Abstract
We evaluated the performance of seven existing risk scoring systems in predicting advanced colorectal neoplasia in an asymptomatic Chinese cohort. We prospectively recruited 5,899 Chinese subjects aged 50–70 years in a colonoscopy screening programme(2008–2014). Scoring systems under evaluation included two scoring tools from the US; one each from Spain, Germany and Poland; the Korean Colorectal Screening(KCS) scores; and the modified Asia Pacific Colorectal Screening(APCS) scores. The c-statistics, sensitivity, specificity, positive predictive values(PPVs) and negative predictive values(NPVs) of these systems were evaluated. The resources required were estimated based on the Number Needed to Screen(NNS) and the Number Needed to Refer for colonoscopy(NNR). Advanced neoplasia was detected in 364 (6.2%) subjects. The German system referred the least proportion of subjects (11.2%) for colonoscopy, whilst the KCS scoring system referred the highest (27.4%). The c-statistics of all systems ranged from 0.56–0.65, with sensitivities ranging from 0.04–0.44 and specificities from 0.74–0.99. The modified APCS scoring system had the highest c-statistics (0.65, 95% C.I. 0.58–0.72). The NNS (12–19) and NNR (5-10) were similar among the scoring systems. The existing scoring systems have variable capability to predict advanced neoplasia among asymptomatic Chinese subjects and further external validation should be performed.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third most common cancer in the world1, accounting for 10% of all malignancies and 8% of all cancer mortality in 2012. Its incidence is rapidly rising in both Western and Asia Pacific countries1,2. CRC screening using colonoscopy has been shown to be effective to reduce CRC mortality by 68%3,4. Both stool-based occult blood tests and colonoscopy have been recommended as primary screening modalities for CRC screening5,6 and the updated Asia Pacific Consensus Recommendations suggested that colonoscopy is the preferred choice in increased risk individuals7.
However, limited colonoscopy resource has been a widely recognized barrier hindering CRC screening8,9. Risk prediction models could therefore prioritize high-risk subjects to receive colonoscopy – which optimizes efficiency of resources for screening. In the past decade, a number of risk scoring systems have been designed and validated based on subjects in various countries and regions10,11,12,13,14,15,16,17. These included two scores derived from US residents10 and US physician, respectively;11 one each from Spain12, Germany13 and Poland;14 the Asia Pacific Colorectal Screening (APCS) score;15 the Korean Colorectal Screening (KCS) score;16 and the modified APCS score17. These studies prospectively recruited asymptomatic CRC screening participants, with significant risk factors identified from a derivation cohort and performance evaluated in a validation cohort. These systems included a combination of well-defined risk factors for CRC as predictive parameters, including age12,18,19, sex12,19,20, family history of CRC12,21, smoking22,23, body mass index (BMI)19,24, dietary factors23,25 and long-term use of non-steroidal anti-inflammatory drugs (NSAIDs)23,26.
Nevertheless, the discriminatory capability of these tools to predict advanced neoplasia in specific population groups remained unexplored. It has been demonstrated that the incidence and distribution of colorectal neoplasia are different among different racial and ethnic groups27,28,29,30. The original studies which published these scoring systems called for external validation in other cohorts10,11,12,13,14,15,16,17. The population of Greater China was 1.39 billion in 2013, excluding residents living in various continents in the globe. The proportion of ethnic Chinese population in the world was 20%31, highlighting a need to evaluate the most suitable tool for risk stratification for this ethnic group.
The objective of this study is to compare the predictive performance and resources required of these seven published risk scoring tools to detect advanced neoplasia in a large Chinese population. These findings could inform the predictive capability of the existing scoring systems and the resources required to identify subjects with advanced neoplasia-i.e. whereby colonoscopy is warranted.
Methods
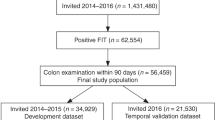
A bowel cancer screening centre was established in Hong Kong in 2008, which provides free-of-charge CRC screening services for eligible Hong Kong citizens32,33. The centre is accessible to all Hong Kong residents. Following several media announcements, we recruited subjects for free screening services by registrations via telephone, e-mail, fax or walk-in. The present evaluation included all screening participants who received colonoscopy in the study period 2008-2014. The Clinical Research Ethics Committee of the Chinese University of Hong Kong approved the study (protocol CRE-2008.404) and the methods were carried out in accordance with the approved guidelines. All participants provided informed consent before enrolling into the study and were invited to visit the centre before screening.
