Abstract
This study investigated interactive effects of CYP2B6 genotypes and liver metastasis on the prognosis of metastatic breast cancer patients who received combined chemotherapy of docetaxel and thiotepa. Totally 153 patients were retrospectively genotyped rs8192719 (c.1294 + 53C > T) and rs2279343 (c.785A > G). Kaplan-Meier method and Cox Proportional Hazard Regression model were used to estimate the survival. Patients with liver metastasis had worsen prognosis, conferring a 2.26-fold high risk of progression and 1.93-fold high risk of death (p < 0.05). Both CT/TT genotype of rs8192719 (c.1294 + 53C > T) and AG genotype of rs2279343 (c.785A > G) prolonged survival (p < 0.05). Furthermore, among liver metastatic patients, AG genotype of rs2279343 (c.785A > G) was associated with a 47% reduced risk of death and a 6-month-longer overall survival (p < 0.05). Among non-liver metastatic patients, hazard ratios of CT/TT genotype of rs8192719 (c.1294 + 53C > T) were 0.45 for progression and 0.40 for death; and the corresponding survival was improved by 6 months and 16 months, respectively (p < 0.05). Genotypes of CYP2B6 had an interaction with clinical efficacy of docetaxel and thiotepa on metastatic breast cancer patients; and metastatic sites also affected clinical responses. Further therapies should take into account of chemotherapy regimen, genotypes of metabolizing enzymes and metastatic sites for the particular subpopulation.
Similar content being viewed by others
Introduction
Metastasis has become the leading causes for death among breast cancer patients. More and more evidence has supported that brain, liver and lung metastases are lethal. The apparent variations in clinical responses among metastatic breast cancer (MBC) patients treated with various salvage chemotherapy remain unclear1,2. We have explored specific chemotherapeutics of docetaxel and thiotepa [targeting liver metastasis (LM)] in MBC patients who had developed resistance to previous anthracycline and paclitaxel. It was believed that docetaxel plus thiotepa were efficient for liver metastasis3. Thiotepa could be rapidly metabolized by cytochrome P450 (CYP450) into its main metabolite tepa through oxidative desulfuration and generation of regional cytotoxicity in metastatic liver lesions4. We therefore recommended that docetaxel plus thiotepa could be optimally recommended as specific targeted-therapy for liver metastasis3. More recently, we have found the new biological activities of thiotepa in killing breast cancer stem cells5. Since CYP2B6 is a phase I xenobiotics metabolizing enzyme, a member of the cytochrome P450 superfamily6 capable of catalyzing the reaction of thiotepa, we postulated the genetic effects of single nucleotide polymorphisms (SNPs) on clinical outcome of MBC individuals treated with docetaxel and thiotepa. Two SNPs at rs8192719 (c.1294 + 53C > T) and rs2279343 (c.785A > G) in CYP2B6 gene were targeted and explored the clinical efficacy7,8. CT/TT genotype of rs8192719 (c.1294 + 53C > T) and AG genotype of rs2279343 (c.785A > G) led to a reduced metabolizing activity of CYP2B6 enzyme9. The primary endpoint of this study was the interactions of CYP2B6 genotypes with metastatic sites on the prognosis for MBC.
Patients and Methods
Selection of Patients
To be eligible for this study, patients must meet the following criteria: female, aged ≥18 years, histological proven MBC, previous treatment with anthracycline and paclitaxel, no previous treatment with docetaxel or thiotepa, Eastern Cooperative Oncology Group (ECOG) performance status of 0–2, at least one measurable lesion, adequate hepatic (serum bilirubin ≤1.5× upper normal limit and aspartate aminotransferase and alanine aminotransferase ≤1.5× upper normal limit), renal (serum creatinine ≤1.5× upper normal limit) and bone marrow (neutrophils ≥1.5 × 103/μl, platelets ≥100 × 103/μl and hemoglobin ≥10 g/dl) functions, normal electrocardiogram, expected life expectancy of more than 3 months, no pregnancy or lactation, no serious or uncontrolled concurrent medical illness and no history of other malignancies. Chemotherapy, radiotherapy and hormonal therapy were all permitted provided that 4 weeks had passed prior to the study.
