. et al. Emergence of Zaire Ebola virus disease in Guinea. N Engl J Med 371, 1418–1425, doi: 10.1056/NEJMoa1404505 (2014).
WHO.int. Ebola Situation Report - 16 December 2015http://apps.who.int/ebola/current-situation/ebola-situation-report-16-december-2015 (2015). (Date of access: 06/01/2016).
Dye, J. M. et al. Postexposure antibody prophylaxis protects nonhuman primates from filovirus disease. Proc Natl Acad Sci USA 109, 5034–5039, doi: 10.1073/pnas.1200409109 (2012).
Olinger, G. G. Jr. et al. Delayed treatment of Ebola virus infection with plant-derived monoclonal antibodies provides protection in rhesus macaques. Proc Natl Acad Sci USA 109, 18030–18035, doi: 10.1073/pnas.1213709109 (2012).
Qiu, X. et al. Successful treatment of ebola virus-infected cynomolgus macaques with monoclonal antibodies. Sci Transl Med 4, 138ra181, doi: 10.1126/scitranslmed.3003876 (2012).
Qiu, X. et al. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature 514, 47–53, doi: 10.1038/nature13777 (2014).
Lyon, G. M. et al. Clinical care of two patients with Ebola virus disease in the United States. N Engl J Med 371, 2402–2409, doi: 10.1056/NEJMoa1409838 (2014).
Qiu, X. et al. Two-mAb Cocktail Protects Macaques Against The Makona Variant of Ebola Virus. Sci Transl Med 8, 329ra33 (2016).
CDC.gov. Use of a Reduced (4-Dose) Vaccine Schedule for Postexposure Prophylaxis to Prevent Human Rabies, http://www.cdc.gov/mmwr/pdf/rr/rr5902.pdf (2010). (Date of access: 06/01/2016).
CDC.gov. Tetanus, http://www.cdc.gov/vaccines/pubs/pinkbook/downloads/tetanus.pdf (2011). (Date of access: 06/01/2016).
Gupta, M., Mahanty, S., Bray, M., Ahmed, R. & Rollin, P. E. Passive transfer of antibodies protects immunocompetent and imunodeficient mice against lethal Ebola virus infection without complete inhibition of viral replication. J Virol 75, 4649–4654, doi: 10.1128/JVI.75.10.4649-4654.2001 (2001).
Dye, J. M. et al. Postexposure antibody prophylaxis protects nonhuman primates from filovirus disease. Proc Natl Acad Sci USA 109, 5034–5039, doi: 10.1073/pnas.1200409109 (2012).
Nakayama, E. & Saijo, M. Animal models for Ebola and Marburg virus infections. Front Microbiol 4, 267, doi: 10.3389/fmicb.2013.00267 (2013).
Wong, G. & Kobinger, G. P. Backs against the wall: novel and existing strategies used during the 2014–2015 Ebola virus outbreak. Clin Microbiol Rev 28, 593–601, doi: 10.1128/CMR.00014-15 (2015).
Mupapa, K. et al. Treatment of Ebola hemorrhagic fever with blood transfusions from convalescent patients. International Scientific and Technical Committee. J Infect Dis 179 Suppl 1, S18–23, doi: 10.1086/514298 (1999).
Erhabor, O. & Adias, T. C. From whole blood to component therapy: the economic, supply/demand need for implementation of component therapy in sub-Saharan Africa. Transfus Clin Biol 18, 516–526, doi: 10.1016/j.tracli.2011.06.001 (2011).
Mikhailov, V. V., Borisevich, I. V., Chernikova, N. K., Potryvaeva, N. V. & Krasnianskii, V. P. [The evaluation in hamadryas baboons of the possibility for the specific prevention of Ebola fever]. Vopr Virusol 39, 82–84 (1994).
Bente, D., Gren, J., Strong, J. E. & Feldmann, H. Disease modeling for Ebola and Marburg viruses. Dis Model Mech 2, 12–17, doi: 10.1242/dmm.000471 (2009).
Jahrling, P. B. et al. Passive immunization of Ebola virus-infected cynomolgus monkeys with immunoglobulin from hyperimmune horses. Arch Virol Suppl 11, 135–140 (1996).
Bray, M. Defense against filoviruses used as biological weapons. Antiviral Res 57, 53–60 (2003).
Black, R. E. & Gunn, R. A. Hypersensitivity reactions associated with botulinal antitoxin. Am J Med 69, 567–570 (1980).
