Abstract
The impact of ribavirin (RBV) dosage on sustained virologic response (SVR) rates remains elusive in hepatitis C virus genotype 2 (HCV-2) rapid responders receiving 16 weeks of peginterferon (Peg-IFN) plus RBV. Treatment-naïve HCV-2 patients with rapid virologic response (RVR) received Peg-IFN alfa-2a 180 μg/week plus weight-based RBV (1,000 or 1,200 mg/day; cut-off body weight: 75 kg) for 6 weeks and then randomly received Peg-IFN alfa-2a 180 μg/week plus weight-based (1,000 or 1,200 mg/day; n = 247) or flat-dose (800 mg/day; n = 246) RBV for additional 10 weeks. The primary endpoint was SVR24. Patients receiving weight-based and flat-dose RBV therapies had comparable SVR24 rates (93.5% versus 91.9%, P = 0.49). The risk differences (RDs) of SVR24 receiving weight-based and flat-dose RBV arms were 7.1% [95% CI: 0.7% to 13.6%] in males and −5.8% [95% CI: −12.1% to 0.5%] in females (interaction P = 0.01). The SVR24 rate was higher in males receiving ≥13 mg/kg/day than those receiving <13 mg/kg/day (96.3% versus 85.1%, P = 0.001). In conclusion, Peg-IFN alfa-2a plus weight-based or flat-dose RBV for 16 weeks provides comparable SVR24 rates in treatment-naïve HCV-2 rapid responders. However, males should receive weight-based RBV to achieve a high SVR24 rate.
Similar content being viewed by others
Introduction
Hepatitis C virus (HCV) infection remains the leading cause of cirrhosis, hepatic decompensation, hepatocellular carcinoma (HCC) and liver transplantation1. While HCV genotype 2 (HCV-2) infection is relatively uncommon in North America and West Europe (except for Northern Italy), it is common in East Asia2,3,4. In the era of peginterferon (Peg-IFN) plus ribavirin (RBV) therapy, the SVR rates in patients with HCV-2/3 infection are higher (75–95% versus 39–79%) than those in patients with HCV-1/4 infection5,6,7,8,9,10,11,12. Although the safety and efficacy of the recently introduced sofosbuvir-based therapies are excellent for HCV-2 patients, the treatment costs and the drug availability preclude the unselected use of these agents13,14,15,16,17.
In HCV-2 patients who receive Peg-IFN plus RBV and who achieve rapid virologic response (RVR), the SVR rates are comparable if they receive 12–16 weeks or 24 weeks of therapy18,19. The SVR rates are also similar in these patients with different interleukin-28B (IL-28B) genotypes20,21,22. However, the impact of weight-based (1,000 or 1,200 mg/day) or flat-dose (800 mg/day) RBV on the SVR rates in HCV-2 patients achieving RVR remains controversial12,23,24. For HCV-2 patients achieving RVR after 6 weeks of induction therapy by Peg-IFN alfa-2a plus weight-based RBV, we aimed to compare the efficacy of additional 10 weeks of therapy by Peg-IFN alfa-2a plus weight-based or flat-dose RBV and to evaluate the factors associated with anti-viral responses.
Results
Patient Characteristics
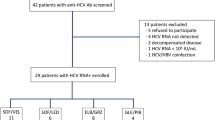
Among 495 patients who achieved RVR after 6 weeks of Peg-IFN alfa-2a plus weight-based RBV induction therapy, 493 were allocated at week 6 of treatment to receive Peg-IFN alfa-2a plus weight-based (n = 247) or flat-dosed (n = 246) RBV for additional 10 weeks. Two hundred and forty (97.2%) patients and 240 (97.6%) patients in weight-based and flat-dose RBV arms completed the assigned treatment, respectively. In addition, 234 (94.7%) patients and 230 (93.5%) patients in these two arms completed off-therapy follow-up to assess SVR24 (Fig. 1). The baseline patient characteristics were comparable between the two arms (Table 1). Most patients had baseline viral load of ≤800,000 IU/mL (79%) and favorable interleukin-28B (IL-28B) rs8099917 genotype (87%) and were infected with 2a subtype (75%). With regard to aspartate aminotransferase (AST) to platelet ratio index (APRI) score, 23.7% of the patients had a score of >2.00.
