Abstract
Despite some studies having indicated a possible association between appendicitis and duodenal ulcers, this association was mainly based on regional samples or limited clinician experiences and as such, did not permit unequivocal conclusions. In this case-control study, we examined the association of acute appendicitis with peptic ulcers using a population-based database. We included 3574 patients with acute appendicitis as cases and 3574 sex- and age-matched controls. A Chi-squared test showed that there was a significant difference in the prevalences of prior peptic ulcers between cases and controls (21.7% vs. 16.8%, p < 0.001). The adjusted odds ratio (OR) of prior peptic ulcers for cases was 1.40 (95% confidence interval [CI]: 1.24~1.54, p < 0.001) compared to controls. The results further revealed that younger groups demonstrated higher ORs for prior peptic ulcers among cases than controls. In particular, the adjusted OR for cases < 30 years old was as high as 1.65 (95% CI = 1.25~2.19; p < 0.001) compared to controls. However, we failed to observe an association of acute appendicitis with peptic ulcers in the ≥ 60-year age group (OR = 1.19, 95% CI = 0.93~1.52). We concluded that there is an association between acute appendicitis and a previous diagnosis of peptic ulcers.
Similar content being viewed by others
Introduction
Acute appendicitis is the most common acute surgical condition of the abdomen. In the general population, the lifetime risk of acute appendicitis is about 7%~16%1,2. The etiology of acute appendicitis remains uncertain. Obstruction of the appendiceal lumen is considered an important part of the pathogenesis of acute appendicitis. The obstruction can have multiple causes, including fecaliths, lymphoid hyperplasia (related to viral illnesses and bacterial and fungal infections), parasites, foreign bodies, Crohn’s disease, tuberculosis, tumors, or endometriosis3,4,5. However, two recent large-scale studies showed that only 6.8% and 10.5% of appendicitis specimens had mechanical obstruction6,7. Furthermore, previous studies reported that in a certain portion of appendicitis cases, appendiceal lumen obstruction was due to spasms or hypertonicity of the neuromusculature at the appendicocecal juncture similar to the mechanism of pylorospasms, caused by an autonomic nervous imbalance8,9. Other studies also suggested that the frequent concurrence of pylorospasms, duodenal ulcers and appendicitis was related to an association of direct nerve connections among the appendix, pylorus and duodenum10,11.
Despite some studies having indicated a possible association between appendicitis and duodenal ulcers, this association was mainly based on regional samples or limited clinician experiences and as such, did not permit unequivocal conclusions. This case-control study aimed to examine the association of acute appendicitis with peptic ulcers using a population-based database.
Methods
Database
Data for this case-control study were sourced from the “Longitudinal Health Insurance Database 2005 (LHID2005)”. Taiwan has been implementing its National Health Insurance (NHI) program since 1995 and the LHID2005 includes registration files and original medical claims for 1,000,000 enrollees. These 1,000,000 enrollees were randomly selected from all enrollees listed in the 2005 Registry of Beneficiaries under the NHI program (n = 25.68 million) by the Taiwan National Health Research Institute. Many researchers have employed the LHID2005 to longitudinally trace the utilization of medical services for these 1,000,000 enrollees. The LHID2005 also provides an excellent opportunity to explore the association of acute appendicitis with peptic ulcers. The Taiwan National Health Research Institute and independent researchers have demonstrated the representative validity of the data from the NHI program12,13. Additionally, many researchers have utilized the LHID2005 to conduct and publish studies in internationally peer-reviewed journals14,15.
This study was exempt from full review by the Institutional Review Board of the National Defense Medical Center since the LHID2005 consists of de-identified secondary data released to the public for research purposes.
Study sample
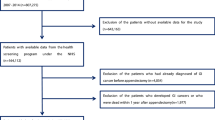
We first selected cases by identifying 4287 hospitalized patients with a first-time principal discharge diagnosis of acute appendicitis (International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes 540, 540.0, 540.1 and 540.9) between January 2008 and December 2012. Patients aged <18 years old (n = 713) were excluded in order to limit the study sample to the adult population. As a result, 3574 patients with acute appendicitis were included as cases. We further defined the date of receiving their first-time diagnosis of acute appendicitis as the index date.
