Abstract
The sensitivity and accuracy of the Risk/Injury/Failure/Loss/End-stage (RIFLE) versus acute kidney injury Network (AKIN) criteria for acute kidney injury (AKI) in critically ill patients remains uncertain. Therefore, we performed a systematic review and meta-analysis to investigate the incidence and prognostic value of the RIFLE versus AKIN criteria for AKI in critically ill patients. Literatures were identified by searching Medline, Embase, PubMed and China National Knowledge Infrastructure (CNKI) database. Nineteen studies with 171,889 participants were included. The pooled estimates of relative risk (RR) were analyzed. We found that the RIFLE and AKIN criteria is different for the incidence of AKI in intensive care unit (ICU) patients (P = 0.02, RR = 0.88), while not for cardiac surgery patients (P = 0.30, RR = 0.93). For AKI-related hospital mortality, the AKIN criteria did not show a better ability in predicting hospital mortality in either ICU (P = 0.19, RR = 1.01) or cardiac surgery patients (P = 0.61, RR = 0.98) compared to RIFLE criteria. Our findings supported that the AKIN criteria can identify more patients in classifying AKI compared to RIFLE criteria, but not showing a better ability in predicting hospital mortality. Moreover, both RIFLE and AKIN criteria for AKI in cardiac surgery patients had better predictive ability compared with the ICU patients.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is the newly name replaced the term acute renal failure1. It is manifested with changes in urine output, creatinine and blood chemistries2. AKI is common worldwide and is associated with significant morbidity, mortality and resource use with a higher risk for the development of chronic kidney disease (CKD) especially for critical ill patients3,4,5,6. Using the Kidney Disease: Improving Global Outcome (KDIGO) definition, a meta-analysis showed that the incidence of AKI in adults and children were 21.6% and 33.7%, respectively, the AKI-associated mortality rates were 23.9% and 13.8% in adults and children, respectively7. AKI is a common and important diagnostic and therapeutic challenge for clinicians8. More than 200 different definitions of AKI were provided9. These multiple definitions make for clinical confusion and difficulty in the diagnosing of this condition10. Several classifications for AKI have been made during the past few years to better define this disease. A consensus definition of AKI was published by the Acute Dialysis Quality Initiative (ADQI) in 20041. This consensus definition is termed the Risk/Injury/Failure/Loss/End-stage (RIFLE) criteria and the following categories were used: ‘Risk’ is the least severe category of AKI, followed by ‘Injury’, ‘Failure’, ‘Loss’ and ‘End-stage renal disease’. In 2007, a modified version of the RIFLE criteria was published by the AKI Network (AKIN)—known as the AKIN criteria11. Definition of AKI: the categories of Risk, Injury and Failure. Since then, many studies compared the two measures to evaluate the incidence and risk factor of AKI, some studies evaluated the sensitivity and accuracy of the RIFLE and AKIN criteria for critically ill patients, some authors also proposed to evaluate the hospital mortality and outcome of AKI patients by the two classifications. However, the results are still inconclusive. In the present study, we aimed to perform a systematic review and pool the available data to evaluate the incidence and prognostic value of the RIFLE and AKIN classification for AKI patients.
Results
Flow and Study Characteristics
The literature search yielded 299 articles, 19 studies12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30 were eligible for inclusion and flow diagram of included/excluded studies was showed in Fig. 1. Twelve studies for Intensive care units (ICU) with 138,521 patients, 7 studies for cardiac surgery with 33,038 patients. There are 8 studies from Asia, 5 from Europe, both America and Australia have 2 studies, each of Brazil and Bitlis had one study. 15 studies were retrospective and 4 studies were prospective, all included studies are compare RIFLE with AKIN for AKI patients in ICU or cardiac surgery, the basic characteristics of the included studies are summarized in Table 1. Among these studies, 7 studies were multicenter, 12 studies were from single center, 14 studies use hospital mortality to evaluate mortality endpoint, 1 study uses mortality of ARF and 1 study with 28-day mortality, 3 studies did not acquire the endpoint information. The quality of the including studies by QUDAS II was listed below (Supplementary figure 1).