Efficacy
The end-of-treatment virologic response (ETVR) (100.0% versus 99.6%, risk difference (RD): 0.4% [95% confidence interval (CI): −0.7% to 1.5%]; P = 0.50) and the SVR24 rates (93.5% versus 91.9%, RD: 1.7% [95% CI: −2.9% to 6.2%]; P = 0.49) were comparable between the weight-based and flat-dose RBV arms (Table 2).
We performed the sensitivity analyses to assess the impact of 6 and 9 patients who failed to achieve SVR24 due to undetermined reason in weight-based and flat-dose RBV arms (Table 2). As a best-case scenario, we assumed that the 6 patients in weight-based RBV arm who achieved SVR24 and the 9 patients in flat-dose RBV arm who failed to achieve SVR24. As a worst-case scenario, we assumed that the 6 patients in weight-based RBV arm who failed to achieve SVR24 and the 9 patients in flat-dose RBV arm who achieved SVR24. Results from the best-case scenario (96.0% versus 91.9%, RD: 4.1% [95% CI: −0.1% to 8.3%]; P = 0.10) and the worst-case scenario (93.5% versus 95.5%, RD: −2.0% [95% CI: −6.0% to 2.0%]; P = 0.43) were consistent with the primary endpoint.
Subgroup Analyses for Prespecified Factors
Differences of the SVR24 rates between weight-based and flat-dose RBV arms did not vary by baseline viral load (interaction P = 0.33), subgenotype (interaction P = 0.61), IL-28B rs8099917 genotype (interaction P = 0.99), age (interaction P = 0.18), weight (interaction P = 0.71), APRI score (interaction P = 0.11), RBV dosage (interaction P = 0.88) or 80/80/80 rule (interaction P = 0.64) (Table 3). Compared with females (91.3% versus 97.1%, RD: −5.8% [95% CI: −12.1% to 0.5%]), males in weight-based RBV arm achieved a greater SVR24 rate than those in flat-dose RBV arm (95.1% versus 88.0%, RD: 7.1% [95% CI: 0.7% to 13.6%]; interaction P = 0.01).
We further examined the daily RBV exposure in males and females receiving weigh-based and flat-dose RBV. Compared to patients in flat-dose RBV arm, those in weight-based RBV arm received a greater RBV dosage (15.4 mg/kg/day [SD, 2.6] versus 12.9 mg/kg/day [SD, 2.1], P < 0.001), regardless of males (14.4 mg/kg/day [SD, 1.9] versus 12.4 mg/kg/day [SD. 2.0], P < 0.001) or females (16.8 mg/kg/day [SD, 2.9] versus 13.6 mg/kg/day [SD, 2.1], P < 0.001). Patients receiving RBV at a dosage of ≥13 mg/kg/day had a greater SVR24 rate than those receiving RBV at a dosage of <13 mg/kg/day (95.7% versus 87.1%, P = 0.001). While the SVR24 rates were similar in females receiving RBV at a dosage of ≥13 and <13 mg/kd/day (94.3% versus 93.9%, P = 0.99), the SVR24 rate in males receiving RBV at a dosage of ≥13 mg/kg/day was greater than those receiving RBV at a dosage of <13 mg/kg/day (97.0% versus 84.3%, P < 0.001) (Table 4).
Safety
The constitutional and laboratory adverse events (AEs) were similar between two arms (Table 5). Two patients in weight-based RBV arm and one in flat-dose RBV arm had serious AEs during treatment (0.8% versus 0.4%, RD: 0.4% [95% CI: −1.0% to 1.8%]). The AE-related withdrawal rates were 2.8% in weight-based RBV arm and 2.4% in flat-dose RBV arm (RD: 0.4% [95% CI: −2.4% to 3.2%]). During the first 6 weeks of treatment, 6.1% and 6.5% of the patients receiving weight-based and flat-dose RBV had anemia (RD: −0.4% [95% CI: −3.9% to 4.7%]). Furthermore, 20.2% and 15.0% of the patients receiving weight-based and flat-dose RBV had anemia (RD: 5.2% [95% CI: −1.5% to 11.9%]) between weeks 6 and 16 of treatment.