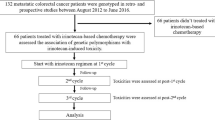
This study, which was registered at ClinicalTrials.gov (NCT01199393), was approved by ethnic committee of Peking University Cancer Hospital. From Aug 31 2010 to Dec 31 2014, each patient who participated in the study had signed an informed consent. Totally, 153 patients were recruited eligibly into the study and detected polymorphisms of CYP2B6. The experiments were performed in accordance with the approved guideline and regulation.
Therapeutic protocols
This was an open-label and prospective study3. Docetaxel 35 mg/m2 was administered in 100 ml of 0.9% sodium chloride over 30 minutes, followed by thiotepa 30 mg/m2 in 250 ml of 0.9% sodium chloride over 30 minutes. Both drugs were given intravenously on days 1 and 8, every 21 days for two cycles at least. Premedication of dexamethasone 7.5 mg by mouth twice daily was administered on the day before docetaxel infusion and continued for a total of 3 days. 5-hydroxytryptamine-3 receptor antagonists were systematically administered to prevent emesis. Patients were scheduled to receive a maximum of 8 cycles and chemotherapy was stopped in case of disease progression, patient refusal, or unacceptable toxicity. Adverse events were classified according to National Cancer Institute Common Toxicity Criteria (NCI-CTC) version 3.010.
Genotyping of CYP2B6 genetic polymorphisms
Genomic DNA was extracted from venous blood samples (4 ml) drawn before drug administration, using standard phenol-chloroform method. Polymorphism of rs8192719 (c.1294 + 53C > T) was genotyped by matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry method (Sequenom, Inc., San Diego) and rs2279343 (c.785A > G) was genotyped by polymerase chain reaction (PCR) and direct sequencing11. All samples were processed and analyzed by Beijing Genome Institute (BGI). To verify the results, 5% of the DNA samples were randomly selected for duplicate assays. All the results were generated and analyzed by laboratory staff unaware of patient status.
Statistical Analysis
All data were analyzed by SPSS for windows version 15.0 (SPSS Inc., Chicago, IL, USA). Progression-free survival (PFS) and overall survival (OS) were estimated by Kaplan-Meier method. In the univariate analyses, the categorical variables between metastatic status and variant genotypes were analyzed by Chi-square test and the continuous variables were analyzed by t-test. The variables included age, estrogen receptor (ER) (negative vs. positive), progestin receptor (PR) (negative vs. positive), human epidermal growth factor receptor-2 (HER2) (negative vs. positive), menopausal status (pre- vs. post-) and chemotherapy (1st, 2nd, vs. ≥ 3rd line).
The Kaplan-Meier survival curve of PFS and OS were estimated for liver metastasis and genotypes with log-rank tests. The significant variables in log-rank tests were further analyzed by Cox Proportional Hazard Regression Models with confounder adjustment (age, menopause, ER, PR, HER2 status and chemotherapy). All tests were two-tailed and the significant level was a p value of ≤0.05.
Results
Patients’ Characteristics
During the follow-up period, 134 patients had disease progressed and 100 patients died. 65 patients had LM and 88 patients had metastases involved other organs. The mean age of MBC patients with LM was 51.1 years old, 4 years younger than the other metastatic patients (p < 0.05) (Table 1). Between the patients with liver and other sites metastases, the frequencies of menopausal, ER, PR, HER2 status and molecular subtypes as well as chemotherapy were similar (p > 0.05) (Table 1). Between genotypes of rs8192719 (c.1294 + 53C > T) and rs2279343 (c.785A > G), all demographic and clinical factors distributed similarly (p > 0.05) (Table 2).