The RIFLE VS. AKIN classification for the incidence of AKI in ICU patients
Twelve studies with 138,521 patients were included for the incidence of AKI in ICU patients, 50,054 patients were diagnosed AKI with RIFLE classification and 50,521 patients were diagnosed AKI with AKIN classification. As shown in Tables 2 and 3, the incidence of AKI range from 18.13%–66.67% and 24.14%–76.67% by RIFLE and AKIN classification, respectively. The total incidence of AKI diagnosed by RIFLE and AKIN classification showed a significance difference (RR, 0.88; 95%CI, 0.80–0.98; P = 0.02; Fig. 2), for each stage, the Risk VS. Stage 1 (RR, 0.70; 95%CI, 0.53–0.93; P = 0.02; Fig. 2) and the Injury VS. Stage 2 (RR, 1.29; 95%CI, 1.17–1.43; P < 0.00001; Fig. 2) for the incidence of AKI were showed a significant difference, but the Failure VS. Stage 3 (RR, 0.90; 95%CI, 0.73–1.11; P = 0.34; Fig. 2) for the incidence of AKI in ICU patients were not showed significant difference.
The RIFLE VS. AKIN classification for the hospital mortality of AKI in ICU patients
There are 10 studies to evaluate the mortality for AKI patients, 49,879 patients diagnosed with AKI using the RIFLE classification and 13,423 patients died in hospital, 13,279 patients died in hospital with a total 50,275 AKI patients using AKIN classification, As shown in Tables 2 and 3, the total hospital mortality was 0.27 and 0.26 by RIFLE and AKIN classification respectively, both classifications were not showed statistical significance (RR, 1.01; 95%CI, 0.99–1.03; P = 0.19; Fig. 3), for each stage, the Risk VS. Stage 1 (RR, 0.96; 95%CI, 0.93–1.00; P = 0.04; Fig. 3) was showed a significant difference, but both the Injury VS. Stage 2 (RR, 1.00; 95%CI, 0.96–1.03; P = 0.95; Fig. 3) and the Failure VS. Stage 3 (RR, 1.01; 95%CI, 0.92–1.04; P = 0.75; Fig. 3) for the hospital mortality of AKI were not showed a significant difference.
The RIFLE VS. AKIN classification for AKI in cardiac surgery patients
Seven studies with 33,038 patients reported the RIFLE and AKIN classification for AKI in cardiac surgery patients, AKI were 9,659 patients with RIFLE classification and 9,717 patients with AKIN classification. The information was listed in Tables 3 and 4 and the two classifications did not have a difference to diagnosis the incidence of AKI (RR, 0.93; 95%CI, 0.81–1.07; P = 0.30; Fig. 4), for each stage comparison, the Risk VS. Stage 1 (RR, 0.85; 95%CI, 0.71–1.03; P = 0.09; Fig. 4) and the Failure VS. Stage 3 (RR, 0.64; 95%CI, 0.39–1.05; P = 0.08; Fig. 4) for the incidence of AKI were also not showed a statistical significant difference, but the Injury VS. Stage 2 (RR, 2.06; 95%CI, 1.61–2.64; P < 0.00001; Fig. 4) was quiet different with the incidence of AKI in cardiac surgery patients.
The RIFLE VS. AKIN classification for the hospital mortality of AKI in cardiac surgery patients
Six studies to evaluate the mortality for AKI in cardiac surgery patients, 9,530 patients diagnosed with AKI using the RIFLE classification and 821 patients died in hospital, 837 patients died in hospital with a total of 9,591 AKI patients using AKIN classification. As showed in Tables 3 and 4, the total hospital mortality in cardiac surgery patients by RIFLE and AKIN classification were not showed significant difference, the RR ratio were 0.98, 95%CI, 0.89–1.07; P = 0.61; Fig. 5, for each stage comparison, there were also not showed a statistical significant difference among the Risk VS. Stage 1(RR, 1.16; 95%CI, 0.71–1.89; P = 0.55; Fig. 5), the Injury VS. Stage 2(RR, 0.87; 95%CI, 0.71–1.06; P = 0.16; Fig. 5) and the Failure VS. Stage 3(RR, 0.92; 95%CI, 0.78–1.09; P = 0.34; Fig. 5).