Screening Participants
Upon centre visits, two independent health educators checked for subject eligibility. These eligibility criteria included: (i) age 50–70 years; (ii) the absence of any current and previous CRC symptoms, such as haematochezia, tarry stool, anorexia or change in bowel habit in the past 4 weeks, or unintentional weight loss of greater than 5 kg in the past 6 months; and (iii) not having undergone any CRC screening tests in the past 5 years. Exclusion criteria consist of personal history of CRC, colorectal adenoma, inflammatory bowel disease and the presence of medical conditions which were contraindications for colonoscopy, like cardiopulmonary insufficiency and the use of double antiplatelet therapies.
Screening Colonoscopy
All study participants were explained about the nature, benefits and risk of colonoscopy before the procedures. We used polyethylene glycol (Klean-PrepR, Helsinn Birex Pharmaceuticals Ltd, Ireland) as a standard bowel preparation regime for all participants, who were reminded of colonoscopy attendance before they left the centre. A team of experienced physicians and colorectal surgeons performed all colonoscopy procedures in the endoscopy centres affiliated with the University. The sedation regimen used included midazolam 2.5 mg (Groupe Panpharma, France) and meperidine 25 mg (Martindale Pharmaceuticals, United Kingdom). Further doses of these drugs were administered according to the subject’s level of discomfort. We used air insufflation and aimed for cecal intubation, aiming for a withdrawal time of ≥6 minutes in accordance with the current quality indicators for colonoscopy34. All colorectal lesions were removed and biopsied as deemed appropriate by the endoscopists. We sent all the biopsied samples to an accredited laboratory for gross and microscopic examination. Advanced neoplasia was defined as CRC or any colorectal adenoma which has (1). a size of ≥10 mm in diameter; (2). high grade dysplasia; (3). villous or tubulovillous histologic characteristics, or any combination thereof19. In the presence of multiple lesions, the most advanced characteristic was assigned.
Evaluation of the existing scoring systems: outcome variables and statistical analysis
From a thorough literature review, seven studies which devised and validated scoring systems based on elementary clinical information to predict advanced neoplasia were identified10,11,12,13,14,15,16,17. Table 1 summarizes the key feature, predictor variables and the computational algorithm of each scoring system. We defined the threshold for colonoscopy referral as the cut-off score where: (1). the subjects were classified as high or very high risk; or (2). the subjects in the initial development and validation of the scoring system were found to be at a specific risk level which was just higher than that of the whole cohort in the respective study.
For the US Physician health survey11, only male subjects in our cohort were included, since the US survey exclusively consists of male physicians. In the German cohort evaluated by Tao and colleagues13, we only included non-smokers, non-drinkers, as we do not have detailed information on pack years and drinking frequency in our cohort. For the Poland system devised by Kaminski et al.14, only non-smokers aged 66 years or below from our participants were included. The original APCS scoring system developed by Yeoh and colleagues has been extensively evaluated in the Asia-Pacific countries and the c-statistics was found to be 0.64 ( ± 0.04)15. A modified version of the APCS scoring system has been devised and validated in 7,463 subjects from 11 Asian cities, with a c-statistics of 0.65 (95% C.I. 0.58–0.72)17. It incorporated body mass index as a predictor variable in addition to age, gender, smoking and family history of CRC. In this study we studied the modified APCS system.