For the controls, we first excluded all enrollees who had a history of acute appendicitis from the Registry of Beneficiaries since initiation of the NHI program in 1995. We then retrieved 3574 enrollees (one for every case) matched to the cases in terms of sex, age and year of the index date. A control was selected by matching them to a given case with acute appendicitis simply on their utilization of medical services in the same index year of that particular case. We further defined the date of the first use of ambulatory care in that matched year as the index date for controls.
Exposure assessment
We identified peptic ulcer cases based on ICD-9-CM codes 531~533. In Taiwan, when a physician suspects that a patient is affected by a peptic ulcer, he or she may provide the patient with a temporary diagnosis of a peptic ulcer in order to conduct the associated clinical examinations or lab tests for confirmation. The peptic ulcer is frequently diagnosed by gastroenterologists based upon characteristic symptoms, endoscopies, or barium contrast x-rays, etc. If a patient has a confirmed peptic ulcer diagnosis after examinations, he or she will receive routine therapy and have a second peptic ulcer diagnosis in their next outpatient visit. On the other hand, if all feasible tests have excluded the possibility of a peptic ulcer, the patient will not receive a diagnosis of a peptic ulcer again. In order to increase the validity of the diagnoses of peptic ulcers, we selected subjects who have received two or more peptic ulcer diagnoses; with at least one being made by a certified gastroenterologist. In addition, we only consider peptic ulcer cases if they have received at least two peptic ulcer diagnoses prior to the index date.
Statistical analysis
The SAS system (SAS, Cary, NC) was used for all statistical analyses. Pearson χ2 tests were performed to examine differences between cases and controls by monthly income (NT$0~15,840, NT$15,841~25,000 and ≥ NT$25,001), geographical location (northern, central, eastern and southern Taiwan) and urbanization level of the patient’s residence (five levels with 1 being the most and 5 the least urbanized). We also performed conditional logistic regressions (conditioned on sex, age and index year) to estimate the association of acute appendicitis with previously diagnosed peptic ulcers.
Additionally, subgroup analyses were conducted to investigate odds ratios (ORs) for peptic ulcer of sampled patients by age group (18~29, 30~59 and ≥ 60 years old). We also analyzed the association between acute appendicitis and previously diagnosed peptic ulcer stratified by the presence of gastric ulcer, duodenal ulcer, Helicobacter pylori (H. pylori)-associated peptic ulcer and non-steroidal anti-inflammatory drugs (NSAID)-associated peptic ulcer. The patients with H pylori-associated peptic ulcer were categorized by those who receiving H pylori eradication therapy. H pylori eradication therapy was defined as proton pump inhibitor or H2 receptor antagonist, plus two antibiotics (clarithromycin, metronidazole, amoxicillin, tetracycline, or levofloxacin), combined with or without bismuth. The duration of therapy was between 7 to 14 days. NSAID-associated peptic ulcer in this study was identified as those patients who had been prescribed NSAIDs for over 30 days prior to the occurrence of peptic ulcer. Furthermore, we identified gastric ulcer cases and duodenal ulcer cases based on ICD-9-CM codes 531 and 532, respectively. Statistical significance was set at p < 0.05.
Results
Of the 7148 sample patients, mean ages for the total study sample, cases and controls were 43.3 ± 17.1 ( ± standard deviation), 43.1 ± 17.1 and 43.3 ± 17.0 years, respectively (p = 0.656). After matching for sex, age and index year, Table 1 shows that there were no significant differences in urbanization level (p = 0.951), monthly income (p = 0.067), geographic region (p = 0.132), or medical history of hyperlipidemia (p = 0.863), congestive heart failure (p = 0.215), chronic renal failure (p = 0.736),cirrhosis (p = 0.106) and malignancy (p = 1.000) between cases and controls. In addition, there were significant differences in prevalences of comorbidities of hypertension (17.7% vs. 19.9%; p = 0.014) and diabetes (8.0% vs. 9.3%; p = 0.048) between cases and controls.
