Abstract
Aberrant DNA methylation can be a potential genetic mechanism in non-small cell lung cancer (NSCLC). However, inconsistent findings existed among the recent association studies between cigarette smoking and gene methylation in lung cancer. The purpose of our meta-analysis was to evaluate the role of gene methylation in the smoking behavior of NSCLC patients. A total of 116 genes were obtained from 97 eligible publications in the current meta-analyses. Our results showed that 7 hypermethylated genes (including CDKN2A, RASSF1, MGMT, RARB, DAPK, WIF1 and FHIT) were significantly associated with the smoking behavior in NSCLC patients. The further population-based subgroup meta-analyses showed that the CDKN2A hypermethylation was significantly associated with cigarette smoking in Japanese, Chinese and Americans. In contrast, a significant association of RARB hypermethylation and smoking behavior was only detected in Chinese but not in Japanese. The genes with altered DNA methylation were likely to be potentially useful biomarkers in the early diagnosis of NSCLC.
Similar content being viewed by others
Introduction
Non-small-cell lung carcinoma (NSCLC) is a major type of epithelial lung cancer causing a serious hazard to human health1,2. The mortality of lung cancer was higher than that of any other malignant tumors among men and women in China3 and the incidence of lung cancer has been rising year by year4. Early detection is the key method to improve the survival of lung cancer patients5.
Cigarette smoking is the top risk factor which is attributed to more than four out of five cases of lung cancers6. Up to date, a handful of candidate genes have been investigated the association with cigarette smoking7,8. Epigenetic inhibition of gene expression is a potential cause for initiation and progression of lung cancer8. DNA methylation, a reversible epigenetic modification, plays an important role in gene expression at the very early stage of NSCLC9. Identification of aberrantly-methylated smoke-related genes may have potential in the early diagnosis of NSCLC.
Aberrant promoter methylation of smoking related genes has been reported in lung cancer patients7, but an unanimous conclusion could not be reached even in the same ethnic population10,11. Although several meta-analyses have reported the results of individual genes in patients with NSCLC, most of the current methylation studies were involved with a small number of samples that might produce spurious results. The purpose of our study was to perform an overview of all the candidate genes rather than single gene associated with smoking in NSCLC patients. Our meta-analysis would help identify the genes with robust findings across the studies in different ethnic populations.
Methods
Selection criteria of eligible studies
We searched the available studies through October 27, 2014 in the PubMed (English), CNKI and Wanfang (Chinese) literature databases using the corresponding combination: “(smok* OR nonsmok* OR clinic*) AND lung cancer AND (methylation OR epigenetic silencing)”. The inclusion criteria for the studies involved in this meta-analysis met the following criteria: 1) they were conducted in non-small cell lung cancer patients; 2) the subjects in every study comprised nonsmokers and smokers (former smokers and/or current smokers); 3) odds ratio (OR) with 95% confidential interval (CI) was included.
Data Extraction
All the datasets were extracted independently by two reviewers using a standard protocol. For each eligible study, we collected information regarding the names of first authors, publication year, ethnicity, country of origin, histology of lung cancer, types of biological specimen, number of participants, methylation status, smoking status, the method for methylation detection and OR with 95% CI.
Meta-analysis
The meta-analysis was performed using the Review Manager software (version 5.2, Cochrane Collaboration, Oxford, United Kingdom)12. The combined ORs and the corresponding 95% CIs were calculated and demonstrated in the forest plots using the fixed or the random effects model. A fixed-effect model was applied for the meta-analysis with moderate heterogeneity (I2 < 50%), otherwise a random-effect model was used13. Funnel plots were used to check whether there was obvious publication bias among the involved studies. P values less than 0.05 were considered to be significant.