Survival
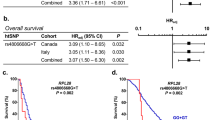
The LM patients had a shorter survival than those with other metastatic sites (Fig. 1). PFS was 4.20 months in LM patients, nearly 4-month shorter than other metastatic patients and the HR of LM was 2.26 (95% CI, 1.53–3.36) (Table 3). OS of LM patients was 14.20 months, in contrast with 25.40 months in other metastatic patients (Table 3). LM produced a 93% increased risk for death (HR = 1.93, 95% CI, 1.26–2.95) (Table 3).
The CT/TT genotypes of rs8192719 (c.1294 + 53C > T) introduced longer survival time than the CC genotype in MBC patients (Fig. 2). PFS of CT/TT genotypes was 7.70 months, 1.7-month longer than CC genotype and the HR of CT/TT genotypes was 0.62 for progression (95% CI, 0.50–0.94) (Table 3). Patients with CT/TT genotypes of rs8192719 (c.1294 + 53C > T) had the OS of 27.50 months compared to 17.90 months in CC genotype (p < 0.05); HR of CT/TT genotypes for death reduced to 0.52 (95% CI, 0.32–0.85) (Table 3).
The AG genotype of rs2279343 (c.785A > G) produced a longer OS than the AA genotype (Fig. 3). OS in patients harboring the AG genotype was 24.80 months, 12-month longer than the AA genotype (p < 0.05); the corresponding risk for death was reduced by 46% (HR = 0.54, 95% CI, 0.35–0.84) (Table 3).
Interactive effects of LM and SNPs
PFS was similar between the CT/TT and CC genotypes of rs8192719 (c.1294 + 53C > T) among LM patients, however, among other metastatic patients, CT/TT genotypes had a PFS of 11.40 months, 3.8 month longer than CC genotype; and a 55% reduced risk of progression (HR = 0.45, 95% CI, 0.24–0.86) (Table 4). OS of other organ metastasis patients with CT/TT genotypes of rs8192719 (c.1294 + 53C > T) was 7.4 month longer than CC genotype, with a HR of 0.40 (95% CI, 0.17–0.91) for death (Table 5). OS in LM patients with the AG genotype of rs2279343 (c.785A > G) was longer than the AA genotype (14.90 vs. 9.40 months) and related with a death risk reduced by 47% (95% CI, 0.29–0.98) (Table 5).
Discussion
The emerging concept of precise and personalized medicine has been recently proposed world widely, which enables us to apply chemotherapeutic protocols tailored with individual genetic identity. Significant heterogeneity in drug response can be observed in the clinical practice. Unfortunately, there is no reliable biomarker to help to select patients who are most likely to benefit from the specific treatment whereas save others from unnecessary toxicities produced by ineffective treatments. Although factors such as age, organ functions and tumor biology can explain different drug responses to a certain extent, genetic constitutions are reported to account for 20% to 95% of this variability12,13. A growing number of literatures suggest that genetic polymorphisms (e.g., SNPs) in metabolizing enzymes may be a major determinant of drug response14. In addition, SNPs in CYP450 may play a critical role since the enzyme is involved in metabolisms of about 80% of all phase I drugs15. Therefore, it is reasonable to hypothesize that those SNPs in CYP450 influence clinical outcome of docetaxel/thiotepa regimen. Our previous study on docetaxel plus capecitabine versus docetaxel plus thiotepa as ≥2nd-line chemotherapy in the MBC patients showed similar clinical responses and tolerable toxicities3.
Our present study indicated that docetaxel plus thiotepa was effective and safe for MBC patients, with the median PFS of 6.5 months and median OS of 20.0 months. It was comparable to other docetaxel-containing regimens for MBC16,17,18,19,20. Interestingly, liver metastatic patients had reduced PFS and OS than other metastatic patients and the poorer survival of liver metastasis was presented from previous studies21,22. Liver has been appointed as the centralized site responsible for maintain the physiologically drug metabolism to deliver the active compound into the circulation. Liver function detained from hepatocytes from extraordinary toxic exposures, Patients who appeared by a lowered albumin and an elevated bilirubin levels ignited the onset of liver failure, leading to a poor clinical outcome22. Decompensation of liver function was observed to be related with a poor outcome among MBC patients regardless of any exposures to treatments23. Metastasis damaged liver function and produced a poor survival among the patients.