Table 2 presents the prevalence of prior peptic ulcers in sampled patients. Of the total sample, 1377 (19.3%) had a history of peptic ulcers prior to the index date. A Chi-squared test further found that there was a significant difference in the prevalences of prior peptic ulcers between cases and controls (21.7% vs. 16.8%, p < 0.001). Moreover, using a conditional logistic regression analysis (conditioned on sex, age and index year), we found that the odds ratio (OR) of prior peptic ulcers for cases was 1.37 (95% confidence interval [CI]: 1.21~1.54, p < 0.001) compared to controls. Furthermore, the adjusted OR for cases was 1.40 (95% CI: 1.24~1.57) in comparison to controls after adjusting for hypertension and diabetes.
Table 3 presents a analysis of prior peptic ulcers stratified by age group. The results revealed that younger groups demonstrated higher ORs for prior peptic ulcers among cases than controls. In particular, the adjusted OR in cases < 30 years old was as high as 1.65 (95% CI = 1.25~2.19; p < 0.001) compared to controls. However, we failed to observe an association of acute appendicitis with peptic ulcers in the ≥ 60-year age group (adjusted OR = 1.19, 95% CI = 0.93~1.52).
Table 4 shows the further analyses of association between acute appendicitis and prior peptic ulcers by the presence of gastric ulcers, duodenal ulcers, H. pylori-associated ulcers or NSAIDs-associated ulcers. The findings consistently indicated that acute appendicitis was associated with H. pylori-associated peptic ulcers (adjusted OR = 1.59, 95% CI = 1.36~1.86), NSAID-associated peptic ulcers (adjusted OR = 2.18, 95% CI = 1.75~2.72), gastric ulcers (adjusted OR = 1.41, 95% CI = 1.22~1.64), or duodenal ulcers (adjusted OR = 1.27, 95% CI = 1.05~1.54).
Additionally, the sensitivity analysis of the association between acute appendicitis and prior peptic ulcers is presented in Table 5. It shows that acute appendicitis is consistently and significantly associated with prior peptic ulcers, even including cases who have received only one, two, or ≥3 peptic ulcer diagnoses prior to the index date (adjusted ORs were 1.82, 1.40 and 1.52 for cases who have received one, two, or ≥3 peptic ulcer diagnoses prior to the index date, respectively). The acute appendicitis is also significantly related with prior peptic ulcers, even including cases who received confirmed peptic ulcer diagnoses after receiving endoscopy (adjusted ORs was 1.79).
Discussion
This case-control study revealed that 21.7% of hospitalized patients due to acute appendicitis had a history of peptic ulcers. A conditional logistic regression analysis showed that previous peptic ulcers were significantly associated with acute appendicitis (OR = 1.37, 95% CI = 1.21~1.54).
Mechanisms affecting the association between peptic ulcers and acute appendicitis remain unclear. The high prevalence of prior peptic ulcers in patients with acute appendicitis can possibly be explained by an autonomic imbalance and spasms of the neuromusculature at the appendicocecal junction. Previous studies indicated that the mechanism of dyskinesia of the pylorus (pylorospasms) is similar to dysfunction at the appendicocecal junction, because both of them share the same sympathetic nerve origin8,10. One recent animal study even demonstrated that antral ulcers significantly destroy the innervation between the intramural descending neuron and pyloric sphincter muscles, which result in pylorospasms and gastric emptying malfunction9. Some studies also reported that pylorospasms occur in 27% of duodenal ulcer and 89% of gastric ulcer patients10,11,16. Furthermore, studies found that appendicitis was significantly associated with duodenal ulcers, but not with Helicobacter pylori10,11,17,18,19. Our findings also suggest that peptic ulcers themselves were associated with acute appendicitis.
