Abstract
Worldwide, prostate cancer (PCa) is the second most common malignancy in males. We undertook a meta-analysis to compare the efficacy and safety of conventional laparoscopic radical prostatectomy with a transperitoneal (TLRP) approach, versus that of an extraperitoneal (ELRP) approach, for treatment of localized PCa. A comprehensive literature search retrieved 14 publications, with a total of 1715 patients. Meta-analysis of these studies showed that an ELRP approach was associated with a significantly shorter postoperative catheterization time (MD: 1.99; 95% CI: 0.52 to 3.54; P = 0.008), less blood transfusion rate (OR: 2.05; 95% CI: 1.03 to 4.06; P = 0.04), shorter intestinal function recovery time (MD: 0.08; 95% CI: 0.52 to 1.09; P < 0.0001) and shorter hospitalization days (MD: 2.71; 95% CI: 1.03 to 4.39; P = 0.002). In addition, our results showed no statistically significant differences between the two groups in operation time (MD: 19.39; 95% CI: −6.67 to 45.44; P = 0.014), intraoperative blood loss (MD: 4.89; 95% CI: −105.00 to 114.79; P = 0.93) and total complication rate (RR: 1.22; 95% CI: 0.86 to 1.74; P = 0.27). In summary, our meta-analysis showed that ELRP is likely to be a safe and feasible alternative for localized PCa patients compared with TLRP.
Similar content being viewed by others
Introduction
Prostate cancer (PCa) is the second most common malignancy in males worldwide and has increased in incidence in recent years1. In 2014, PCa incidence rates in the United States reached approximately 27% of all new cancer cases2. Radical prostatectomy is one of the methods in treating localized PCa3. A minimally invasive technique, conventional laparoscopic radical prostatectomy (LRP) was first introduction in 1992 by Schuessler et al.4; LRP has since become a common treatment approach for the management of patients with localized PCa5.
However, both approaches to conventional LRP are routinely used in urological practice: the transperitoneal LRP (TLRP) and the extraperitoneal LRP (ELRP). Both approaches have been touted as efficacious and safe techniques by which to perform LRP6,7,8,9,10,11; however, whether TLRP is superior to ELRP in terms of efficacy and safety has become a subject of controversy in recent years. We performed a meta-analysis to assess the safety and efficacy of TLRP and ELRP.
Results
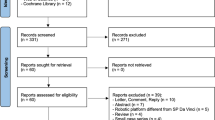
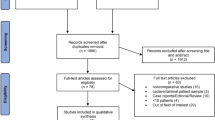
We formulated a comprehensive search strategy to identify all relevant studies, regardless of the language or publication status. Through literature selection, 14 studies were identified from the literature search. The literature screening process is summarized in Fig. 1.
A total of 1715 patients were included in the 14 studies7,8,9,10,11,12,13,14,15,16,17,18,19,20; of these, 939 underwent TLRP and 776 underwent ELRP. All included studies reported on the number of patients. Two studies failed to report mean PSA levels12,14. Seven studies reported on the mean Gleason scores7,9,10,11,16,18,19. The basic characteristics and quality assessments of the included studies were summarized in Table 1.
Study results and meta-analysis
Operation time (minutes)
Operation time was reported in eleven studies9,10,11,13,14,15,16,17,18,19,20 (1159 patients): 617 receiving TLRP and 542 receiving ELRP. Heterogeneity was observed in the pooled analysis (P < 0.0001; I2 = 95%). In this present meta-analysis of the eleven studies using the random-effect model, the pooled estimates showed no statistically significant difference between the two groups (mean difference [MD]: 19.39; 95% confidence interval [95% CI]: −6.67–45.44; P = 0.014) (Fig. 2). However, after excluding the results from Siqueira et al.17, sensitivity analysis showed that there was a statistically significant difference between the TLRP and ELRP groups (MD: 30.75; 95% CI: 9.66–51.84; P = 0.004).
Intraoperative blood loss (mL)
Mean blood loss during LRP surgery was reported in ten studies9,11,13,14,15,16,17,18,19,20 (1053 participants). Heterogeneity was detected in the pooled analysis (P < 0.0001; I2 = 96%). Data from the ten studies were merged for meta-analysis using a random-effects model. The result revealed no statistically significant difference between the two groups (MD: 4.89; 95% CI: −105.00–114.79; P = 0.93) (Fig. 3). This finding indicates that there was a similar rate of intraoperative bleeding in the TLRP group, compared to the ELRP group.