Discussion
Our study demonstrated that Peg-IFN alfa-2a plus weight-based or flat-dose RBV for 16 week provided high SVR24 rates in HCV-2 rapid responders. The SVR24 rates in our patients (91.9% to 93.5%) were greater than those in HCV-2 slow responders receiving 24–48 weeks of Peg-IFN plus RBV therapy (46.2% to 52.6% for 24 weeks; 71.4% for 36 weeks; 68.4% to 77.8% for 48 weeks), suggesting that the early viral kinetics play an important role in determining the anti-viral responses in these patients25,26,27. Furthermore we also showed that treatment with Peg-IFN alfa-2a plus weight-based RBV provided a comparable SVR24 rate (93.5% versus 91.9%) and treatment-related withdrawal rate (2.8% versus 2.4%) to treatment with Peg-IFN alfa-2a plus flat-dose RBV, suggesting HCV-2 rapid responders may receive Peg-IFN plus flat-dose RBV for 16 weeks to achieve high a SVR rate and a low AE rate. While the SVR24 rates were similar in females in weight-based and flat-dose RBV arms (91.3% versus 97.1%), the SVR24 rate was greater in males receiving Peg-IFN alfa-2a plus weight-based RBV than that in males receiving Peg-IFN alfa-2a plus flat-dose RBV (95.1% versus 88.0%).
Although the SVR24 rates between weight-based and flat-dose RBV arms were similar stratified by baseline viral load, subgenotype, IL-28B genotype, age, weight, APRI score, RBV dosage or 80/80/80 rule, males in weight-based RBV arm achieved a significant greater SVR rate than those in flat-based RBV arm. We further examined the possible factors for the gender effects. The mean dosage of RBV in weight-based RBV arm was significantly greater than flat-dose RBV arm, regardless of gender. When we stratified the RBV dosage at a cut-off value of 13 mg/kg/day, we revealed that males with a RBV dosage of ≥13 mg/kg/day had a greater SVR24 rate than those with a dosage of <13 mg/kg/day, but the SVR24 rates in females were similar whether they received a RBV dosage of ≥13 mg/kg/day or not. Manns et al. demonstrated that the SVR24 rate tended to increase in HCV-infected patients if they received a RBV dosage of ≥13 mg/kg/day5. Our study implied that although males who achieved RVR after induction therapy with Peg-IFN alfa-2a plus weight-based RBV, a sufficiently high dosage of RBV (≥13 mg/kg/day) should be maintained to secure a high SVR rate if they received a truncated treatment duration for 16 weeks. In females who achieved RVR after Peg-IFN alfa-2a plus weight-based RBV induction therapy, flat-dose RBV therapy may be preferred at treatment weeks 6–16 because it did not compromise the SVR24 rate and may lessen the severity of RBV-induced anemia.
With regard to safety, treatment by Peg-IFN alfa-2a plus RBV for 16 weeks showed low rates of serious AE and treatment withdrawal in weight-based and flat-dose RBV arms. Except for the tendency of clinically significant anemia at treatment weeks 6–16 in weight-based RBV arm, the constitutional symptoms and the other laboratory abnormalities of interest were comparable between the two arms. However, the proportions of severe anemia (Hb < 8.5 g/dL) which warranted temporary RBV discontinuation were low (6.9% and 6.1%) in weight-based and flat-dose RBV arms, respectively, implying that by careful monitoring the on-treatment hemoglobin levels and titrating the RBV dosages, most patients receiving weight-based or flat-dose RBV may safely complete treatment.
Our study had several limitations. First, our patients were East Asians and the results should be validated in patients of different ancestry. Second, with the introduction of sofosbuvir-base therapies which confers excellent treatment responses, Peg-IFN plus RBV therapy may not be listed in the first-line therapy in Western countries. Despite the potentially higher on-treatment AE rates by Peg-IFN plus RBV therapy, our study also showed that HCV-2 rapid responders may also achieve high SVR rates by 16 weeks of therapy. The use of our strategies may provide a practical guide of IFN-eligible HCV-2 patients in resource-limited countries for sofosbuvir-based therapy28.
In conclusion, Peg-IFN alfa-2a plus weight-based or flat-dose RBV for 16 weeks provides comparable SVR rates for treatment-naïve HCV-2 patients with RVR. However, males should receive Peg-IFN alfa-2a plus weight-based RBV to provide a high SVR rate.
