Abstract
We investigated the associations between within-visit blood pressure variability (BPV) and risk factors for cardiovascular disease (CVD). The study subjects included 17,795 people aged 40–74 years who underwent health check-ups in Aichi Prefecture, Japan and completed two blood pressure measurements. Subjects were categorized into three groups according to the difference of systolic blood pressure (ΔSBP), namely, low-BPV (≤10 mmHg), moderate-BPV (11–20 mmHg) and high-BPV (>20 mmHg). Subjects were also divided into three categories as those without prediabetes (glycosylated hemoglobin A1c [HbA1c] < 5.7%), prediabetes (HbA1c 5.7–6.4%) and diabetes (HbA1c ≥ 6.5% or under treatment for diabetes). The proportion of prediabetes and diabetes were significantly higher in subjects with high-BPV than in those with low-BPV after adjusting for age, sex and mean SBP (odds ratio [95% confidence interval] was 1.16 [1.01–1.33] for prediabetes and 1.33 [1.06–1.66] for diabetes). Other CVD risk factors were not associated with high-BPV after the adjustment. In conclusion, increased within-visit BPV was significantly associated with the prevalence of prediabetes and diabetes, independent of mean SBP, in a large general population. Therefore, assessing BPV in a single visit may help to identify subjects at increased risk of impaired glycemic control.
Similar content being viewed by others
Introduction
Blood pressure variability (BPV) is now thought to be a risk factor for cardiovascular diseases (CVD)1,2. Recent data suggest that BPV persisting across several clinic visits (i.e., long-term BPV) is associated with stroke3,4, coronary heart disease and all-cause mortality5. BPV measured over 24 h by ambulatory blood pressure monitoring (ABPM) (i.e., short-term BPV) is also associated with CVD events6,7. However, few studies have examined the importance of BPV measured during a single clinic visit (i.e., very-short-term BPV). Recent studies have demonstrated that within-visit BPV is associated with metabolic syndrome score8, target organ damage (left ventricular hypertrophy and albuminuria)9 and the risk of stroke3,4, but not with overall CVD or all-cause mortality10,11. If it is associated with specific CVD risk factors, within-visit BPV could be a clinically useful measure because it can be assessed in a single visit. Therefore, we sought to determine the associations between within-visit BPV and common CVD risk factors.
Results
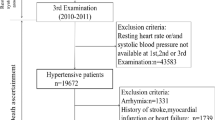
Overall, 312 821 subjects had complete data for CVD risk factors and had one or more BP measurement. We excluded 115 461 subjects who were taking antihypertensive drugs and/or had a history of cerebrovascular or cardiovascular diseases. We also excluded 188 487 subjects in whom only one value of blood pressure (BP) was recorded. After excluding these subjects, 17 795 subjects (6 907 men and 10 888 women) were included in the present analyses. There were no significant differences in the characteristics of subjects in whom BP was measured multiple times or once (Table 1).
The characteristics of subjects according to the BPV categories are shown in Table 2. Compared with subjects with low-BPV, those with high-BPV tended to be older and had higher BP, glycemic levels, lipid levels, waist circumference (WC) and body mass index (BMI). The prevalence of proteinuria was also higher in subjects with high-BPV, which may be explained by the higher prevalence of diabetes. There was no difference in estimated glomerular filtration rate (eGFR) or the proportions of male/female subjects.
After adjusting for age, sex, mean systolic BP (SBP), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), use of lipid-lowering medication, WC, BMI and current smoking, the prevalence of prediabetes and diabetes were higher in subjects with high-BPV than those with low-BPV (odds ratio [OR] 1.16, 95% confidence interval [CI] 1.00–1.33 for prediabetes; and OR 1.39, 95% CI 1.11–1.75 for diabetes). Other CVD risk factors were not associated with high-BPV after adjusting for age, sex and mean SBP (Table 3).