The proportion of subjects referred for colonoscopy in our cohort was delineated when different scoring systems were applied – and each was compared with the modified APCS scoring system using McNemar test. The accuracy of all the prediction strategies to detect advanced neoplasia was evaluated, including the sensitivity, specificity and positive predictive values (PPVs) and negative predictive values (NPVs). The discriminatory ability for prediction was computed for each scoring model, presented as the concordance (c-) statistics. The c-statistics was used to measure the discriminatory power between those with and without advanced neoplasia35, which is identical to the Area Under the Curve (AUC) for binary logistic regression models. The statistics considered all pairs of subjects and computed the proportion of pairs in which the model accurately predicted a higher likelihood of advanced neoplasia for subjects categorized as high risk. Similar to the approach adopted by Imperiale et al.36, a c-statistic of 0.7–0.8 was regarded as good discrimination, whilst a value >0.8 indicated excellent discrimination. A c-statistics between 0.6–0.7 had some clinical value whereas c-statistics <0.6 had no clinical value. We employed the deLong test to compare the AUCs of the seven systems. Using the modified APCS scoring system as the comparison group, each system was evaluated according to their ability to accurately classify subjects into high vs. low risk group. This is presented as the Net Reclassification Index (NRI), defined as the sum of differences in proportions of correct reclassification minus incorrect reclassification. A positive NRI indicates more accurate classification of risk for advanced neoplasia by the assessed system than the modified APCS system; whilst a negative NRI indicates less accurate classification of the risk by the assessed system than the modified APCS system.
The resources required to detect advanced neoplasia was estimated by the Number Needed to Screen (NNS) and the Number Needed to Refer (NNR) for colonoscopy to detect one advanced neoplasia. The NNS was the total number of subjects in each subgroup divided by the number of subjects referred for colonoscopy and detected as having advanced neoplasia, according to each risk stratification system. The NNR was the number of subjects referred for colonoscopy divided by the number of subjects referred for colonoscopy and detected as having advanced neoplasia. The Statistical Package for Social Sciences version 19.0 was used for all data analysis. P values < 0.05 were considered statistically significant.
Results
Participant characteristics
From a total of 5,899 eligible screening participants, the average age was 57.7 years (SD 4.9) (Table 2). Male subjects consist of 47.1% and the proportion of smokers and alcohol drinkers was 8.3% and 9.7%, respectively. Of all participants, 1,700 (29.2%) had BMI ≥ 25 kg/m2, 847 (14.4%) had a family history of CRC in a first-degree relative and the proportion of subjects self-reported as having diabetes, hypertension and current NSAID use was 7.6%, 23.2% and 4.7%, respectively. There were 25 CRC (0.4%) and 339 (5.7%) advanced adenomas. The characteristics of the screening participants are summarized in Table 2.
Proportions of colonoscopy referral
The proportion of subjects referred for colonoscopy was the highest with the KCS scores (27.4%, 95% C.I. 26.3%–28.6%), followed by the Spain scores (25.5%, 95% C.I. 24.4%–26.7%) and the modified APCS scores (21.4%, 95% C.I. 20.3%–22.5%). The proportion of colonoscopy referral by applying each scoring system (p < 0.001) was significantly different from that of the modified APCS scores (Table 3).
Performance of the scoring systems
The c-statistics of the scoring systems ranged from 0.56 (95% C.I 0.48–0.64) [the Spain system] to 0.65 (95% C.I. 0.58–0.72) [the modified APCS system] (Table 4). The sensitivity of these systems ranged from 0.04–0.44 and the specificity was moderate to high (range 0.74–0.99). All of them had low PPVs (range 0.10–0.19) and high NPVs (range 0.92–0.96). The deLong tests showed that the AUCs of all the six scores, other than the modified APCS score, had no statistically significant difference.
Using the modified APCS scoring system as a comparator, the NRI of the Spain (−3.3%, 95% C.I. −8.0% to 1.4%), Germany (−0.5%, 95% C.I. −6.4% to 5.5%), Poland (1.2%, 95% C.I. −2.7% to 5.2%) and the KCS (−2.7%, 95% C.I. −7.2% to 1.9%) was statistically similar (all p > 0.05) (Table 5). The US-Seattle (−8.1%, 95% C.I. −13.1% to −3.1%, p = 0.001) and the US physician health survey (−20.4%, 95% C.I. −27.2% to −13.6%, p < 0.001) classified advanced neoplasia less accurately than the modified APCS scores (Table 5).