Materials and Methods
Patients
Treatment-naïve Taiwanese HCV-2 patients who were old than ≥18 years who had serum alanine aminotransferase (ALT) level ≥upper limit of normal (ULN) were consecutively enrolled between 2007 and 2013 in the Tailored Regimens of Peginterferon alfa-2a and Ribavirin for Genotype 2 Chronic Hepatitis C Patients (TARGET-2) trial. Chronic HCV infection was defined as documentation of anti-HCV antibody (Abbott HCV EIA 3.0, Abbott Laboratories, Abbott Park, Illinois, USA) and HCV RNA (Cobas TaqMan HCV Test v2.0, Roche Diagnostics GmbH, Mannheim, Germany, limit of detection: 15 IU/mL) for ≥6 months. The HCV genotyping was tested by reverse hybridization assay (Versant HCV Genotype 2.0 assay, Siemens Healthcare Diagnostics, Illinois, USA)29.
The exclusion criteria of the study were as follows: hemoglobin levels <13 g/dL for men or <12 g/dL for women, neutrophil count <1.5 × 109 cells/L, platelet count < 90 × 109 cells/L, hepatitis B virus (HBV) or human immunodeficiency virus (HIV) co-infection, HCV infection other than genotype 2, alcohol consumption >20 g/day, serum albumin level <35 g/L, serum bilirubin level ≥1.5 times ULN, serum AST or ALT level ≥10 times ULN, serum creatinine level ≥1.5 times ULN, Child-Puge grade B or C cirrhosis, history of autoimmune liver diseases or neoplastic diseases, concurrent immunosuppressive therapy, pregnancy, poorly controlled systemic illness or unwilling to receive birth control during the study period.
The study was approved by Taiwan Joint Institutional Review Board. All study procedures were conducted in accordance with the principles of Declaration of Helsinki and the International Conference on Harmonization for Good Clinical Practice. Patients who were willing to join the study provided written informed consent before enrollment.
Study Design
This was a multicenter randomized controlled trial. All patients who were eligible to participate in this trial received induction therapy of Peg-IFN alfa-2a 180 μg/week (Pegasys, Hoffman-LaRoche, Basel, Switzerland) plus weight-based RBV 1,000 or 1,200 mg/day (Copegus, Hoffman-LaRoche, Basel, Switzerland; cut-off body weight: 75 kg) for 6 weeks. The viral responses at week 4 of treatment were evaluated for all patients. At week 6 of treatment, patients who achieved rapid virologic response (RVR), defined as undetectable serum HCV RNA at week 4 of treatment, were randomly assigned as 1:1 ratio to receive Peg-IFN alfa-2a 180 μg/week plus weight-based (1,000 or 1,200 mg/day) or flat-dose (800 mg/day) RBV for additional 10 weeks (Fig. 2). Randomization code was computer-generated in blocks of 4 and secured by an independent assistant. In addition, all patients were centrally allocated to the assigned treatment.
Baseline demographic data, hemoglobin level, neutrophil count and platelet count, serum albumin, serum bilirubin, serum AST, serum ALT, serum creatinine, anti-HCV, HBsAg, anti-HIV, HCV RNA, HCV genotype and IL-28B rs8099917 genotypes (ABI TaqMan allelic discrimination kit and ABI7900HT Sequence Detection System, Applied Biosystems, Life Technologies Corporation, Grand Island, New York, USA) were evaluated. The hepatic fibrosis was staged by APRI30. Low baseline viral load was defined as a level of <800,000 IU/mL, whereas high baseline viral load was defined as a level of ≥800,000 IU/mL11. IL-28B rs8099917 TT genotype was defined as favorable genotype and GT/GG genotype was defined as unfavorable genotype, respectively31,32,33. An APRI score of >1.50 and >2.00 denoted significant hepatic fibrosis (≥F2 by Metavir score) and cirrhosis (F4 by Metavir score), respectively34.
Efficacy
All patients received treatment for 16 weeks and the off-therapy follow-up for 24 weeks. Serum HCV RNA levels were assessed at weeks 4 and 16 of treatment and at week 24 after the cessation of therapy. The ETVR and the SVR24 were defined as previously described11. The ETVR was assessed for all patients who early discontinued treatment at the treatment discontinuation.
The primary endpoint was SVR24, defined as undetectable serum HCV RNA 24 weeks after the cessation of therapy. Patients with viral breakthrough at the end-of-treatment were considered failure to achieve SVR24, regardless of the end of follow-up HCV RNA data. Patients who lacked the end of follow-up data to assess SVR24 or who relapsed after the cessation of treatment were also considered failure to achieve SVR24. Sensitivity analyses were done for the primary endpoint.