Docetaxel is a well-established anti-mitotic medication used mainly for the treatment of breast cancer for more than decade24. Thiotepa is a traditionally alkylating antineoplastic agent used for breast cancer and bladder cancer etc25. The data from our group showed the combination of docetaxel with thiotepa has been reported to obtain an optimistic outcome in MBC patients26. CYP2B6 is a phase I xenobiotics metabolizing enzyme and a member of the cytochrome P450 superfamily6. CYP2B6 as a monooxygenase, participates in drug metabolism and synthesis of some lipids6. The enzyme metabolizes several anti-cancer drugs, such as cyclophosphamide and thiotapa4,6. CYP2B6 first metabolizes thiotepa to tapa and then phase II drug-metabolizing enzymes (GSTA1/P1) catalyze tepa to monoglutathionlytepa4. CT/TT genotypes of rs8192719 (c.1294 + 53C > T) and AG genotype of rs2279343 (c.785A > G) caused a decreased metabolizing activity of CYP2B69. A low metabolizing activity of CYP2B6 resulted in a high exposure to thiopeta and tepa4,9. The decreased activity of drug-metabolizing enzyme was possible to introduce an increase in drug exposure and then an optimistic survival was observed among patients of CT/TT genotypes of rs8192719 (c.1294 + 53C > T) and AG genotype of rs2279343 (c.785A > G).
Due to the metabolism properties of thiotepa which could be converted into tepa in the liver, we were interested in testifying the feasibility of applying a specific chemotherapeutic regimen for patients with liver metastases. In this study, AG genotype of rs2279343 (c.785A > G) was associated with longer OS among liver metastatic MBC patients, however, CT/TT genotype of rs8192719 (c.1294 + 53C > T) was associated with longer PFS and OS among non-liver metastatic MBC patients. The docetaxel plus thiotepa regimen had a better efficacy to patients with AG genotype of rs2279343 (c.785A > G) and liver metastasis, as well as the patients with the CT/TT genotype of rs8192719 (c.1294 + 53C > T) and metastases to organs other than liver.
Conclusions
The regimen of combined docetaxel and thiotepa achieved a better prognosis among MBC patient harboring AG genotype of rs2279343 (c.785A > G) and CT/TT genotype of rs8192719 (c.1294 + 53C > T). Liver metastasis conferred a worse survival than metastases other than liver. Under docetaxel and thiotepa regimen, AG genotype of rs2279343 (c.785A > G) correlated with a better prognosis among liver metastatic patients, whereas CT/TT genotype of rs8192719 (c.1294 + 53C > T) favored other-than-liver metastatic patients. The chemotherapy regimen, together with genetic polymorphisms of drug-metabolizing enzymes as well as metastatic sites should be taken into account in precise medicine.
Additional Information
How to cite this article: Song, Q. et al. The prognostic values of CYP2B6 genetic polymorphisms and metastatic sites for advanced breast cancer patients treated with docetaxel and thiotepa. Sci. Rep. 5, 16775; doi: 10.1038/srep16775 (2015).
References
Bevers, T. B. et al. NCCN clinical practice guidelines in oncology: breast cancer screening and diagnosis. Journal of the National Comprehensive Cancer Network: JNCCN 7, 1060–1096 (2009).
Beslija, S. et al. Second consensus on medical treatment of metastatic breast cancer. Annals of oncology: official journal of the European Society for Medical Oncology/ESMO 18, 215–225, 10.1093/annonc/mdl155 (2007).
Yu, J. et al. [Randomized clinical case-control trial for the comparison of docetaxel plus thiotepa versus docetaxel plus capecitabine in patients with metastatic breast cancer]. Beijing da xue xue bao. Yi xue ban = Journal of Peking University. Health sciences 43, 151–156 (2011).