Blood transfusion rate
Blood transfusion rate was measured in eight studies7,8,12,13,14,15,16,19 including 875 patients; our meta-analysis indicated that ELRP group had lower blood transfusion rate than TLRP groups (odd ratio [OR]: 2.05; 95% CI: 1.03 – 4.06; P = 0.04) without statistical heterogeneity (P = 0.98; I2 = 0%) (Fig. 4).
Postoperative catheterization time (days)
We extracted the data of postoperative catheterization time from the six studies13,15,16,18,19,20. The pooled data indicated that the heterogeneity was exist (P < 0.0001, I2 = 83%). There was statistically significant in shorter postoperative catheterization time in the ELRP group compared with the TLRP group (MD: 1.99; 95% CI: 0.52–3.54; P = 0.008; Fig. 5).
Postoperative intestinal function recovery time (days)
Data on postoperative intestinal function time were extracted for meta-analysis from five studies13,15,16,18,19. Heterogeneity was revealed in the pooled analysis (P = 0.07; I2 = 54%); the result from the combined studies using a random-effect model showed that ELRP group was associated with a shorter intestinal function recovery time than TLRP group (MD: 0.80; 95% CI: 0.52–1.09; P < 0.0001) (Fig. 6).
Hospitalization days
Eight studies9,11,13,15,16,18,19,20 including 938 patients compared the hospital time between the TLRP group and ELRP group. High heterogeneity was observed in the pooled analysis (P < 0.0001; I2 = 93%). In the random-effect model meta-analysis of the eight studies, the pooled estimates had statistically significantly different between the 2 groups (MD: 2.71; 95% CI: 1.03–4.39; P = 0.002) (Fig. 7). This pooled analysis indicated that ELRP group was associated with a markedly shorter hospital time than TLRP group.
Total complication rate
Postoperative total complication rate of the eight studies7,8,9,12,13,17,19,20 was revealed an 11.4% (86/753) incidence in TLRP group and a 9.8% (61/623) incidence in ELRP group. No heterogeneity was exist in the pooled analysis (P = 0.81; I2 = 0%), a fixed-effect model was used for statistical analysis. ELRP group was associated with a lower total complication rate than TLRP group, but the meta-analysis demonstrated that no statistically significant difference was exist (RR: 1.22; 95% CI: 0.86 to 1.74; P = 0.27) (Fig. 8).
Discussion
Radical prostatectomy is one of the ways for treat patients with localized PCa3. The advantages of LRP over open radical prostatectomy include a reduced intraoperative blood loss, a lower blood transfusion rate, shorter hospitalization days, a shorter time to resumption of routine activity and improved scar heals well21,22. However, robot-assisted radical prostatectomy has higher costs than conventional LRP technology23. In current practice, conventional LRP approach for localized PCa patients is available14,15,16,17,18,19,20,21. In addition, either a transperitoneal or an extraperitoneal approach has been demonstrated to be both safe and effective. Although there is a meta-analysis reporting on the safety and efficacy between TLRP and ELRP that was published in Chinese24, this is necessary to update this meta-analysis for provided update evidence regarding their benefits for patients with localized PCa. Therefore, we conduct the systematic review and meta-analysis to compare the safety and efficacy of TLRP with ELRP for the treatment of localized PCa.
The results of the present meta-analysis demonstrated a similar operation time with TLRP, relative to ELRP. Studies conducted by Erdogru et al.10 and Wang et al.16 reported that TLRP was associated with a shorter operation time, compared with ELRP. Conversely, other research showed ELRP had a shorter operation time, compared with TLRP9,13,14,15. To our surprise, after excluding study data from Siqueira et al.17 from our meta-analysis, a statistically significant difference was found between the TLRP and ELRP groups. Furthermore, our finding from the pooled analysis revealed that operating times were 30.75 minutes shorter in the ELRP group, compared with the TLRP group; and this difference was statistically significant. The findings from the pooled analysis were consistent with those of 2 studies that were not included in our meta-analysis21,22. It is plausible that the shorter operative time might result from the direct access to the retropubic space and avoidance of bowel handling in ELRP. We supposed that it is possible that this result was influenced by the small sample sizes or a lack of surgical experience in the ELRP procedure in the study. Therefore, it is necessary to evaluate the operation time of TLRP versus ELRP in further, high quality, randomized controlled trials with larger sample sizes.
Our findings reveal that the average blood loss during TLRP group was similar to that associated with ELRP group and the observed difference did not achieve statistical significance. Therefore, ELRP had no advantages, in terms of reduced blood loss, compared with TLRP. However, our results regarding blood transfusion rate clearly indicated that the TLRP group had a rate 2.05 times higher than the ELRP group. This present findings also agree with the results of previous controlled clinical trial15,16.