Results
As shown in the Fig. 1, our initial search for the genetic studies of NSCLC retrieved 1724 articles from PubMed, CNKI and Wanfang literature databases. Among the retrieved studies, there were 1061 irrelevant studies, 412 studies without methylation data, 77 studies without the histological types of lung cancer, 15 studies with duplicate data, 26 only involved in risk factors and 36 studies without smoking status of participants. At last, a total of 97 eligible association studies between smoking and nonsmoking NSCLC patients were included in the current meta-analyses. There were 14 genes involved in at least three studies, 13 genes involved in two studies and 89 genes involved in one study.
Smoking behavior was evaluated for its contribution to the methylation status of 116 genes in NSCLC patients. Among these genes, 14 hypermethylated and 12 hypomethylated genes were shown to be associated with the smoking behavior. Six hypermethylated and eight hypomethylated genes were reported to be associated with smoking in one study (p < 0.05, Dataset 1). In addition, four hypermethylated and one hypomethylated genes were reported to be associated with smoking behavior in two independent studies (p < 0.05, Dataset 1).
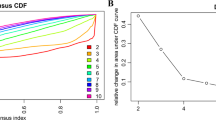
For 14 genes reported in at least three studies (Dataset 1), no evidence of statistical heterogeneity was observed for nine genes, including CDKN2A (I2 = 38%), MGMT (I2 = 19%), CDH13 (I2 = 38%), RARB (I2 = 0%), DAPK (I2 = 27%), WIF1 (I2 = 0%), MLH1 (I2 = 0%), PTEN (I2 = 0%) and CDH1 (I2 = 0%). No visual bias was shown in the meta-analyses of the above nine genes (Fig. 2). Our data also demonstrated a significant heterogeneity of the rest five genes that comprised RASSF1 (I2 = 57%), RUNX3 (I2 = 56%), SFRP1 (I2 = 55%), FHIT (I2 = 52%) and APC (I2 = 69%). Therefore, random-effect tests were applied for meta-analysis of the above five genes. Their funnel plots were shown in Fig. 2.
As shown in Table 1, meta-analysis of CDKN2A gene was involved with 36 studies between 2957 smoking and 1192 nonsmoking NSCLC patients. Our results indicated that CDKN2A hypermethylation was significantly associated with smoking risk in NSCLC patients (the overall OR = 2.33, 95% CI = 1.96–2.77, p < 0.00001). Meta-analysis of the association between RASSF1 hypermethylation and smoking behavior among 1046 smoking NSCLC patients and 441 nonsmoking NSCLC patients indicated a statistical difference (the overall OR = 1.75, 95% CI = 1.15–2.65, p = 0.008). The same consequences were also found in the other five genes including MGMT (the overall OR = 2.51, 95% CI = 1.81–3.46, p < 0.00001), RARB (the overall OR = 1.77, 95% CI = 1.29–2.42, p = 0.0004), DAPK (the overall OR = 2.04, 95% CI = 1.40–2.99, p = 0.0002), WIF1 (the overall OR = 1.62, 95% CI = 1.04–2.53, p = 0.03) and FHIT (the overall OR = 2.18, 95% CI = 1.33–5.95, p = 0.007). Our meta-analyses were unable to find statistical association with smoking for the methylation of the rest 7 genes, including CDH13, RUNX3, SFRP1, MLH1, APC, PTEN and CDH1.
Subgroup meta-analyses by ethnic populations were also performed for CDKN2A, RASSF1, CDH13 and RARB. As shown in Fig. 3, our results showed that significant association between cigarette smoking and CDKN2A hypermethylation existed in Japanese from 10 studies (OR = 3.61, 95% CI = 2.52–5.18), Americans from 6 studies (OR = 1.60, 95% CI = 1.15–2.22) and Chinese from 12 studies (OR = 2.47, 95% CI = 1.39–4.41). In addition, there was a significant ethnic difference in the meta-analysis of RARB gene. We found a statistical difference between RARB hypermethylation and smoking status in Chinese (OR = 2.05, 95% CI = 1.39–3.03, I2 = 0) but not in Japanese (p = 0.50, I2 = 94%, Fig. 4). Subgroup meta-analyses of RASSF1 and CDH13 were unable to observe any significant results in each ethnic population (Fig. 5 and Fig. 6). The funnel plots of four genes showed there was no publication bias among the above meta-analyses (Fig. 7).