Ekhart, C. et al. Polymorphisms of drug-metabolizing enzymes (GST, CYP2B6 and CYP3A) affect the pharmacokinetics of thiotepa and tepa. British journal of clinical pharmacology 67, 50–60, 10.1111/j.1365-2125.2008.03321.x (2009).
Lu, Z. et al. DNA methyltransferase inhibitor CDA-2 synergizes with high-dose thiotepa and paclitaxel in killing breast cancer stem cells. Frontiers in bioscience (Elite edition) 3, 240–249 (2011).
Gene. CYP2B6 cytochrome P450, family 2, subfamily B, polypeptide 6 [Homo sapiens (human)]. Available from: http://www.ncbi.nlm.nih.gov/gene/1555. Accessed on 09/11/2014.
NCBI. dbSNP Short Genetic Variations. Reference SNP Cluster Report: rs2279343. Available from: http://www.ncbi.nlm.nih.gov/projects/SNP/snp_ref.cgi?rs=2279343 Accessed on 09/22/2015.
NCBI. dbSNP Short Genetic Variations. Reference SNP Cluster Report: rs8192719. Available from: http://www.ncbi.nlm.nih.gov/SNP/snp_ref.cgi?searchType=adhoc_search&type=rs&rs=rs8192719 Accessed on: 09/22/2015.
Dobrinas, M. et al. Contribution of CYP2B6 alleles in explaining extreme (S)-methadone plasma levels: a CYP2B6 gene resequencing study. Pharmacogenetics and genomics 23, 84–93, 10.1097/FPC.0b013e32835cb2e2 (2013).
National Cancer Institute. Cancer Therapy Evaluation Program. Common Terminology Criteria for Adverse Events (CTCAE) v3.0. Available from: http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf Accessed on: 09/22/2015.
Blievernicht, J. K. et al. MALDI-TOF mass spectrometry for multiplex genotyping of CYP2B6 single-nucleotide polymorphisms. Clinical chemistry 53, 24–33, 10.1373/clinchem.2006.074856 (2007).
Ingelman-Sundberg, M., Sim, S. C., Gomez, A. & Rodriguez-Antona, C. Influence of cytochrome P450 polymorphisms on drug therapies: pharmacogenetic, pharmacoepigenetic and clinical aspects. Pharmacology & therapeutics 116, 496–526, 10.1016/j.pharmthera.2007.09.004 (2007).
Watson, R. G. & McLeod, H. L. Pharmacogenomic contribution to drug response. Cancer journal (Sudbury, Mass.) 17, 80–88, 10.1097/PPO.0b013e3182147432 (2011).
Eichelbaum, M., Ingelman-Sundberg, M. & Evans, W. E. Pharmacogenomics and individualized drug therapy. Annual review of medicine 57, 119–137, 10.1146/annurev.med.56.082103.104724 (2006).
Ingelman-Sundberg, M. Pharmacogenetics of cytochrome P450 and its applications in drug therapy: the past, present and future. Trends in pharmacological sciences 25, 193–200, 10.1016/j.tips.2004.02.007 (2004).
Stemmler, H. J. et al. Randomised phase II trial of gemcitabine plus vinorelbine vs gemcitabine plus cisplatin vs gemcitabine plus capecitabine in patients with pretreated metastatic breast cancer. British journal of cancer 104, 1071–1078, 10.1038/bjc.2011.86 (2011).
Ciruelos, E. M. et al. Gemcitabine and capecitabine in previously anthracycline-treated metastatic breast cancer: a multicenter phase II study (SOLTI 0301 trial). Annals of oncology: official journal of the European Society for Medical Oncology / ESMO 21, 1442–1447, 10.1093/annonc/mdp536 (2010).
Finek, J. et al. A phase II trial of oral vinorelbine and capecitabine in anthracycline pretreated patients with metastatic breast cancer. Anticancer research 29, 667–670 (2009).