The present results indicate a significantly faster intestinal function recovery time following ELRP, compared with TLRP. From Fig. 4, it is clear that the mean intestinal function recovery time in the ELRP group was 0.8 times faster than seen in TLRP group. Porpiglia et al. reviewed 160 patients who underwent radical prostatectomy, either TLRP or ELRP; they also reported a faster intestinal function recovery time in the ELRP group13. Our findings are also consistent with the findings of a previous study by Liu et al.24.
Additionally, the present meta-analysis demonstrated that ELRP was superior to TLRP with regard to postoperative catheterization time and hospitalization days. However, there was no statistically significant difference in terms of overall complication rate. As described previously23,24, our results are in agreement with those of researchers, suggesting a shorter catheterization time and hospitalization days in the ELRP group. There was a similar overall rate of complications in the 2 groups11,12,13,14,15,16,17,18,19,20. Total complication rates generally include bleeding, intra-abdominal organ and vessel injuries, urinary leakage, ileus, anastomotic leakage, pulmonitis, lymphocele formation and stricture at vesicourethral anastomosis. Certainly, we also thought that the rate of complications may be associated with surgical experience and skill. Complication rates were reported by research centers and revealed a mean complication rate of approximately 10% for the each approach25,26. Results of the current study showed a total complication rate of 11.4% (86/753) in the TLRP group and 9.8% (61/623) in the ELRP group; the difference was not statistically significant, consistent with the findings of the above wor25,26.
Overall, it is generally considered that the main advantages of the TLRP procedure are; (1) the faster placement of trocars; and (2) the larger cavity, which allows placement of the specimen bag out of the operative field, improving vision and facilitating the vesicourethral anastomosis. However, TLRP also has many disadvantages, including the requirement of a much steeper Trendelenburg position to move the bowel out of the pelvic cavity. This position might cause upper airway and facial swelling, which may postpone extubation, lengthen the recovery time and increase the risk of brachial plexus injury27. The bowels may adhere in the retropubic space of Retzius after the operation and radiation therapy can lead to radiation enteritis. Such factors might explain the longer catheterization time and longer duration of hospitalization days associated with TLRP.
The ELRP approach has several advantages; the procedure can be finished extraperitoneally and the Trendelenburg required is less steep, compared with the transperitoneal route. The incidence rate of bowel lesions, ileus and peritonitis is therefore lower and the procedure prevents herniation from the trocar ports. The peritoneum can isolate the operative field from the abdominal cavity, bleeding does not contact the bowel and reflex ileus is avoided; even a poor anastomosis could not result in urinary ascites with its associated complications8,9. In addition, a self-made gasbag is inserted sufflating gas to build a pneumopreperitoneum. This keeps pressure on the peripheral tissues and inhibits serious bleeding. However, there is also a greater risk of rectal injury with the initial dissection of the seminal vesicles, especially in obese patients. Therefore, from the above-mentioned technical considerations, ELRP might have lower blood transfusion rate and shorter intestinal function recovery time, but a similar total complication rate.
Our meta-analysis detected heterogeneity in the operation time, intraoperative blood loss, postoperative catheterization time, postoperative intestinal function recovery time and hospitalization days. We maintain that these heterogeneities might have resulted from differences in the skill of the surgeon. Additionally, the small sample sizes and difference between patients, which included different clinical stages and prostate volume, could have potentially increased the degree of heterogeneity. Additional factors that have been predicted to potentially amplify heterogeneity between studies include differences in country, follow-up periods and a lack of uniformity in surgical procedure measurement standards.
Our systematic review and meta-analysis has several limitations. The study quality estimation was influenced by the non-randomized studies and there was inadequate information provided in terms of methodological differences among the included studies. Some studies did not adequately report the outcomes measures. In addition, we could not obtain some relevant data, which may have introduced bias. Nonetheless, with the exception of operation time, the all conclusions were stable and were not impacted by the sensitivity analysis, in which each study was sequentially excluded from the pooled analysis.
In summary, both ELRP and TLRP have advantages and disadvantages; the efficacy and safety of LRP related to standardization of the procedure and the personal experience of the surgeon. However, this present meta-analysis has demonstrated that ELRP is associated with a lower blood transfusion rate, shorter catheterization time, faster intestinal function recovery time and shorter hospitalization days, compared with TLRP. In addition, the approaches are similar in terms of operation time, intraoperative blood loss and total complication rate. Therefore, the present meta-analysis showed that ELRP is likely to be a safe and feasible alternative for patients with localized PCa.