As BPV is closely related to the mean SBP, the prevalence of prediabetes/diabetes was compared in each mean SBP category. The prevalence of prediabetes/diabetes were higher in subjects with high-BPV compared to those with low-BPV in each mean SBP category (34.4% vs. 32.5%, 43.8% vs. 36.1% and 44.0% vs. 40.7% in high-BPV vs. low-BPV for mean SBP of <120, 120–139 and ≥140 mm Hg, respectively). However, the difference was statistically significant only in subjects with mean SBP of 120–140 mm Hg after adjustment; the ORs were 1.00 (0.70–1.41), 1.34 (1.11–1.63) and 1.12 (0.92–1.37) for mean SBP of <120, 120–139 and ≥140 mm Hg, respectively, after adjustment.
Discussion
In the present study, high within-visit BPV was significantly associated with the prevalence of prediabetes and diabetes, independent of mean SBP, in a large general population. Our results suggest that measuring BPV at a single visit may help to identify subjects at increased risk of having impaired glycemic control.
Recent data suggest that BPV is a strong prognostic factor for stroke, coronary heart disease and all-cause mortality1,2,3,4,5,6,7. Several methods are available to measure BPV; visit-to-visit BPV is an index of long-term BPV, while 24-h BPV assessed by ABPM is an index of short-term BPV1,2. Both of these measurements of BPV are useful for assessing the risk of CVD3,12.
Within-visit BPV, an index of very-short-term BPV, is related to autonomic cardiovascular modulation13, mental stress14 and arterial stiffness15. However, few studies have evaluated the importance of BPV measured in a single clinic visit. One study revealed that within-visit BPV is associated with the risk of stroke3, but other studies found no association between within-visit BPV and the risks of all-cause or CVD mortality10,11. Different definitions of high-BPV might explain this discrepancy. Of note, BPV was not associated with CVD risk in studies where high-BPV was defined as the highest quintile or quartile of BPV10,11. By contrast, Rothwell et al. defined high-BPV as the highest decile of BPV3 and our cutoff point (20 mm Hg) is close to the 95th percentile of BPV. Thus, the highest level of BPV might be associated with the risk of CVD, which should be examined in future studies.
The prevalence of prediabetes was associated with within-visit BPV in this study. Previous studies have shown that subjects with diabetes had greater 24-h BPV compared with non-diabetic subjects16 and glycosylated hemoglobin A1c (HbA1c) was associated with 24-h BPV in subjects with diabetic neuropathy17. A recent study revealed that fasting plasma glucose was correlated with within-visit BPV8, but the data were not adjusted for mean SBP. To the best of our knowledge, our study was the first to show an association between prediabetes and within-visit BPV and that the association was independent of mean SBP in a large general population.
The mechanism underlying the association between prediabetes and BPV is somewhat unclear and needs to be considered. One possible mechanism is endothelial injury caused by impaired glucose tolerance18,19. BPV is related to abnormalities in endothelial and vascular smooth muscle function, which suggests BPV may influence the pathogenesis of CVD20. Another mechanism could be sympathetic overactivity and autonomic imbalance initiated by impaired glucose tolerance18,21 and these changes may lead to impaired ability to control BPV22,23, as circadian BP abnormality24. Further studies are needed to confirm these findings and to better understand the underlying mechanisms.
Several limitations of this study should be mentioned. First, we defined prediabetes and diabetes according to HbA1c rather than fasting plasma glucose. HbA1c is an index of long-term glycemic control and can be used to define prediabetes and diabetes25. Future studies should assess whether prediabetes defined according to fasting plasma glucose is also associated with high-BPV. Second, BPV was based on first and second measurements of BP. Although the first BP measurement is often considered unreliable26, a recent study suggested that the first BP measurement is related to CVD risk8. Additionally, it can be an easy and useful measure if difference of only two measurements of SBP reflects the risk of diabetes. Third, although mean SBP was adjusted in this study, the strong relationship between the mean SBP and BPV should be considered. The association between BPV and impaired glycemic status was observed strongly in subjects with prehypertensive range, but the association was weak in subjects with normotension or hypertension, which should be confirmed in another study. Fourth, selection bias should be considered because BP was measured twice in just 9% of the subjects who underwent health check-ups. However, there were no significant differences in the first BP measurement or other clinical factors between subjects who underwent one or multiple BP measurements. Although the guideline of this program recommends measurement of BP twice, single measurement of BP is also accepted and it depends on each facility. Fifth, considering the cross-sectional design of this study, we could not determine the cause-effect relationship between BPV and prediabetes. Unfortunately, we lack the data on heart rate variability which reflects antonomic dysfunction and there is no information about detailed glycemic status in the past. Whether treating subjects with prediabetes and high-BPV can prevent the progression to diabetes should be examined in longitudinal studies.