Safety
During the study period, the safety profiles were reported by a prespecified checklist to assess the severity and the causality of the AEs. The grades of all AEs were assessed by the Common Terminology Criteria for Adverse Events (CTCAE), version 3.0. If the patients had serious AEs, missed he allocated treatment for >4 consecutive weeks, or subjectively stopped treatment, they were considered withdrawn from the study.
Based on the severity of the constitutional AEs, the dosage of Peg-IFN alfa-2a and RBV was reduced in a stepwise fashion of 45 μg/week and 200 mg/day as tolerated. With regard to hematological toxicity, Peg-IFN alfa-2a was reduced from 180 μg/week to 90 μg/week if the neutrophil count was <0.75 × 109 cells/L or the platelet count was <50 × 109 cells/L and Peg-IFN alfa-2a was stopped if the neutrophil count was <0.50 × 109 cells/L or the platelet count was <25 × 109 cells/L. RBV was reduced in a stepwise fashion of 200 mg/day if the hemoglobin level was <10 g/dL and RBV was stopped if the hemoglobin level was <8.5 g/dL. The erythropoiesis-stimulating agent (ESA) was not permitted during the treatment. Blood transfusion was allowed if the patients developed serious hematological AEs. Peg-IFN or RBV was allowed to be reinitiated or increased in dosage as tolerated if the constitutional or laboratory AEs improved following treatment cessation or dosage reduction.
Statistical Analyses
Analysis of the data was performed by Statistical Program for Social Sciences (SPSS 17.0; SPSS Inc., Chicago, Illinois, USA). Based on the assumption that the SVR24 rate was 86% for patients assigned to receive Peg-IFN plus flat-dose RBV, we estimated that 488 patients would provide 90% power to detect an absolute increase of 8% or more in SVR24 for patients assigned to receive Peg-IFN plus weight-based RBV (2-sided α = 0.05)12,18. Values were expressed as mean (standard deviation, SD) or percentage when appropriate.
The on-treatment and off-therapy viral response rates between weight-based and flat-dose RBV arms were compared by RD. The P values for RD were assessed by the Wald asymptotic test. The subgroup analyses for the factors of interest to predict SVR24, including baseline viral load, HCV subgenotype, IL-28B rs8099917 genotype, age, sex, body weight, APRI score, RBV dosage and 80/80/80 rule were compared by RD35. The interactions between the prespecified factors and the treatment arms were evaluated by the stratified Mantel-Haenszel test. The dosage of RBV associated with SVR was compared by chi-square with Fisher’s exact test. All statistical tests were two-tailed and the results were considered to be statistically significant when a P value was <0.05.
Additional Information
How to cite this article: Liu, C.-H. et al. Peginterferon alfa-2a plus Weight-Based or Flat-Dose Ribavirin for Treatment-Naïve Hepatitis C Virus Genotype 2 Rapid Responders: A Randomized Trial. Sci. Rep. 5, 15255; doi: 10.1038/srep15255 (2015).
References
Rosen, H. R. Clinical practice. Chronic hepatitis C infection. N. Engl. J. Med. 364, 2429–2438 (2011).
Yu, M. L. & Chuang, W. L. Treatment of chronic hepatitis C in Asia: when East meets West. J. Gastroenterol. Hepatol. 24, 336–345 (2009).
Sievert, W. et al. A systematic review of hepatitis C virus epidemiology in Asia, Australia and Egypt. Liver. Int. 31, (Suppl 2), 61–80 (2011).
Liu, C. H. & Kao, J. H. Nanomedicines in the treatment of hepatitis C virus infection in Asian patients: optimizing use of peginterferon alfa. Int. J. Nanomedicine. 9, 2051–2067 (2014).
Manns, M. P. et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet. 358, 958–965 (2001).
Fried, M. W. et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N. Engl. J. Med. 347, 975–982 (2002).
Hadziyannis, S. J. et al. Peginterferon-alpha2a and ribavirin combination therapy in chronic hepatitis C: a randomized study of treatment duration and ribavirin dose. Ann. Intern. Med. 140, 346–355 (2004).
McHutchison, J. G. et al. Peginterferon alfa-2b or alfa-2a with ribavirin for treatment of hepatitis C infection. N. Engl. J. Med. 361, 580–593 (2009).
Mangia, A. et al. Individualized treatment duration for hepatitis C genotype 1 patients: a randomized controlled trial. Hepatology. 47, 43–50 (2008).