Lee, S. H. et al. Capecitabine monotherapy in patients with anthracycline- and taxane-pretreated metastatic breast cancer. Medical oncology (Northwood, London, England) 21, 223–231, 10.1385/mo:21:3:223 (2004).
Chan, S. et al. Phase III study of gemcitabine plus docetaxel compared with capecitabine plus docetaxel for anthracycline-pretreated patients with metastatic breast cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 27, 1753–1760, 10.1200/jco.2007.15.8485 (2009).
Baur, M., Schlappack, O., Havelec, L., Wrba, F. & Dittrich, C. Prognostic significance of liver metastases as first site of generalisation in patients with breast cancer–a retrospective analysis. Acta medica Austriaca 28, 135–140 (2001).
Wyld, L. et al. Prognostic factors for patients with hepatic metastases from breast cancer. British journal of cancer 89, 284–290, 10.1038/sj.bjc.6601038 (2003).
O’Reilly, S. M., Richards, M. A. & Rubens, R. D. Liver metastases from breast cancer: the relationship between clinical, biochemical and pathological features and survival. European journal of cancer (Oxford, England: 1990) 26, 574–577 (1990).
PubChem Compound. Docetaxel. Available from: http://pubchem.ncbi.nlm.nih.gov/summary/summary.cgi?cid=148124&loc=ec_rcs#x94 Accessed on: 09/11/2014.
US Dept. of Health and Human Services, Public Health Service, National Toxicology Program. Thiotepa. Report on carcinogens: carcinogen profiles/US Dept. of Health and Human Services, Public Health Service, National Toxicology Program 12, 406–407 (2011).
Ren, J. et al. Selections of appropriate regimen of high-dose chemotherapy combined with adoptive cellular therapy with dendritic and cytokine-induced killer cells improved progression-free and overall survival in patients with metastatic breast cancer: reargument of such contentious therapeutic preferences. Clinical & translational oncology : official publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico 15, 780–788, 10.1007/s12094-013-1001-9 (2013).
Acknowledgements
We thank Dr. Sherry Gu Ph.D. from Duke Clinical Research Institute, Duke University, Durham, NC and Professor Subhashis Ghoshal from Department of Statistics, North Carolina State University, USA for their assistance with the statistical analysis. This work was supported by Natural Science Foundation of China (No. 81172534), Suan G Komen for Cure Foundation (No. SPCHIN1201) and Youth Foundation of Beijing Shijitan Hospital (No. 2013-q-04).
Author information
Authors and Affiliations
Contributions
Q.K.S., J.R. and K.L. prepared, revised and approved the manuscript. J.Y., N.N.D., X.N.Z., X.L.W. and H.B.Y. collected the data and blood sample. Q.K.S., X.N.Z. and X.L.W. analyzed the data. Q.K.S. and J.R. prepared the tables and figures.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Song, Q., Zhou, X., Yu, J. et al. The prognostic values of CYP2B6 genetic polymorphisms and metastatic sites for advanced breast cancer patients treated with docetaxel and thiotepa. Sci Rep 5, 16775 (2015). https://doi.org/10.1038/srep16775
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep16775
This article is cited by
-
Sequencing of genes of drug response in tumor DNA and implications for precision medicine in cancer patients
The Pharmacogenomics Journal (2023)
-
Single-nucleotide polymorphisms and the effectiveness of taxane-based chemotherapy in premenopausal breast cancer: a population-based cohort study in Denmark
Breast Cancer Research and Treatment (2022)
-
Circulating DNA as prognostic biomarker in patients with advanced hepatocellular carcinoma: a translational exploratory study from the SORAMIC trial
Journal of Translational Medicine (2019)
-
CYP1A1 genetic polymorphism is a promising predictor to improve chemotherapy effects in patients with metastatic breast cancer treated with docetaxel plus thiotepa vs. docetaxel plus capecitabine
Cancer Chemotherapy and Pharmacology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.