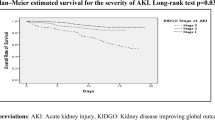
Area under the receiver operator characteristics (AuROC) curves for the RIFLE and AKIN classification for hospital mortality of AKI
The AuROC curve for incidence was 0.598 for RIFLE classification (95%CI, 0.592–0.603, P<0.0001) and was 0.594 for AKIN classification (95%CI, 0.589–0.600, P < 0.0001) for hospital mortality of AKI in ICU patients, whereas the AuROC curve was 0.762 (95%CI, 0.743–0.782, P < 0.0001) for RIFLE classification and was 0.761 for AKIN classification (95%CI, 0.741–0.781, P < 0.0001) for hospital mortality of AKI in cardiac surgery patients, although the AuROC curve was not significant between RIFLE and AKIN classification in either ICU patients or cardiac surgery patients, the AuROC of both RIFLE and AKIN classification for cardiac surgery patients had better predictive ability compared with the ICU patients (Fig. 6).
Area under the receiver operator characteristics (AuROC) curves for the RIFLE and AKIN classification.
(A) The RIFLE classification for the incidence of AKI in ICU patients (AuROC = 0.598). (B) The AKIN classification for the incidence of AKI in ICU patients (AuROC = 0.594). (C) The RIFLE classification for the hospital mortality of AKI in cardiac surgery patients (AuROC = 0.762). (D) The AKIN classification for the hospital mortality of AKI in cardiac surgery patients (AuROC = 0.761).
Publication bias
Begg’s funnel plot was performed to access the publication bias of the literature. The shapes of the funnel plots revealed some evidence of obvious asymmetry. The funnel plot of the incidence of AKI in ICU patients and the incidence of AKI in cardiac patients were showed in Supplementary Figure 2 and 3, respectively.
Discussion
Acute kidney injury is very common with high hospital mortality in critically ill patients31, epidemiological studies demonstrate the wide variation in etiologies and risk factors, developing into chronic kidney disease and progression to dialysis dependency32,33. However, there is lack of a universally accepted and standardized definition for AKI for nephrologists and health care workers. The Acute Dialysis Quality Initiative’s RIFLE criteria has been validated in several clinical settings and shown to correlate with important outcomes, such as needing for renal replacement therapy (RRT), length of hospital stay and mortality22,34,35,36. But it is still imperfect. In 2007, the AKIN convened to refine the RIFLE criteria. A few modifications were added to AKI including the eliminating the change of glomerular filtration rate (GFR) and the outcome categories of Loss and ESRD; the stage 1 was redefined with an absolute increase in creatinine of at least 0.3 mg/dl; patients starting RRT are automatically classified as stage 3. Both the RIFLE and AKIN classifications use the changes of serum creatinine or urine output to establish the clinical syndrome of AKI in 3 severity levels. But whether the sensitivity of AKIN in the diagnosis of AKI in ICU patients has clinical significance, or the new classification can representative the severity of AKI patients and good predictive value for prognosis is not very clear.
A number of epidemiologic studies have tried to compare the RIFLE and AKIN criteria for the incidence and in-hospital mortality of AKI in critical ill patients and cardiac surgery patients12,13,14,25,27,28. Bagshaw and their college work revealed that the AKIN criteria do not improve the sensitivity and predictive ability of classification of AKI in the first 24 h after admission to ICU compared to the RIFLE criteria12. However, Ratanarat et al.23 found that AKIN criteria improved sensitivity for detection of AKI and prediction of in-hospital mortality was better than that of RIFLE criteria in critically ill patients with multi-organ dysfunction syndrome, Lopes et al.13, Zhang et al.17 and Jiang et al.16 showed that although AKIN criteria improved sensitivity of AKI diagnosis but does not improve ability in predicting in-hospital mortality of critically ill patients. In cardiac surgery patients, Haase et al.25 reported that the AKIN classification do not materially improve the clinical usefulness of RIFLE definition, however, Yan et al.26 found that the AKIN criteria seem not to have greater sensitivity and specificity compared with the RIFLE classification.