Discussion
In the present study, a comprehensive overview of genetic association studies was performed for the susceptibility of smoking patients of NSCLC. Our meta-analyses mainly focused on 14 tumor suppressor genes (≥3 studies per gene). Seven NSCLC-associated genes (CDKN2A, RASSF1, MGMT, RARB, DAPK, WIF1 and FHIT) hypermethylation showed significant evidences in the smoking NSCLC patients compared with nonsmoking NSCLC patients. Subgroup meta-analyses by ethnic populations found that CDKN2A hypermethylation was a common risk factor of cigarette smoking in NSCLC patients, however, RARB hypermethylation was only found in Chinese.
Smoking is the main cause of lung cancer14,15, which can be associated with the calcium signaling and the other signaling pathways16,17,18,19. Aberrant methylation of gene promoters induced by cigarette carcinogens was shown to be associated with cancer occurrence and tumor suppressor gene inactivation20. Cigarette smoking was shown to induce DNMT1 accumulation and subsequent hypermethylation of the tumor suppressor gene that might cause tumorigenesis and poor prognosis in NSCLC patients21.
Cyclin-dependent kinase inhibitor 2A (CDKN2A) has two alternative transcripts that playing an important role in the p53 and pRB tumor suppressor pathways22. Tobacco carcinogens were shown to raise promoter methylation and then down-regulate the expression of CDKN2A gene23, which might lead to tumorigenesis. Ras-association domain family (RASSF1) and O-6-methylguanine DNA methyltransferase (MGMT) gene are both involved in lung cancer development in different human lung cell lines24,25. Cigarette smoking led to the changes in expression and promoter methylation of MGMT and RASSF126. Retinoic acid receptor beta (RARB) encoded a receptor mediating cellular signaling in embryonic morphogenesis, cell growth and differentiation27,28. Death-associated protein kinase (DAPK), a tumor suppressor gene, encodes a novel serine/threonine kinase linked with loss of expression in cancers29,30. Fragile histidine triad (FHIT) gene is located in the most common fragile site that is easy to be rearranged with the exposure in tobacco and other carcinogens, finally causing malignant transformation31. WNT inhibitory factor 1 (WIF1), as another tumor suppressor gene, has been found to be epigenetically silenced in various cancers including NSCLC32. Our results indicated that the hypermethylation of these genes were associated with cigarette smoking in the development of NSCLC.
Our meta-analyses aimed to provide a comprehensive list of aberrantly methylated genes in the smoking NSCLC patients. Compared with the meta-analysis of CDKN2A by Zhang et al33, our study was involved with a total of 2957 smoking patients and 1192 nonsmoking patients, which provided a much larger sample size than 2037 smoking patients and 765 nonsmoking patients in the study by Zhang et al33. In addition, our study was involved with the meta-analysis of 14 genes, among which 10 genes (including MGMT, DAPK, FHIT, CDH13, RARB, SFRP1, PTEN, CDH1, WIF1 and APC) hadn't been included by previous meta-analysis studies. Moreover, the meta-analysis by Liu et al.34 showed that RASSF1 gene promoter methylation was not associated with smoking behaviour in NSCLC patients. Our meta-analysis of RASSF1 methylation involved with 14 studies, which was 6 more than that of Liu et al.34. The smaller sample size might be the reason for the negative results in the meta-analysis by Liu et al.34.
Previous studies found mixed results regarding to racial disparities in NSCLC35. Our population-based subgroup meta-analyses showed that significant association of CDKN2A hypermethylation existed in Japanese, Chinese and American populations. However, RARB hypermethylation was only found in Chinese but not in Japanese.