Wilson, J. A. et al. Epitopes involved in antibody-mediated protection from Ebola virus. Science 287, 1664–1666 (2000).
Qiu, X. et al. Ebola GP-specific monoclonal antibodies protect mice and guinea pigs from lethal Ebola virus infection. Plos neglected tropical diseases 6, e1575, doi: 10.1371/journal.pntd.0001575 (2012).
Wong, G. et al. Immune parameters correlate with protection against ebola virus infection in rodents and nonhuman primates. Sci Transl Med 4, 158ra146, doi: 10.1126/scitranslmed.3004582 (2012).
Maruyama, T. et al. Ebola virus can be effectively neutralized by antibody produced in natural human infection. J Virol 73, 6024–6030 (1999).
Oswald, W. B. et al. Neutralizing antibody fails to impact the course of Ebola virus infection in monkeys. Plos Pathog 3, e9, doi: 06-PLPA-RA-0388R2 (2007).
Schlesinger, J. J., Foltzer, M. & Chapman, S. The Fc portion of antibody to yellow fever virus NS1 is a determinant of protection against YF encephalitis in mice. Virology 192, 132–141, doi: 10.1006/viro.1993.1015 (1993).
Chung, K. M. et al. Antibodies against West Nile Virus nonstructural protein NS1 prevent lethal infection through Fc gamma receptor-dependent and -independent mechanisms. J Virol 80, 1340–1351, doi: 10.1128/JVI.80.3.1340-1351.2006 (2006).
Jayasekera, J. P., Moseman, E. A. & Carroll, M. C. Natural antibody and complement mediate neutralization of influenza virus in the absence of prior immunity. J Virol 81, 3487–3494, doi: 10.1128/JVI.02128-06 (2007).
Mehlhop, E. et al. Complement protein C1q reduces the stoichiometric threshold for antibody-mediated neutralization of West Nile virus. Cell Host Microbe 6, 381–391, doi: 10.1016/j.chom.2009.09.003 (2009).
Ye, L. et al. Ebola virus-like particles produced in insect cells exhibit dendritic cell stimulating activity and induce neutralizing antibodies. Virology 351, 260–270, doi: 10.1016/j.virol.2006.03.021 (2006).
Farr, R. S. A quantitative immunochemical measure of the primary interaction between I BSA and antibody. J Infect Dis 103, 239–262 (1958).
Gao, J. et al. Structure of the fusion core and inhibition of fusion by a heptad repeat peptide derived from the S protein of Middle East respiratory syndrome coronavirus. J Virol 87, 13134–13140, doi: 10.1128/JVI.02433-13 (2013).
Acknowledgements
This work was supported by the National Science and Technology Major Project of the ministry of Science and Technology of China (No. 2015ZX09102025 and 2014ZX09102044-007), and the Public Health Agency of Canada. G.W. is the recipient of a Banting Postdoctoral Fellowship from the Canadian Institutes of Health Research (CIHR) and the President’s International Fellowship Initiative from the Chinese Academy of Sciences (CAS).
Author information
Authors and Affiliations
Contributions
X.Z., G.W., Y.Z., H.W., S.H., Y.B., X.Q., S.Y. and X.X. performed the experiments and analyzed the results. X.Z., G.W., G.K., G.F.G., X.Q., S.Y. and X.X. wrote the manuscript. W.C., H.J., W.G., D.C., Z.C., C.W., Q.F., H.C., Y.G., T.W., N.F., F.Y., G.H., Y.Z., N.L., Y.L. and J.Q. prepared the horse antisera. G.F.G., X.Q., S.Y. and X.X. jointly supervised the work. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zheng, X., Wong, G., Zhao, Y. et al. Treatment with hyperimmune equine immunoglobulin or immunoglobulin fragments completely protects rodents from Ebola virus infection. Sci Rep 6, 24179 (2016). https://doi.org/10.1038/srep24179
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep24179
This article is cited by
-
The Application of a Safe Neutralization Assay for Ebola Virus Using Lentivirus-Based Pseudotyped Virus
Virologica Sinica (2021)
-
An adenovirus serotype 2-vectored ebolavirus vaccine generates robust antibody and cell-mediated immune responses in mice and rhesus macaques
Emerging Microbes & Infections (2018)
-
Generation of therapeutic antisera for emerging viral infections
npj Vaccines (2018)
-
Successful post-exposure prophylaxis of Ebola infected non-human primates using Ebola glycoprotein-specific equine IgG
Scientific Reports (2017)
-
Viral effects on the content and function of extracellular vesicles
Nature Reviews Microbiology (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.