Yu, M. L. et al. Rapid virological response and treatment duration for chronic hepatitis C genotype 1 patients: a randomized trial. Hepatology. 47, 1884–1893 (2008).
Liu, C. H. et al. Pegylated interferon-alpha-2a plus ribavirin for treatment-naive Asian patients with hepatitis C virus genotype 1 infection: a multicenter, randomized controlled trial. Clin. Infect. Dis. 47, 1260–1269 (2008).
Yu, M. L. et al. A randomised study of peginterferon and ribavirin for 16 versus 24 weeks in patients with genotype 2 chronic hepatitis C. Gut. 56, 553–559 (2007).
Jacobson, I. M. et al. Sofosbuvir for hepatitis C genotype 2 or 3 in patients without treatment options. N. Engl. J. Med. 368, 1867–1877 (2013).
Lawitz, E. et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N. Engl. J. Med. 368, 1878–1887 (2013).
Zeuzem, S. et al. Sofosbuvir and ribavirin in HCV genotypes 2 and 3. N. Engl. J. Med. 370, 1993–2001 (2014).
Sulkowski, M. S. et al. Daclatasvir plus sofosbuvir for previously treated or untreated chronic HCV infection. N. Engl. J. Med. 370, 211–221 (2014).
European Association for Study of Liver. EASL Clinical Practice Guidelines: management of hepatitis C virus infection. J. Hepatol. 60, 392–420 (2014).
Di Martino, V. et al. Response-guided peg-interferon plus ribavirin treatment duration in chronic hepatitis C: meta-analyses of randomized, controlled trials and implications for the future. Hepatology. 54, 789–800 (2011).
Chou, R. et al. Comparative effectiveness of antiviral treatment for hepatitis C virus infection in adults: a systematic review. Ann. Intern. Med. 158, 114–123 (2013).
Mangia, A. et al. An IL28B polymorphism determines treatment response of hepatitis C virus genotype 2 or 3 patients who do not achieve a rapid virologic response. Gastroenterology. 139, 821–827, 827.e1 (2010).
Sarrazin, C. et al. Importance of IL28B gene polymorphisms in hepatitis C virus genotype 2 and 3 infected patients. J. Hepatol. 54, 415–421 (2011).
Yu, M. L. et al. Role of interleukin-28B polymorphisms in the treatment of hepatitis C virus genotype 2 infection in Asian patients. Hepatology. 53, 7–13 (2011).
Mangia, A. et al. Peginterferon alfa-2b and ribavirin for 12 vs. 24 weeks in HCV genotype 2 or 3. N. Engl. J. Med. 352, 2609–2617 (2005).
Shiffman, M. L. et al. Peginterferon alfa-2a and ribavirin for 16 or 24 weeks in HCV genotype 2 or 3. N. Engl. J. Med. 357, 124–134 (2007).
Shiffman, M. L. et al. Extended treatment with pegylated interferon alfa/ribavirin in patients with genotype 2/3 chronic hepatitis C who do not achieve a rapid virological response: final analysis of the randomised N-CORE trial. Hepatol. Int. 8, 517–526 (2014).
Liu, C. H. et al. Peginterferon plus weight-based ribavirin for treatment-naïve hepatitis C virus genotype 2 patients not achieving rapid virologic response: a randomized trial. Sci. Rep. 5, 11710 (2015).
Heidrich, B. et al. Treatment Extension of Pegylated Interferon Alpha and Ribavirin Does Not Improve SVR in Patients with Genotypes 2/3 without Rapid Virological Response (OPTEX Trial): A Prospective, Randomized, Two-Arm, Multicentre Phase IV Clinical Trial. PLoS. One. 10, e0128069 (2015).
Mangia, A. & Andriulli, A. Tailoring the length of antiviral treatment for hepatitis C. Gut. 59, 1–5 (2010).
Liu, C. H. et al. Comparison of Abbott RealTime HCV Genotype II with Versant line probe assay 2.0 for hepatitis C virus genotyping. J. Clin. Microbiol. 53, 1754–1757 (2015).
Liu, C. H. et al. Noninvasive tests for the prediction of significant hepatic fibrosis in hepatitis C virus carriers with persistently normal alanine aminotransferases. Liver. Int. 26, 1087–1094 (2006).
Huang, C. F. et al. Interleukin-28B genetic variants in identification of hepatitis C virus genotype 1 patients responding to 24 weeks peginterferon/ribavirin. J. Hepatol. 56, 34–40 (2012).