There were several potential limitations in our study. Firstly, selection bias might exist since publications only in English and Chinese were included in the current meta-analyses, which could affect the results in a certain extent. Secondly, the main ethnicities of the current meta-analyses were Chinese, Japanese and Americans. Studies in other ethnic populations were needed in the near future to explore the contribution of gene methylation to the smoking in NSCLC. Thirdly, the effects of genetic factors on NSCLC risk might be confounded by gender36 and age37, therefore better design were warranted to avoid these confounding factors in the future. Lastly, our meta-analysis focused on gene with at least three independent studies and this might prevent those genes reported in two large scale smokers-nonsmokers studies from being included in the current meta-analysis.
In conclusion, we identified significant associations between seven genes (CDKN2A, RASSF1, MGMT, RARB, DAPK, WIF1 and FHIT) and smoking behavior in non-small cell lung cancer patients. CDKN2A hypermethylation was a common risk factor of smoking behavior in NSCLC patients, however, RARB hypermethylation was only found as a risk factor of smoking in Chinese but not in other populations.
References
Takeda, K., Hida, T., Sato, T., Ando, M., Seto, T., Satouchi, M. et al. Randomized phase III trial of platinum-doublet chemotherapy followed by gefitinib compared with continued platinum-doublet chemotherapy in Japanese patients with advanced non-small-cell lung cancer: results of a west Japan thoracic oncology group trial (WJTOG0203). J Clin Oncol 28, 753–60 (2010).
Pao, W. & Chmielecki, J. Rational, biologically based treatment of EGFR-mutant non-small-cell lung cancer. Nat Rev Cancer 10, 760–74 (2010).
Chen, W., Zheng, R., Zhang, S., Zhao, P., Zeng, H. & Zou, X. Report of cancer incidence and mortality in China, 2010. Ann Transl Med 2, 61 (2014).
Siegel, R., Naishadham, D. & Jemal, A. Cancer statistics, 2012. CA Cancer J Clin 62, 10–29 (2012).
Byers, L. A. & Rudin, C. M. Small cell lung cancer: Where do we go from here? Cancer (2014).
Xie, D., Lan, L., Huang, K., Chen, L., Xu, C., Wang, R. et al. Association of p53/p21 expression and cigarette smoking with tumor progression and poor prognosis in non-small cell lung cancer patients. Oncol Rep 32, 2517–26 (2014).
Tessema, M., Yingling, C. M., Liu, Y., Tellez, C. S., Van Neste, L., Baylin, S. S. et al. Genome-wide unmasking of epigenetically silenced genes in lung adenocarcinoma from smokers and never smokers. Carcinogenesis 35, 1248–57 (2014).
Tessema, M., Yu, Y. Y., Stidley, C. A., Machida, E. O., Schuebel, K. E., Baylin, S. B. et al. Concomitant promoter methylation of multiple genes in lung adenocarcinomas from current, former and never smokers. Carcinogenesis 30, 1132–8 (2009).
Kwon, Y. J., Lee, S. J., Koh, J. S., Kim, S. H., Lee, H. W., Kang, M. C. et al. Genome-wide analysis of DNA methylation and the gene expression change in lung cancer. J Thorac Oncol 7, 20–33 (2012).
Yanagawa, N., Tamura, G., Oizumi, H., Endoh, M., Sadahiro, M. & Motoyama, T. Inverse correlation between EGFR mutation and FHIT, RASSF1A and RUNX3 methylation in lung adenocarcinoma: relation with smoking status. Anticancer Res 31, 1211–4 (2011).
Nakata, S., Sugio, K., Uramoto, H., Oyama, T., Hanagiri, T., Morita, M. et al. The methylation status and protein expression of CDH1, p16(INK4A) and fragile histidine triad in nonsmall cell lung carcinoma: epigenetic silencing, clinical features and prognostic significance. Cancer 106, 2190–9 (2006).
Jiang, H., Sun, M. W., Hefright, B., Chen, W., Lu, C. D. & Zeng, J. Efficacy of hypocaloric parenteral nutrition for surgical patients: a systematic review and meta-analysis. Clin Nutr 30, 730–7 (2011).
Coory, M. D. Comment on: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol 39, 932 (2010).