Methods
Search strategy
We performed a systematic literature search up to May 1, 2014 using Medline, Embase, the Cochrane library and Google Scholar databases. We did not restrict our search to articles published in English. The following search terms were used: transperitoneal; extraperitoneal; LRP; PCa; or prostatic neoplasms. We also searched the relevant references of all included studies and manually searched urology, andrology and oncology diseases journals for further relevant articles. The search strategy was independently performed by 2 reviewers.
Study selection
All randomized or non-randomized controlled trials that compared TLRP with ELRP and included data on at least 1 of the pre-defined outcome measures were eligible for inclusion. Studies were excluded if they met any of the following criteria; (1) not comparative studies for TLRP versus ELRP; (2) robot-assisted radical prostatectomy; (3) study sample did not comprise PCa patients. When multiple publications from the same study or institution were available, we used the publication with the largest number of cases. Review of all titles and abstracts of the included studies was independently performed by 2 authors and full texts were screened when necessary. Any disagreements were resolved in consultation with Wei Q. All of the authors have reached a consensus with respect to included/excluded studies.
Data extraction
The following information was recorded independently by 2 reviewers, using data extraction forms: the first author’s name, year of publication, origin country, total number of patients, average age, prostatic specific antigen level, Gleason score and the type of research design. All extracted data was cross-checked and discrepancies in the data were resolved after discussions among all authors. The following outcome measures were recorded from the included studies: (1) operation time; (2) intraoperative blood loss; (3) blood transfusion rate; (4) postoperative catheterization time; (5) intestinal function recovery time; (6) hospitalization days; (7) total complication rate. All of the authors have reached a consensus with respect to the extracted data.
Quality assessment
The quality of the included studies was measured independently by two reviewers using a modification of the Newcastle–Ottawa Scale28. Review scores ranged from 0 to 9 points for each trial. Scores ranging from 0 to 4 were defined as low-quality while those ranging from 5 to 9 were defined as high-quality. Any disagreements were resolved after discussion between the two reviewers. All of the authors have reached a consensus with respect to the quality of the included studies.
Statistical analysis
All statistical analyses were conducted using Review Manager, version 5.1.0 (Cochrane Collaboration, Oxford, UK). Statistical analysis of dichotomous variables (blood transfusion rate and total complication rate) was performed using the OR as the summary analysis, while continuous variables (operation time, intraoperative blood loss, postoperative catheterization time, intestinal function recovery time and hospitalization days) were analyzed using the MD; accompanying 95% CI and P-value were reported. For all statistical results, P < 0.05 was considered statistically significant. The Mantel-Haenszel chi-squared test for heterogeneity was conducted. Heterogeneity was assessed using the I2 statistic. I2 values of < 50% were defined as acceptable; a fixed-effects models was used, otherwise random-effects model was applied for the meta-analysis.
Additional Information
How to cite this article: De Hong, C. et al. Comparison of efficacy and safety of conventional laparoscopic radical prostatectomy by the transperitoneal versus extraperitoneal procedure. Sci. Rep. 5, 14442; doi: 10.1038/srep14442 (2015).
References
Plata, B. A. & Concepcion, M. T. Prostate cancer epidemiology. Arch Esp Urol 67, 373–382 (2014).
Siegel, R., Ma, J., Zou, Z. & Jemal, A. Cancer Statistics, 2014. CA Cancer J Clin 64, 9–29 (2014).
Menon, M. et al. Laparoscopic radical prostatectomy: conventional and robotic. Urology 66, 101–104 (2005).
Schuessler, W. W., Kavoussi, L. R., Clayman, R. V. & Vancaille, T. H. Laparoscopic radical prostatectomy: initial case report. J Urol 147, 246 (1992).
Stolzenburg, J. U. et al. Endoscopic extraperitoneal radical prostatectomy: evolution of the technique and experience with 2400 cases. J Endourol 23, 1467–1472 (2009).
Liatsikos, E. et al. Comments on the extraperitoneal approach for standard laparoscopic radical prostatectomy: what is gained and what is lost. Prostate Cancer 2011, 150978 (2011).
Eden, C. G. et al. Transperitoneal or extraperitoneal laparoscopic radical prostatectomy: does the approach matter? J Urol 172, 2218–2223 (2004).
Cathelineau, X. et al. Transperitoneal or extraperitoneal approach for laparoscopic radical prostatectomy: a false debate over a real challenge. J Urol 171, 714–716 (2004).
Ruiz, L. et al. Comparison of early oncologic results of laparoscopic radical prostatectomy by extraperitoneal versus transperitoneal approach. Eur Urol 46, 50–56 (2004).