Bacteria are nowadays considered to play the most important role in appendiceal inflammation, in contrast to obstruction of the appendix20,21,22. Previous studies suggested that Fusobacterium nucleatum/necrophorum infection was responsible for the majority of causes of acute appendicitis22,23. Overgrowth of intragastric bacteria including Fusobacterium spp. is due to hypochlorhydria after long-term use of proton pump inhibitors (PPIs)24. Thus, peptic ulcers with long-term use of gastric acid secretory inhibitors could be potential risk factors for acute appendicitis.
However, the present study failed to observe an association between acute appendicitis and peptic ulcers in the elderly (≥60 years old) (OR = 1.18, 95% CI = 0.92~1.25). Previous studies suggested that acute appendicitis in the elderly is mainly due to lumen obstruction by residual stools or undigested food, which contribute to degenerative changes in the elderly appendix and poor colon peristalsis with age, or are secondary to frequent medications or comorbidities in the elderly25,26,27. According the anatomical and physiological changes in the elderly, the pathogenesis of appendiceal inflammation differs from that in young adults25,26.
This study has several strengths. First, a population-based dataset with a large sample size was used to explore the relationship between of acute appendicitis and peptic ulcers. The large sample size afforded a considerable statistical advantage in detecting real differences between cases and controls. Second, we believe that the diagnoses of peptic ulcers had very high validity because they were made by certified gastroenterologists after performing panendoscopy.
Nevertheless, results of this study need to be seen in the light of several limitations. The first limitation is that the LHID2005 provides no information on dietary fiber consumption, histology, or the existence of fecaliths in appendectomy specimens28. Second, physicians do not routinely identify the bacterial species in non-complicated appendicitis cases in Taiwan. This may have influenced the pathogenesis of acute appendicitis. Third, the NHI program in Taiwan was initiated in 1995, so the dataset used in the present study only allowed us to trace medical utilization from 1996 to 2013. Therefore, we could not exclude those patients who had undergone appendectomy before 1996. Therefore, it is very possible that some of the controls in this study had undergone appendectomy before 1996. However, if such a bias exists in the data, the results of our analysis would be biased towards the null. Finally, the severity of peptic ulcers could not be determined from the registry.
Despite the aforementioned limitations, this study demonstrated a potential association between acute appendicitis and peptic ulcers. We suggested that clinicians be alert in suspecting acute appendicitis for abdominal pain in patients with a history of peptic ulcers. Additionally, clinicians can provide instructions for patients with a history of peptic ulcers to seek medical services as soon as possible if they have severe abdominal pain. Nevertheless, further studies are suggested to explore the potential pathophysiology mechanisms for the relationship between acute appendicitis and peptic ulcers.
Additional Information
How to cite this article: Tsai, M.-C. et al. Acute Appendicitis Is Associated with Peptic Ulcers: A Population-based Study. Sci. Rep. 5, 18044; doi: 10.1038/srep18044 (2015).
References
Addiss, D. G. et al. The epidemiology of appendicitis and appendectomy in the United States. Am. J. Epidemiol. 132, 910–925 (1990).
Lee, J. H. et al. The epidemiology of appendicitis and appendectomy in South Korea: national registry data. J. Epidemiol. 20, 97–105 (2010).
Hardin, D. M. Jr. Acute appendicitis: review and update. Am. Fam. Physician 60, 2027–2034 (1999).
Lamps, L. W. Infectious causes of appendicitis. Infect. Dis. Clin. North Am. 24, 995–1018 (2010).
Singh, J. P. & Mariadason, J. G. Role of the faecolith in modern-day appendicitis. Ann. R. Coll. Surg. Engl. 95, 48–51 (2013).
Chandrasegaram, M. D. et al. Pathologies of the appendix: a 10-year review of 4670 appendicectomy specimens. ANZ. J. Surg. 82, 844–847 (2012).