Gates, P., Jaffe, A. & Copeland, J. Cannabis smoking and respiratory health: consideration of the literature. Respirology 19, 655–62 (2014).
Xie, A., Croce, B. & Tian, D. H. Smoking and lung cancer. Ann Cardiothorac Surg 3, 221 (2014).
Tan, Q., Wang, G., Huang, J., Ding, Z., Luo, Q., Mok, T. et al. Epigenomic analysis of lung adenocarcinoma reveals novel DNA methylation patterns associated with smoking. Onco Targets Ther 6, 1471–9 (2013).
Suda, K., Tomizawa, K., Yatabe, Y. & Mitsudomi, T. Lung cancers unrelated to smoking: characterized by single oncogene addiction? Int J Clin Oncol 16, 294–305 (2011).
Uimonen, K., Merikallio, H., Paakko, P., Harju, T., Mannermaa, A., Palvimo, J. et al. GASC1 expression in lung carcinoma is associated with smoking and prognosis of squamous cell carcinoma. Histol Histopathol 29, 797–804 (2014).
Massion, P. P., Zou, Y., Chen, H., Jiang, A., Coulson, P., Amos, C. I. et al. Smoking-related genomic signatures in non-small cell lung cancer. Am J Respir Crit Care Med 178, 1164–72 (2008).
Ling, Q., Shi, W., Huang, C., Zheng, J., Cheng, Q., Yu, K. et al. Epigenetic silencing of dual oxidase 1 by promoter hypermethylation in human hepatocellular carcinoma. Am J Cancer Res 4, 508–17 (2014).
Lin, R. K., Hsieh, Y. S., Lin, P., Hsu, H. S., Chen, C. Y., Tang, Y. A. et al. The tobacco-specific carcinogen NNK induces DNA methyltransferase 1 accumulation and tumor suppressor gene hypermethylation in mice and lung cancer patients. J Clin Invest 120, 521–32 (2010).
Kobayashi, T., Wang, J., Al-Ahmadie, H. & Abate-Shen, C. ARF regulates the stability of p16 protein via REGgamma-dependent proteasome degradation. Mol Cancer Res 11, 828–33 (2013).
Jarmalaite, S., Kannio, A., Anttila, S., Lazutka, J. R. & Husgafvel-Pursiainen, K. Aberrant p16 promoter methylation in smokers and former smokers with nonsmall cell lung cancer. Int J Cancer 106, 913–8 (2003).
Beckedorff, F. C., Ayupe, A. C., Crocci-Souza, R., Amaral, M. S., Nakaya, H. I., Soltys, D. T. et al. The intronic long noncoding RNA ANRASSF1 recruits PRC2 to the RASSF1A promoter, reducing the expression of RASSF1A and increasing cell proliferation. PLoS Genet 9, e1003705 (2013).
Ekim, M., Caner, V., Buyukpinarbasili, N., Tepeli, E., Elmas, L. & Bagci, G. Determination of O(6)-methylguanine DNA methyltransferase promoter methylation in non-small cell lung cancer. Genet Test Mol Biomarkers 15, 357–60 (2011).
Word, B., Lyn-Cook, L. E., Jr, Mwamba, B., Wang, H., Lyn-Cook, B. & Hammons, G. Cigarette smoke condensate induces differential expression and promoter methylation profiles of critical genes involved in lung cancer in NL-20 lung cells in vitro: short-term and chronic exposure. Int J Toxicol 32, 23–31 (2013).
Evans, T. R. & Kaye, S. B. Retinoids: present role and future potential. Br J Cancer 80, 1–8 (1999).
Moison, C., Senamaud-Beaufort, C., Fourriere, L., Champion, C., Ceccaldi, A., Lacomme, S. et al. DNA methylation associated with polycomb repression in retinoic acid receptor beta silencing. FASEB J 27, 1468–78 (2013).
Ye, M., Li, D., Zhou, F., Guo, Q. & Xia, B. Epigenetic regulation of death-associated protein kinase expression in primary gastric cancers from Chinese patients. Eur J Cancer Prev 21, 241–6 (2012).