In conclusion, we have demonstrated that high within-visit BPV was significantly associated with the prevalence of prediabetes and diabetes, independent of mean SBP, in a large general population. Therefore, we consider that glycemic parameters should be monitored in subjects with high-BPV. Because BPV can be assessed in a single visit, it may be an easy and useful measure to identify subjects at increased risk of impaired glycemic control.
Methods
Study population
The subjects were people who underwent specific health check-ups and health guidance between April 2008 and March 2009 as part of the Tokutei-Kenshin (Special Health Check-up) programme in Aichi Prefecture, Japan. This programme was started by the Japanese government in 2008 to facilitate the early diagnosis and interventions for metabolic syndrome27. The target population comprises all Japanese citizens aged 40–74 years. The present study included subjects with complete data for at least two SBP and diastolic BP (DBP) measurements in one visit and for the following CVD risk factors: HbA1c, HDL-C, LDL-C, TG, WC and BMI. The guideline recommends taking a rest of ≥5 min before taking the first BP measurement and a rest of ≥1 min before taking the second BP measurement using automated machines. The first and second measurement of BP were used for the analysis because very few subjects had data on the third measurement of BP (n = 269). Serum creatinine was measured in most of the subjects. According to the program's guidelines proposed by the Japanese government, the clinician could measure either fasting plasma glucose or HbA1c as an index of glycemic control. Therefore, fasting plasma glucose was unknown in most of the study subjects with complete data for the other variables listed above.
All of the subjects completed a self-administered questionnaire to document their current medications for hypertension, diabetes and hyperlipidemia, history of cardiovascular and cerebrovascular diseases and smoking habits (current smoker or not). BP measurement and blood and urine sampling were performed at the local medical institutions. HbA1c values are presented as National Glycohemoglobin Standardization Program (NGSP) values, which were calculated with the following equation: HbA1c (NGSP, %) = 1.02 × HbA1c (Japan Diabetes Society, %) + 0.25%. Subjects currently taking antihypertensive drugs and those with a history of cerebrovascular or cardiovascular diseases reported in the self-administered questionnaire were excluded from the present analyses, because antihypertensive medication influences BPV and as the purpose of this study is to find the non-invasive methods (e.g. BPV in a single visit) to identify subjects at increased risk for cerebrovascular or cardiovascular diseases.
This study was conducted by the Aichi Chronic Kidney Disease Epidemiology Conference with support from the Aichi Kidney Foundation. Written informed consent was not required as only the existing information was used. This study was conducted in accordance with the Ethical Guidelines for Epidemiological Research by Japanese government. This study was approved by the Ethics Committee of Nagoya University School of Medicine (approval number 679).
Definitions of BPV categories and CVD risk factors
As previous described8,9, subjects were classified into 3 groups according to the maximum minus minimum systolic BP (ΔSBP) value as low-BPV (ΔSBP ≤ 10 mmHg) moderate-BPV (ΔSBP 11–20 mmHg) and high-BPV (ΔSBP > 20 mmHg). HbA1c was used as a marker of glycemic status. Subjects were divided into those without prediabetes (HbA1c < 5.7%) and those with prediabetes (HbA1c 5.7–6.4%) or diabetes (HbA1c ≥ 6.5% or under treatment for diabetes)25,28. Low HDL-C was defined as HDL-C < 40 mg/dL in men and <50 mg/dL in women, or the use of lipid-lowering drugs. High LDL-C was defined as LDL-C ≥ 160 mg/dL or the use of lipid-lowering drugs. Borderline-high TG was defined as TG 150–199 mg/dL and high TG was defined as TG ≥ 200 mg/dL or the use of lipid-lowering drugs29. Elevated WC was defined based on criteria for Asians30 as WC ≥ 90 cm in men and ≥80 cm in women. Using criteria for Asians31, overweight was defined as BMI 23.0–27.4 kg/m2 and obesity was defined as BMI ≥ 27.5 kg/m2. The eGFR was calculated using the Japanese GFR equation32, as follows: eGFR (mL/min/1.73 m2) = 194 × serum creatinine−1.094 (mg/dL) × age−0.287 (years) (×0.739 if female). Reduced eGFR was defined as eGFR < 60 mL/min/1.73 m2.