Colonoscopy resources
The NNS ranged from 12 (95% C.I. 6–21) of the US physician health survey to 19 (95% C.I. 11–30) of the Germany and Poland scores (Table 6). The NNR ranged from 5 (95% C.I. 2–12) of the US physician health survey to 10 (95% C.I. 5–18) of the Spain, Poland and KCS systems. There were no significant differences of both NNS and NNR among the various scoring systems (Table 6).
Discussion
This study compared the performance of seven existing prediction models in a Chinese population. From 5,899 asymptomatic subjects, 6.1% had advanced neoplasia. The proportion of screening participants referred for colonoscopy was the highest using the KCS and the Spain scores and the lowest using the Germany and the US Physician Health Survey criteria. The scoring systems had variable discriminatory ability to predict the risk of advanced neoplasia (c-statistics ranged from 0.56–0.65). The modified APCS score seemed a preferable system to classify high risk subjects based on its highest c-statistics. These findings implied that prediction tools for advanced neoplasia may need further external validation to evaluate their generalizability.
The modified APCS scoring system demonstrated a higher discriminatory ability to detect advanced neoplasia and improvements in risk prediction compared with two other tools. There is a relatively high proportion of Chinese subjects represented in this score (5,795 out of 7,463; 77.6%), whilst the other subjects were recruited in Korea (4.0%), Malaysia (5.8%), the Philippines (0.7%), Singapore (0.9%), Thailand (4.2%), Japan (5.3%), Brunei (1.1%) and Pakistan (0.4%). Also, BMI was included as a predictive variable – a parameter missing in the original APCS score15. In addition, despite the lowest c-statistics of the KCS scoring system16, its NNS and NNR were similar to other scores. It might be that the difference in c-statistics with other systems was so small to observe a clinically significant difference in NNS/NNR. Future studies are needed to explore further rooms for improving the discriminatory capability of the KCS scoring system.
This is the first large-scale study which evaluated the predictive ability and colonoscopy resources required when the existing prediction tools were applied in a Chinese population. The evaluation is unique as we did not only evaluate these scoring systems by their concordance statistics. The approach of solely relying on discrimination measures has been criticized, since calibration (i.e. the agreement between predicted and observed risk) is also a crucial aspect of model performance37,38. Most importantly, comparing c-statistics lacks an apparent clinical interpretation, such as how patient classification would improve with inclusion or exclusion of other predictors in risk scoring systems. Reclassification has recently become a popular approach for comparing improvement among risk scoring systems for diagnosing common diseases39,40,41. A model is considered better when individuals who have subsequently developed the disease and those who have not developed the disease are reclassified to a higher risk category and to a lower risk category, respectively.
This study highlighted a need to modify existing tools with c-statistics <0.60 to risk stratify subjects for colonoscopy screening – and is clinically important as identification of advanced neoplasia enables secondary prevention by polypectomy19,42. The estimation of individual risk for advanced neoplasia may facilitate informed, shared decision making process about screening as part of patient-centred care43. Nevertheless, there are some limitations which should be addressed. Firstly, we invited screening participants who were self-referred following media announcements. They may be different from the general public – therefore our subjects are more representative of patients who volunteered as screening participants. The self-selected population included in the present cohort had low prevalence of smoking or alcohol drinking and high proportion of them had family members suffering from CRC – which may reflect the better health-consciousness when compared with the general population. One may also anticipate that a revised methodology to recruit subjects using a population-based, random sampling approach may meet with a high refusal rate. Secondly, the German and Poland systems13,14 excluded some of our subjects and this might have introduced biases, since in our original cohort comprehensive data on number of pack years among smokers and frequency of alcohol drinking were not collected. The original Kaminski score14 was developed from screening subjects aged between 40–66 years, thus limiting the number of subjects which could be included for external validation. In addition, we are unable to validate some scoring systems, including the prediction model constructed by Cai and colleagues in China, which has been demonstrated as having better discrimination in previous evaluations44. Among eight parameters, four variables require dietary recall of green vegetable, prickled food, fried food and white meat intake. Detailed information of these food items were not collected in our cohort. Another system developed by Law and colleagues in Malaysia45 was mainly reserved for symptomatic patients and none of our subjects in our study was categorized as high risk, as they were all asymptomatic. Other scoring systems required detailed information on family history, physical activity, leisure time vigorous activity, dietary intake, the use of hormone replacement therapy and folate consumption46,47,48,49,50. Critics might argue that exclusion of high-risk subjects (smokers and drinkers) and low-risk subjects (women) might lead to altered estimates of the discriminatory ability of these three scoring systems. Furthermore, the choice of cut-off value for each prediction system was based on the recommendation from the respective original article. It still remains to be explored whether addition of more variables could further improve the scoring systems, such as lifestyle measures (like dietary intake; smoking and alcohol drinking) and medical conditions known to be risk factors for advanced neoplasia (like diabetes and central obesity measured by waist circumference). Besides, some variables like age and BMI could be analyzed by treating them as continuous variables which might enhance the concordance statistics. Finally, the nature of these risk models may apply to lifetime or longer-term prediction of risk for ACN and the cross-sectional nature of the present study might benefit by further prospective colonoscopy follow-up for additional risk score validation.