Erdogru, T. et al. Comparison of transperitoneal and extraperitoneal laparoscopic radical prostatectomy using match-pair analysis. Eur Urol 46, 312–319 (2004).
Remzi, M. et al. Morbidity of laparoscopic extraperitoneal versus transperitoneal radical prostatectomy verus open retropubic radical prostatectomy. Eur Urol 48, 83–89 (2005).
Brown, J. A., Rodin, D., Lee, B. & Dahl, D. M. Transperitoneal versus extraperitoneal approach to laparoscopic radical prostatectomy: an assessment of 156 cases. Urology 65, 320–324 (2005).
Porpiglia, F. et al. Transperitoneal versus extraperitoneal laparoscopic radical prostatectomy: experience of a single center. Urology 68, 376–380 (2006).
Katz, P. et al. Laparoscopic radical prostatectomy in patients following transurethral resection of the prostate. Urol Int 77, 216–221 (2006).
Gao, Z. L. et al. Comparison of the extraperitoneal and transperitoneal laparoscopic radical prostatectomy. Chin Med J 119, 2125–2128 (2006).
Wang, S. et al. Comparison of transperitoneal and extraperitoneal laparoscopic radical prostatectomy. Chin J Urol 29, 329–331 (2008).
Siqueira, T. M. Jr. et al. Transperitoneal versus extraperitoneal laparoscopic radical prostatectomy during the learning curve: does the surgical approach affect the complication rate? Int Braz J Urol 36, 450–457 (2010).
Wang, Z. R. et al. Laparoscopic radical prostatectomy: transpetitoneal approach versus extrapetitoneal approach. J Practical Oncology 24, 533–549 (2010).
San, Q., Chen, X. J. & Sun, L. N. Effect observation of extraperitoneal laparoscopic radical prostatectomy. YiYao QianYan 2, 227–228 (2012).
Zhao, Z. et al. Comparation of the transperitoneal and extraperitoneal laparoscopic radical prostatectomy. Chin J Surg 52, 135–138 (2014).
Phinthusophon, K., Nualyong, C., Srinualnad, S., Taweemonkongsap, T. & Amornvesukij, T. Laparoscopic radical prostatectomy: transperitoneal laparoscopic radical prostatectomy versus extraperitoneal endoscopic radical prostatectomy. J Med Assoc Thai 90, 2644–2650 (2007).
Stolzenburg, J. U. et al. Endoscopic extraperitoneal radical prostatectomy: oncological and functional results after 700 procedures. J Urol 174, 1271–1275 (2005).
Ia Chapelle, C. F., Jansen, F. W., Pelger, R. C. & Mol, B. W. Robotic surgery in the Netherlands: lack of high-quality proof of efficacy. Ned Tijdschr Geneeskd 157, 5154 (2013).
Liu, L. H. et al. Transperitoneal versus extraperitoneal laparoscopic radical prostatectomy for localized prostate cancer: a meta analysis. National J of Andrology 19, 1020–1026 (2013).
Coelho, R. F., et al. Retropubic, laparoscopic and robot-assisted radical prostatectomy: a critical review of outcomes reported by high-volume centers. J Endourol 24, 2003–2015 (2010).
Ficarra, V. et al. Retropubic, laparoscopic and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur Urol 55, 1037–1063 (2009).
Rozet, F., Harmon, J., Cathelineau, X., Barret, E. & Vallancien, G. Robot-assisted versus pure laparoscopic radical prostatectomy. World J Urol 24, 171–179 (2006).
Wells, G. A. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analysis. Ottawa Health Research Institute Web site. http://www.ohri.ca/programs/clinical–epidemiology/oxford.htm. Accessed: June 15, 2012.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (Grant No. 81200551 and 81270841). No funding bodies played any role in study design, data collection and analysis, decision to publish, or preparation this manuscript. The authors would like to thank their colleagues and staff in the Chinese Cochrane Centre for their help.
Author information
Authors and Affiliations
Contributions
W.Q. contributed to the conception and design of the study, C.D., H.Y. and L.L. wrote the main manuscript text and L.Y. and Y.L. prepared figures 1–8. C.D. and L.L. searched the studies, analyzed the data. L.H. and Y.L. participated in the acquisition of data and statistical analysis. W.J., Y.S., L.Z. and L.H. reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
De Hong, C., Liang Ren, L., Qiang, W. et al. Comparison of efficacy and safety of conventional laparoscopic radical prostatectomy by the transperitoneal versus extraperitoneal procedure. Sci Rep 5, 14442 (2015). https://doi.org/10.1038/srep14442
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep14442
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.