Liu, C. H. et al. Interleukin 28B genetic polymorphisms and viral factors help identify HCV genotype-1 patients who benefit from 24-week pegylated interferon plus ribavirin therapy. Antivir. Ther. 17, 477–484 (2012).
Liu, C. H. et al. Interleukin 28B genetic polymorphisms play a minor role in identifying optimal treatment duration in HCV genotype 1 slow responders to pegylated interferon plus ribavirin. Antivir. Ther. 17, 1059–1067 (2012).
Wai, C. T. et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 38, 518–526 (2003).
McHutchison, J. G. et al. Adherence to combination therapy enhances sustained response in genotype-1-infected patients with chronic hepatitis C. Gastroenterology. 123, 1061–1069 (2002).
Acknowledgements
The authors thank the nurses and the patients involved in the study; Ching-Chuan Chen for central block randomization management; Hui-Ju Lin, Yu-Lin Tan, Po-Chung Liu for clinical data management; Wan-Ting Yang for host genetic analyses; Yu-Sheng Chiu, PhD for virology analyses; the 4th Core Lab of National Taiwan University Hospital and the 1st Common Laboratory of National Taiwan University Hospital, Yun-Lin Branch for instrumental and technical support. The authors thank all the TARGET-2 investigators to participate the study. Grant Support: Ministry of Science and Technology, Taiwan (NSC 100-2314-B-002-137-MY2). Trial registration number: ClinicalTrial.gov number, NCT00532701.
Author information
Authors and Affiliations
Contributions
C.H.L., C.F.H., W.L.C., J.H.K. and M.L.Y. designed the study; C.H.L., C.F.H., W.L.C., J.H.K. and M.L.Y. analyzed and interpreted data; C.H.L., C.F.H., C.J.L., W.L.C., J.H.K. and M.L.Y. drafted the article; C.H.L., C.F.H., C.J.L., C.Y.D., J.F.H., J.W.L., CC.L., S.S.Y., C.L.L., T.H.S., H.C.Y., P.J.C., D.S.C., W.L.C., J.H.K. and M.L.Y. revised and approved the article for important intellectual content; C.H.L., C.F.H., C.J.L., C.Y.D., J.F.H., J.W.L., C.C.L., S.S.Y., C.L.L., T.H.S., H.C.Y., P.J.C., D.S.C., W.L.C., J.H.K. and M.L.Y. provided the study materials or patients; C.H.L., C.F.H., J.W.L., J.H.K. and M.L.Y. performed statistics; C.H.L., C.F.H., J.H.K. and M.L.Y. obtained funding; J.H.K. and M.L.Y. provided administrative, technical or logistic support; C.H.L., C.F.H., J.W.L., J.H.K. and M.L.Y. collected and assembled data.
Ethics declarations
Competing interests
Chen-Hua Liu: consultant for Abbott, Abbvie, Bristol-Myers Squibb, Roche, Johnson & Johnson and Gilead Sciences; grant support from Abbvie; on speaker’s bureau for Abbott, Roche, Bristol-Myer Squibb, GlaxoSmithKline, Novartis and Gilead Sciences. Jia-Horng Kao: consultant for Abbott, Abbvie, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Merck Sharp & Dohme, Novartis, Roche, Johnson & Johnson and Gilead Sciences; on speaker’s bureau for Abbott, Abbvie, Roche, Bayer, Bristol-Myers Squibb, GlaxoSmithKline and Novartis; Ding-Shinn Chen: consultant for Novartis and GlaxoSmithKline; Pei-Jer Chen: consultant for Novartis and Roche; Ming-Lung Yu and Wan-Long Chuang: consultants for Merck Sharp & Dohme Abbott, Abbvie, Johnson & Johnson and Gilead; grants support from Abbvie, Abbott and Roche; on speaker’s bureau from Bristol-Myers Squibb, Roche, Merck Sharp & Dohme, GlaxoSmithKline, Novartis and Gilead Sciences.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Liu, CH., Huang, CF., Liu, CJ. et al. Peginterferon alfa-2a plus Weight-Based or Flat-Dose Ribavirin for Treatment-Naïve Hepatitis C Virus Genotype 2 Rapid Responders: A Randomized Trial. Sci Rep 5, 15255 (2015). https://doi.org/10.1038/srep15255
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep15255
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.