In summary, these findings suggested that in the absence of newer prediction tools, the modified APCS system could be useful to risk-stratify ethnic Chinese subjects. The formulation and implementation of a higher-performing scoring system may optimize the efficiency of screening resources and prioritize high-risk subjects for colonoscopy. Future studies may evaluate the performance of these scoring systems where the same cut-off values for absolute risk of ACN were applied and target on devising scores using additional variables.
Additional Information
How to cite this article: Wong, M. C. S. et al. The discriminatory capability of existing scores to predict advanced colorectal neoplasia: a prospective colonoscopy study of 5,899 screening participants. Sci. Rep. 6, 20080; doi: 10.1038/srep20080 (2016).
References
GLOBOCAN 2012. Cancer Fact Sheet. Colorectal Cancer Incidence, Mortality and Prevalence Worldwide in 2012. Available at: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. Accessed on 15 Sept, 2014.
Sung, J. J., Lau, J. Y., Goh, K. L. & Leung, W. K. Asia Pacific Working Group on Colorectal Cancer. Increasing incidence of colorectal cancer in Asia: implications for screening. Lancet Oncol 6, 871–6 (2005).
Nishihara, R. et al. Long-Term Colorectal-Cancer Incidence and Mortality after Lower Endoscopy. N Engl J Med 369, 1095–1105 (2013).
Zauber, A. G. et al. Colonoscopic Polypectomy and Long-Term Prevention of Colorectal-Cancer Deaths. N Engl J Med 366, 687–96 (2012).
U.S. Preventive Services Task Forces. Screening for colorectal cancer: recommendation and rationale. Ann Intern Med 137, 129–31 (2002).
Sung, J. J. et al. for The Asia Pacific Working Group on Colorectal Cancer. Asia Pacific consensus recommendations for colorectal cancer screening. Gut 57, 1166–1176 (2008).
Sung, J. J. et al. An updated Asia Pacific Consensus Recommendations on colorectal cancer screening. Gut 64, 121–132 (2015).
Levin, T. R. Colonoscopy capacity: can we build it? Will they come? Gastroenterology 127, 1841–1844 (2004).
Brown, M. L., Klabunde, C. N. & Mysliwiec, P. Current capacity for endoscopic colorectal cancer screening in the United States: data from the National Cancer Institute Survey of Colorectal Cancer Screening Practices. Am J Med 115, 129–133 (2003).
Lin, O. S. et al. Risk stratification for colon neoplasia: screening strategies using colonoscopy and computerized tomographic colonography. Gastroenterology 131, 1011–1019 (2006).
Driver, J. A. et al. Development of a risk score for colorectal cancer in men. Am J Med 120, 257–263 (2007).
Betés, M. et al. Use of colonoscopy as a primary screening test for colorectal cancer in average risk people. Am J Gastroenterol 98, 2648–2654 (2003).
Tao, S., Hoffmeister, M. & Brenner, H. Development and validation of a scoring system to identify individuals at high risk for advanced colorectal neoplasms who should undergo colonoscopy screening. Clin Gastrointest Hepatol 12, 478–485 (2014).