In the present study, 19 studies with more than 171,559 participants are included in our meta-analysis. We have consistently confirmed that patients with AKI, the RIFLE and AKIN classification is different for the incidence of AKI in ICU patients, the incidence of AKI diagnosed by AKIN classification is higher than the RIFLE classification, in subgroup analysis, we found that Risk vs. Stage 1 and Injury vs. Stage 2 were also different, but the Failure vs. Stage 3 did not show a statistical significance. This may be explained by the change criteria in stage 1 and the elimination of GFR, thus more patients were diagnosed as AKI by AKIN classification and there still some patients needs RRT for fluid overload were stratified in Stage 3 without increased serum creatinine which cannot be included in Failure stage by RIFLE. All this contributes to the high incidence of AKI by AKIN criteria. In cardiac surgery patients with AKI, the RIFLE and AKIN classification did not show difference for the diagnosis, only Injury vs. Stage 2 has a significant difference by subgroup analysis while the other stages did not. Comparing to cardiac surgery patients, the AKI incidence is higher in ICU patients, although some cardiac surgery patients were transferred to ICU. ICU is mixed with all kind of critical ill patients such as septic shock, acute respiratory distress syndrome, or hepatic cirrhosis. We also evaluated the in-hospital mortality and found that both RIFLE and AKIN criteria did not reach a significant difference to predict mortality, by subgroup analysis, only Risk VS. Stage 1 of AKI in ICU patients reached a significant difference. Thus, from our pooled analysis, our findings support the RIFLE or AKIN definition for AKI in ICU patients is different, but both classifications were not different for mortality. But we did find that both RIFLE and AKIN classification had a better predictive ability for cardiac surgery patients compared with ICU patients, which means that the predictive value for AKI related in-hospital mortality may different according to the different patients. This needs other patients to confirm our results.
In 2012, the Kidney Disease Improving Global Outcomes (KDIGO) Work Group proposed another definition that builds upon the AKIN definition, attempting to harmonize earlier consensus definitions and staging criteria for AKI. But Palevsky et al. thought that the KDIGO definition and staging criteria are appropriate for defining the epidemiology of AKI and is insufficient evidence to support their widespread application to clinical care in the United States37. A retrospective cohort study of 31,970 hospitalizations performed by Zeng et al.38 showed that AKI incidence was highest according to the KDIGO definition (18.3%) followed by the AKIN (16.6%) and RIFLE (16.1%). In addition, another retrospective observational study of 49,518 admissions indicated that 11.6% were diagnosed with KDIGO criteria, 11.0% were diagnosed with RIFLE criteria and only 4.8% were diagnosed with AKIN criteria39. In critically ill patients, KDIGO was more predictive than the RIFLE criteria, but there was no significant difference between AKIN and KDIGO40, Luo et al. found that the incidence of AKI using the RIFLE, AKIN and KDIGO criteria were 46.9%, 38.4% and 51%, respectively40. Moreover, for in-hospital mortality, only small differences in predictive abilities between RIFLE and KDIGO concerning clinical outcomes at 30 days in acute decompensated heart failure patients41. Therefore, all these definitions have their own limitation for wide accepted, new classification was needed to establish an early diagnosis of AKI that would be a simple and useful clinical tool.
The major limitation is that most of the included studies were retrospective and the AKI incidence was a large range in different medical center, which cause a heterogeneity. Second, some studies were multicenter which increased the weight in the meta-analysis. Third, we only evaluate the AKI in ICU and cardiac patients, the other diseases or syndromes associated acute kidney injury were not included in our meta-analysis. At last, A publication bias may have occurred. The funnel plot shows significant evidence of the bias (Supplementary Figures 2 and 3).
In conclusion, our study found that the AKIN criteria can identify more patients in classifying AKI in ICU patients compared to RIFLE criteria but not cardiac patients, for the prediction of AKI-related mortality, the AKIN criteria did not show a better ability in predicting hospital mortality in both ICU and cardiac surgery patients compared to RIFLE criteria. But both the RIFLE and AKIN classifications for AKI in cardiac surgery patients had better predictive ability compared with the ICU patients.