Hu, S. L., Kong, X. Y., Cheng, Z. D., Sun, Y. B., Shen, G., Xu, W. P. et al. Promoter methylation of p16, Runx3, DAPK and CHFR genes is frequent in gastric carcinoma. Tumori 96, 726–33 (2010).
Kim, J. S., Kim, H., Shim, Y. M., Han, J., Park, J. & Kim, D. H. Aberrant methylation of the FHIT gene in chronic smokers with early stage squamous cell carcinoma of the lung. Carcinogenesis 25, 2165–71 (2004).
Liu, Y. L., Yang, H. P., Zhou, X. D., Gong, L., Tang, C. L. & Wang, H. J. The hypomethylation agent bisdemethoxycurcumin acts on the WIF-1 promoter, inhibits the canonical Wnt pathway and induces apoptosis in human non-small-cell lung cancer. Curr Cancer Drug Targets 11, 1098–110 (2011).
Zhang, B., Zhu, W., Yang, P., Liu, T., Jiang, M., He, Z. N. et al. Cigarette smoking and p16INK4alpha gene promoter hypermethylation in non-small cell lung carcinoma patients: a meta-analysis. PLoS One 6, e28882 (2011).
Liu, W. J., Tan, X. H., Guo, B. P., Ke, Q., Sun, J. & Cen, H. Associations between RASSF1A promoter methylation and NSCLC: a meta-analysis of published data. Asian Pac J Cancer Prev 14, 3719–24 (2013).
Murphy, S. E., Park, S. S., Thompson, E. F., Wilkens, L. R., Patel, Y., Stram, D. O. et al. Nicotine N-glucuronidation relative to N-oxidation and C-oxidation and UGT2B10 genotype in five ethnic/racial groups. Carcinogenesis 35, 2526–2533 (2014).
Siegel, R., Ma, J., Zou, Z. & Jemal, A. Cancer statistics, 2014. CA Cancer J Clin 64, 9–29 (2014).
Tantraworasin, A., Lertprasertsuke, N., Kongkarnka, S., Euathrongchit, J., Wannasopha, Y. & Saeteng, S. Retrospective study of ALK rearrangement and clinicopathological implications in completely resected non- small cell lung cancer patients in Northern Thailand: role of screening with D5F3 antibodies. Asian Pac J Cancer Prev 15, 3057–63 (2014).
Acknowledgements
The research was supported by the grants from National Natural Science Foundation of China (31100919 and 81371469), Natural Science Foundation of Zhejiang Province (LR13H020003), K. C. Wong Magna Fund in Ningbo University and Ningbo Natural Science Foundation (2014A610235), Zhejiang Provincial Bureau of Traditional Chinese Medicine (2013ZZ003) and the Sciences Technology Department of Zhejiang Province (2013F2005).
Author information
Authors and Affiliations
Contributions
T.H., X.C., S.D. and M.Y. contributed to the conception, design and final approval of the submitted version. Q.H., Z.D., H.M., Y.X., Y.F., H.Y., R.W. and C.Z. contributed to the meta-analysis, interpretation of data and completion of figures and tables. All the authors read and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Huang, T., Chen, X., Hong, Q. et al. Meta-analyses of gene methylation and smoking behavior in non-small cell lung cancer patients. Sci Rep 5, 8897 (2015). https://doi.org/10.1038/srep08897
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep08897
This article is cited by
-
Environment factors, DNA methylation, and cancer
Environmental Geochemistry and Health (2023)
-
Molecular subtypes based on DNA methylation predict prognosis in lung squamous cell carcinoma
BMC Cancer (2021)
-
Meta-Analysis Based on Nonconvex Regularization
Scientific Reports (2020)
-
CHRNA5 and CHRNA3 polymorphism and lung cancer susceptibility in Palestinian population
BMC Research Notes (2018)
-
A systematic review and meta-analysis: Association between MGMT hypermethylation and the clinicopathological characteristics of non-small-cell lung carcinoma
Scientific Reports (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.