Kaminski, M. F. et al. A score to estimate the likelihood of detecting advanced colorectal neoplasia at colonoscopy. Gut 63, 1112–1119 (2014).
Yeoh, K. G. et al. The Asia-Pacific Colorectal Screening score: a validated tool that stratifies risk for colorectal advanced neoplasia in asymptomatic Asian subjects. Gut 60, 1236–1241 (2011).
Kim, D. H. et al. Development and validation of a risk stratification-based screening model for predicting colorectal advanced neoplasia in Korea. J Clin Gastroenterol 49, 41–49 (2015).
Sung, J. J., Wong, M. C. & Tsoi, K. K. Modified Asia-Pacific Colorectal Screening (APCS) Score to Stratify Risk for Colorectal Advanced Neoplasia in Asymptomatic Population in Asian Subjects. Gastroenterology 146, S-730 (2014).
Lieberman, D. A., Weiss, D. G. & Bond, J. H. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med 343, 162–68 (2002).
Regula, J. et al. Colonoscopy in colorectal-cancer screening for detection of advanced neoplasia. N Engl J Med 355, 1863–72 (2006).
Nguyen, S. P. et al. Gender as a risk factor for advanced neoplasia and colorectal cancer: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 7, 676–81 (2009).
Taylor, D. P. et al. Population-based family history-specific risks for colorectal cancer: a constellation approach. Gastroenterology 138, 877–85 (2010).
Botteri, E. et al. Cigarette smoking and adenomatous polyps: a meta-analysis. Gastroenterology 134, 388–95 (2008).
Lieberman, D. A. et al. VA Cooperative Study Group 380. Risk factors for advanced colonic neoplasia and hyperplastic polyps in asymptomatic individuals. JAMA 290, 2959–67 (2003).
Terry, M. B. et al. Risk factors for advanced colorectal adenomas: a pooled analysis. Cancer Epidemiol Biomarkers Prev 11, 622–9 (2002).
Larsson, S. C. & Wolk, A. Meat consumption and risk of colorectal cancer: a meta-analysis of prospective studies. Int J Cancer 119, 2657–64 (2006).
Cole, B. F. et al. Aspirin for the chemoprevention of colorectal adenomas: meta-analysis of the randomized trials. J Natl Cancer Inst 101, 256–66 (2009).
Soon, M. S. et al. Screening colonoscopy in Chinese and Western patients: a comparative study. Am J Gastroenterol 100, 2749–2755 (2005).
Byeon, J. S. et al. Colorectal neoplasm in asymptomatic Asians: a prospective multinational multicenter colonoscopy survey. Gastrointest Endosc 65, 1015–1022 (2007).
Shavers, V. L. Racial/ethnic variation in the anatomic subsite location of in situ and invasive cancers of the colon. J Natl Med Assoc 99, 733–48 (2007).
Lieberman, D. A. et al. Prevalence of colon polyps detected by colonoscopy screening in asymptomatic black and white patients. JAMA 300, 1417–22 (2008).
World’s Most Typical Person: Han Chinese Man. Wall Street Journal. March 4, 2011. Available at: http://blogs.wsj.com/chinarealtime/2011/03/04/worlds-most-typical-person-han-chinese-man/ Accessed on 21 August 2015.
Wong, M. C. S. et al. A validated tool to predict colorectal neoplasia and inform screening choice for asymptomatic subjects. Gut 63, 1130–6 (2014).
Wong, M. C. S. et al. Prediction of proximal advanced neoplasia: a comparison of four existing sigmoidoscopy-based strategies in a Chinese population. Gut 64, 776–783 (2015).
Segnan, N., Patnick, J. & von Karsa, L. eds. European guidelines for quality assurance in colorectal cancer screening and diagnosis. Luxembourg: Publications Office of the European Union; 2010
Hanley, J. A. & McNeil, B. J. The meaning and the use of the area under a receiver operating characteristic (ROC) curve. Radiology 143, 29–36 (1982).
Imperiale, T. F. et al. Using risk for advanced proximal colonic neoplasia to tailor endoscopic screening for colorectal cancer. Ann Intern Med 139, 959–965 (2003).