Materials and Methods
Data Sources, Search Strategy and Selection Criteria
We performed a systematic search to identify the studies examined the RIFLE and AKIN criteria for acute kidney injury. Literatures were identified by searching MEDLINE via Ovid, EMBASE, PubMed and China National Knowledge Infrastructure (CNKI) database. The last updated search was performed on November 1st, 2013. The searching terms were “Risk or Injury or Failure or RIFLE”, “AKIN or Acute Kidney Injury Network” and “acute renal failure or acute kidney injury or AKI”. We manually searched the references of the identified studies and review articles and academic congresses on kidney disease with available data were also included. The search was limited to compare the RIFLE and AKIN classification for AKI in ICU and cardiac surgery patients out without restriction on language.
Data extraction
Two authors independently extracted the information from all eligible publications using standard data extraction forms. Disagreement was resolved by discussion between the two authors, or the consultation with a third reviewer. The standardized data form was used for data collection, including first author, year of publication, country of origin, ethnicity of the study. The data of baseline serum creatinine, length of stay and renal replace therapy were recorded when available. All completed studies that compare AKI was defined and classified by the RIFLE criteria and the AKIN criteria in ICU or cardiac patients were eligible for inclusion.
Inclusion and Exclusion Criteria
The included studies met the following criteria: (1) Compare the AKIN classification with the RIFLE classification for acute kidney injury; (2) Age ≥16 years; (3) Patients were from ICU or cardiac surgery. Exclusion Criteria: (1) Age <16 years; (2) Length of stay less than 24 hours; (3) Patients with end-stage renal disease (ESRD) on chronic dialysis, prior ESRD or kidney transplant patients readmitted in hospital; (4) Renal allograft patients; (5) if serum creatinine data were not available either during the pre-specified time windows for AKI; (6) Data were unavailable for estimating odds ratio (OR) with 95% confidence interval (CI).
Evaluations of statistical associations
To summarize the incidence and hospital mortality of AKI patients diagnosed by the RIFLE criteria and AKIN criteria in published studies in adults, we looked at the pooled estimate of relative ratios (RRs) and 95% confidence intervals (CIs) were calculated for AKI patients with the two classifications. We also looked at the RRs comparing the three RIFLE classes Risk, Injury and Failure with AKIN stages (Risk VS. Stage 1, Injury VS. Stage 2 and Failure VS. Stage 3). Data were combined using a random effects model or fixed effects model according to the I2 test, I2 value 25%, 50% and 75% correspond to low, medium and high levels of heterogeneity, Fixed effects model was selected while the I2 under 50%, otherwise the a random effects model will be used42. Analysis was performed with Stata software, version 12. We used QUDAS II to evaluate the quality of the including studies and Asymmetry funnel plots were used to assess potential publication bias by Revman software, version 5.3. Model fit was assessed by the goodness of-fit test and discrimination was assessed by the area under the receiver operator characteristic (AuROC) curve (SPSS version 20). The p value less than 0.05 was considered as a statistical significance.
Additional Information
How to cite this article: Xiong, J. et al. The RIFLE versus AKIN classification for incidence and mortality of acute kidney injury in critical ill patients: A meta-analysis. Sci. Rep. 5, 17917; doi: 10.1038/srep17917 (2015).
References
Bellomo, R., Ronco, C., Kellum, J. A., Mehta, R. L. & Palevsky, P. Acute renal failure–definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 8, R204 (2004).
Bellomo, R., Kellum, J. A. & Ronco, C. Acute kidney injury. Lancet. 380, 756–766 (2012).
Chertow, G. M., Burdick, E., Honour, M., Bonventre, J. V. & Bates, D. W. Acute kidney injury, mortality, length of stay and costs in hospitalized patients. J Am Soc Nephrol. 16, 3365–3370 (2005).
De Mendonça, A. et al. Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med. 26, 915–921 (2000).