Marudanayagam, R. et al. Review of the pathological results of 2660 appendicectomy specimens. J. Gastroenterol. 41, 745–749 (2006).
Connell, F. G. Etiology of appendicitis. Am. J. Surg. 2, 232–238 (1937).
Zalecki, M. The Influence of Antral Ulcers on Intramural Gastric Nerve Projections Supplying the Pyloric Sphincter in the Pig (Sus scrofa domestica)-Neuronal Tracing Studies. PLoS One 10, e0126958 (2015).
Aaron, C. D. Chronic appendicitis, pylorospasm and duodenal ulcer, a preliminary note. JAMA. LXIV, 1845 (1915).
Burden, V. G. Chronic appendicitis-duodenal ulcer. Am. J. Surg : 21, 235–239 (1933).
Cheng C. L. et al. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol. Drug. Saf. 20, 236–242 (2011).
Cheng, C. L. et al. Validity of in-hospital mortality data among patients with acute myocardial infarction or stroke in National Health Insurance Research Database in Taiwan. Int. J. Cardiol. 201, 96–101 (2015).
Liou, T. H. et al. Risk of stroke in patients with rheumatism: a nationwide longitudinal population-based study. Sci. Rep. 4, 5110 (2014).
Lin, H. W. et al. Risk of ovarian cancer in women with pelvic inflammatory disease: a population-based study. Lancet. Oncol. 12, 900–904 (2011).
Hughson, W. Reflex spasm of the pylorus and its relation to diseases the digestive organs. Arch. Surge. 11, 136–151 (1925).
Fanning, N. F. et al. Helicobacter pylori does not play a role in the etiology of acute appendicitis. Ir. J. Med. Sci. 167, 39–40 (1998).
Pavlidis, T. E. et al. Helicobacter pylori infection in patients undergoing appendectomy. Swiss. Surg. 8, 110–112 (2002).
Kell, M. R. et al. Nitric oxide synthetase and Helicobacter pylori in patients undergoing appendicectomy. Br. J. Surg. 86, 1538–1542 (1999).
Arnbjörnsson, E. & Bengmark, S. Role of obstruction in the pathogenesis of acute appendicitis. Am. J. Surg. 147, 390–392 (1984).
Carr, N. J. The pathology of acute appendicitis. Ann. Diagn. Pathol. 4, 46–58 (2000).
Swidsinski, A. et al. Acute appendicitis is characterised by local invasion with Fusobacterium nucleatum/necrophorum. Gut 60, 34–40 (2011).
Bennett, K. W. & Eley. A., Fusobacteria: new taxonomy and related diseases. J. Med. Microbiol. 39, 246–254 (1993).
Väkeväinen, S. et al. Hypochlorhydria induced by a proton pump inhibitor leads to intragastric microbial production of acetaldehyde from ethanol. Aliment. Pharmacol. Ther. 14, 1511–1518 (2000).
Maxwell, J. M. & Ragland, J. J. Appendicitis, improvements in diagnosis and treatment. Am. Surg. 57, 282–285 (1991).
Peltokallio, P. & Jauhianinen, K. Acute appendicitis in the aged patient. Arch. Surg. 100, 140–143 (1970).
Spinzi, G. C. Bowel care in the elderly. Dig. Dis. 25, 160–165 (2007).
Jones, B. A. et al. The prevalence of appendiceal fecaliths in patients with and without appendicitis. A comparative study from Canada and South Africa. Ann. Surg. 202, 80–82 (1985).
Author information
Authors and Affiliations
Contributions
M.C. and L.T. participated in the design of the study and helped to draft the manuscript. H.C. and S.D. performed the statistical analysis and helped to draft the manuscript. C.Z. conceived of the study, participated in its design and coordination and helped to draft the manuscript. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Tsai, MC., Kao, LT., Lin, HC. et al. Acute Appendicitis Is Associated with Peptic Ulcers: A Population-based Study. Sci Rep 5, 18044 (2015). https://doi.org/10.1038/srep18044
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep18044
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.