Pepe, M. S. et al. Limitations of the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am J Epidemiol 159, 882–90 (2004).
Cook, N. R. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation 115, 928–35 (2007).
Cook, N. R. & Ridker, P. M. Advances in measuring the effect of individual predictors of cardiovascular risk: the role of reclassification measures. Ann Intern Med. 150, 795–802 (2009).
Darabi, H. et al. Breast cancer risk prediction and individualised screening based on common genetic variation and breast density measurement. Breast Cancer Res. 14, R25 (2012).
Lyssenko, V. et al. Clinical risk factors, DNA variants and the development of type 2 diabetes. N Engl J Med. 359, 2220–32 (2008).
Kim, D. H. et al. The usefulness of colonoscopy as a screening test for detecting colorectal polyps. Hepatogastroenterology 54, 2240–2 (2007).
Sheridan, S., Harris, R. & Woolf, S. Shared decision making about screening and chemoprevention. A suggested approach from the US Preventive Services Task Force. Am J Prev Med 26, 56–66 (2004).
Cai, Q. C. et al. Derivation and validation of a prediction rule for estimating advanced colorectal neoplasm risk in average-risk Chinese. Am J Epidemiol 175, 584–93 (2012).
Law, C. W. et al. Development of A Risk Score to Stratify Symptomatic Adults Referred for Colonoscopy. J Gastroenterol Hepatol. 29, 1890–1896 (2014).
Kastrinos, F. et al. Development and validation of a colon cancer risk assessment tool for patients undergoing colonoscopy. Am J Gastroenterol 104, 1508–1518 (2009).
Park, Y. et al. Validation of a colorectal cancer risk prediction model among white patients age 50 years and older. J Clin Oncol 27, 694–698 (2009).
Freedman, A. N. et al. Colorectal cancer risk prediction tool for white men and women without known susceptibility. J Clin Oncol 27, 686–693 (2009).
Wei, E. K. et al. Cumulative risk of colon cancer up to age 70 years by risk factor status using data from the Nurses’ Health Study. Am J Epidemiol 170, 863–872 (2009).
Ma, E. et al. Japan Public Health Center-based Prospective Study Group. 10-Year risk of colorectal cancer: development and validation of a prediction model in middle-aged Japanese men. Cancer Epidemiol 34, 534–541 (2010).
Acknowledgements
We acknowledged the full funding support by the Hong Kong Jockey Club Charities Trust. We acknowledge the Hong Kong Jockey Club Charities Trust which funded this project.
Author information
Authors and Affiliations
Contributions
M.C.S.W. participated in design of the study, analysis of the results and writing of the first draft of the manuscript; J.Y.L.C., S.N. and T.Y.T.L. participate in design of study and analysis of results; A.K.C.L. conducted the study and analyzed the results; S.H.W., S.C.N., S.S.M.N., J.C.Y.W., F.K.L.C. and J.J.Y.S. participated in design and performance of the study, analysis and discussion; All authors reviewed and approved the final manuscript. All authors included on a paper fulfill the criteria of authorship. There is no one else who fulfills the criteria but has not been included as an author.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Wong, M., Ching, J., Ng, S. et al. The discriminatory capability of existing scores to predict advanced colorectal neoplasia: a prospective colonoscopy study of 5,899 screening participants. Sci Rep 6, 20080 (2016). https://doi.org/10.1038/srep20080
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep20080
This article is cited by
-
An adjusted Asia-Pacific colorectal screening score system to predict advanced colorectal neoplasia in asymptomatic Chinese patients
BMC Gastroenterology (2023)
-
Relationship between oral and physical function and length of participation in long-term care prevention programs in community-dwelling older Japanese women
European Geriatric Medicine (2021)
-
Risk Scores for Predicting Advanced Colorectal Neoplasia in the Average-risk Population: A Systematic Review and Meta-analysis
American Journal of Gastroenterology (2018)
-
A scoring model for predicting advanced colorectal neoplasia in a screened population of asymptomatic Japanese individuals
Journal of Gastroenterology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.