Uchino, S. et al. Acute renal failure in critically ill patients. J Am Med Assoc. 294, 813–818 (2005).
Leung, K. C., Tonelli, M. & James, M. T. Chronic kidney disease following acute kidney injury—risk and outcomes. Nat Rev Nephrol. 9, 77–85 (2012).
Susantitaphong, P. et al. World Incidence of AKI: A Meta-Analysis. Clin J Am Soc Nephrol. 8, 1482–1493 (2013).
Liangos, O. et al. Epidemiology and outcomes of acute renal failure in hospitalized patients: a national survey. Clin J Am Soc Nephrol. 1, 43–51 (2006).
Ricci, Z., Cruz, D. N. & Ronco, C. Classification and staging of acute kidney injury: beyond the RIFLE and AKIN criteria. Nat Rev Nephrol. 7, 201–208 (2011).
Ricci, Z. et al. Practice patterns in the management of acute renal failure in the critically ill patient: an international survey. Nephrol Dial Transpl. 21, 690–696 (2006).
Mehta, R. et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit care. 11, R31 (2007).
Bagshaw, S. M., George, C., Dinu, I. & Bellomo, R. A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol Dial Transpl. 23, 1203–1210 (2008).
Lopes, J. et al. Acute kidney injury in intensive care unit patients: a comparison between the RIFLE and the Acute Kidney Injury Network classifications. Crit Care. 12, R110 (2008).
Joannidis, M. et al. Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med. 35, 1692–1702 (2009).
Chang, C. et al. Acute kidney injury classification: comparison of AKIN and RIFLE criteria. Shock. 33, 247–52 (2010).
Jiang, F. et al. The sensitivity and accuracy of RIFLE and AKIN criteria for acute kidney injury diagnosis in intensive care unit patients. Chin Crit Care Med. 23, 759 (2011).
Zhang, J. et al. Comparison between the RIFLE and the Acute Kidney Injury Network Classifications in Diagnosis of Acute Kidney Injury. Chin Gen Prac. 7, 013 (2011).
Kim, W. Y., Huh, J. W., Lim, C. M., Koh, Y. & Hong, S. A comparison of acute kidney injury classifications in patients with severe sepsis and septic shock. Am J Med Sci. 344, 350–366 (2012).
Zhang, K., Zhou, J., Yang, L., Su, X. & Liu, Y. Comparative study to assess incidence and mortality of AKI patients in ICU by using AKIN and RIFLE criteria. J Clin Nephrol 12, 494–496 (2013)
Marinho1 A. D. & Gil R. M. A comparison of the RIFLE and AKIN criteria for acute kidney injury in critically ill patients. Intensive Care Med. 38, S47–48 (2012).
Huber W., Schneider J. & Saugel. B. Prediction of ICU-mortality and requirement of renal replacement therapy by RIFLE, AKIN and serum creatinine on admission in medical ICU patients. Intensive Care Med. 38, S262 (2012).
Tülübaş, E. K. et al. Monitoring of renal function in patients with RIFLE and AKIN scores to compare the effects on mortality and morbidity in ICU. Med J of Bakirkoy. 9, 69–72 (2013).
Ratanarat, R., Skulratanasak, P., Tangkawattanakul, N. & Hantaweepant, C. Clinical accuracy of RIFLE and Acute Kidney Injury Network (AKIN) criteria for predicting hospital mortality in critically ill patients with multi-organ dysfunction syndrome. J Med Assoc Thai. 96, S224–231 (2013).
Che M. et al. Comparison of RIFLE and AKIN diagnosis criteria for acute kidney injury in patients undergoing cardiac surgery. J Shanghai Jiaotong University (Medical Science) 29, 1214 (2009).
Haase, M. et al. A comparison of the RIFLE and Acute Kidney Injury Network classifications for cardiac surgery–associated acute kidney injury: a prospective cohort study. J Thorac Cardiovasc Surg. 138, 1370–1376 (2009).
Yan, X. et al. Acute kidney injury in adult postcardiotomy patients with extracorporeal membrane oxygenation: evaluation of the RIFLE classification and the Acute Kidney Injury Network criteria. Eur J Cardiothorac Surg. 37, 334–338 (2010).
Robert, A. M. et al. Cardiac surgery-associated acute kidney injury: a comparison of two consensus criteria. Ann Thorac Surg 90, 1939–1943 (2010).
Englberger, L. et al. Clinical accuracy of RIFLE and Acute Kidney Injury Network (AKIN) criteria for acute kidney injury in patients undergoing cardiac surgery. Crit care. 15, R16 (2011).
Bastin, A. J. et al. Acute kidney injury after cardiac surgery according to risk/injury/failure/loss/end-stage, acute kidney injury network and kidney disease: improving global outcomes classifications. J Crit Care. 28, 389–396 (2013).
Nina, V. J. d. S. et al. Acute kidney injury after coronary artery bypass grafting: assessment using RIFLE and AKIN criteria. Rev Bras Cir Cardiovasc. 28, 231–237 (2013).
Coca, S. G., Yusuf, B., Shlipak, M. G., Garg, A. X. & Parikh, C. R. Long-term risk of mortality and other adverse outcomes after acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 53, 961–973 (2009).
Wald, R. et al. Chronic dialysis and death among survivors of acute kidney injury requiring dialysis. J Am Med Assoc. 302, 1179–1185 (2009).
Abosaif, N. Y., Tolba, Y. A., Heap, M., Russell, J. & Nahas, A. The outcome of acute renal failure in the intensive care unit according to RIFLE: model application, sensitivity and predictability. Am J Kidney Dis. 46, 1038–1048 (2005).
Lopes, J. A. et al. Prognostic utility of RIFLE for acute renal failure in patients with sepsis. Crit Care. 11, 408 (2007).
Lin, C. et al. RIFLE classification is predictive of short-term prognosis in critically ill patients with acute renal failure supported by extracorporeal membrane oxygenation. Nephrol Dial Transpl. 21, 2867–2873 (2006).
Ricci, Z., Cruz, D. & Ronco, C. The RIFLE criteria and mortality in acute kidney injury: a systematic review. Kidney Int. 73, 538–546 (2008).
Palevsky, P. M. et al. KDOQI US Commentary on the 2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury. Am J Kidney Dis. 61, 649–672 (2013).
Zeng, X., McMahon, G. M., Brunelli, S. M., Bates, D. W. & Waikar, S. S. Incidence, outcomes and comparisons across definitions of AKI in hospitalized individuals. Clin J Am Soc Nephrol. 9, 12–20 (2014).
Fujii, T., Uchino, S., Takinami, M. & Bellomo, R. Validation of the Kidney Disease Improving Global Outcomes criteria for AKI and comparison of three criteria in hospitalized patients. Clin J Am Soc Nephrol. 9, 848–854 (2014).
Luo, X. et al. A comparison of different diagnostic criteria of acute kidney injury in critically ill patients. Crit Care. 18, R144 (2014).
Roy, A. K. et al. A comparison of traditional and novel definitions (RIFLE, AKIN and KDIGO) of acute kidney injury for the prediction of outcomes in acute decompensated heart failure. Cardiorenal Med. 3, 26–37 (2013).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. Brit Med J. 327, 557 (2003).
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Xiong, J., Tang, X., Hu, Z. et al. The RIFLE versus AKIN classification for incidence and mortality of acute kidney injury in critical ill patients: A meta-analysis. Sci Rep 5, 17917 (2015). https://doi.org/10.1038/srep17917
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep17917
This article is cited by
-
Balanced crystalloid solutions versus normal saline in intensive care units: a systematic review and meta-analysis
International Urology and Nephrology (2023)
-
Pre-operative kidney biomarkers and risks for death, cardiovascular and chronic kidney disease events after cardiac surgery: the TRIBE-AKI study
Journal of Cardiothoracic Surgery (2022)
-
Risk estimation model for acute kidney injury defined by KDIGO classification after heart valve replacement surgery
General Thoracic and Cardiovascular Surgery (2020)
-
A new scoring model for the prediction of mortality in patients with acute kidney injury
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.