Statistical analyses
We compared the characteristics of subjects between those who were included and those who were excluded from the study. We also compared the characteristics of subjects among the groups of high-BPV, moderate-BPV and low-BPV. The prevalences of CVD risk factors in the high-BPV and moderate-BPV groups were compared with the low-BPV group. ORs and 95% CI were calculated for each CVD risk factor using unconditional logistic regression analysis adjusted for age (as a continuous variable), sex, mean SBP, HDL-C, LDL-C, TG, use of lipid-lowering medication, WC, BMI and current smoking. HDL-C, LDL-C, TG and use of lipid-lowering medication were not included in the analyses of HDL-C, LDL-C and TG. WC and BMI were not included in the analyses of WC and BMI. Values of p < 0.05 in adjusted models were considered statistically significant. All analyses were carried out using STATA software version 9 (Stata Corp, College Station, TX, USA).
References
Parati, G., Ochoa, J. E., Salvi, P., Lombardi, C. & Bilo, G. Prognostic value of blood pressure variability and average blood pressure levels in patients with hypertension and diabetes. Diabetes Care. 36 Suppl 2S312–24 (2013).
Parati, G., Ochoa, J. E., Lombardi, C. & Bilo, G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 10, 143–155 (2013).
Rothwell, P. M. et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure and episodic hypertension. Lancet. 375, 895–905 (2010).
Rothwell, P. M. et al. ASCOT-BPLA and MRC Trial Investigators. Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol. 9, 469–80 (2010).
Mancia, G. et al. Blood pressure control and improved cardiovascular outcomes in the International Verapamil SR-Trandolapril Study. Hypertension 50, 299–305 (2007).
Hansen, T. W. et al. International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators. Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension 55, 1049–1057 (2010).
Kikuya, M. et al. Prognostic significance of blood pressure and heart rate variabilities: the Ohasama study. Hypertension 36, 901–906 (2000).
Shin, J. H. et al. Within-visit blood pressure variability: relevant factors in the general population. J Hum Hypertens. 27, 328–334 (2013).
Wei, F. F. et al. Beat-to-Beat, Reading-to-Reading and Day-to-Day Blood Pressure Variability in Relation to Organ Damage in Untreated Chinese. Hypertension 63, 790–796 (2014).
Muntner, P. et al. Within-visit variability of blood pressure and all-cause and cardiovascular mortality among US adults. J Clin Hypertens (Greenwich) 14, 165–171 (2012).
Schutte, R. et al. Within-subject blood pressure level–not variability–predicts fatal and nonfatal outcomes in a general population. Hypertension. 60, 1138–1147 (2012).
Eguchi, K., Hoshide, S., Schwartz, J. E., Shimada, K. & Kario, K. Visit-to-visit and ambulatory blood pressure variability as predictors of incident cardiovascular events in patients with hypertension. Am J Hypertens. 25, 962–968 (2012).
Parati, G., Saul, J. P., Di Rienzo, M. & Mancia, G. Spectral analysis of blood pressure and heart rate variability in evaluating cardiovascular regulation. A critical appraisal. Hypertension 25, 1276–1286 (1995).
Webb, A. J. & Rothwell, P. M. Physiological correlates of beat-to-beat, ambulatory and day-to-day home blood pressure variability after transient ischemic attack or minor stroke. Stroke 45, 533–538 (2014).
Liu, Y. P. et al. Do level and variability of systolic blood pressure predict arterial properties or vice versa? J Hum Hypertens. 28, 316–322 (2013).
Mokhtar, R. H., Ayob, A. & Mohd Noor, N. Blood pressure variability in patients with diabetes mellitus. Asian Cardiovasc Thorac Ann. 18, 344–348 (2010).
Liu, F. et al. Influence of HbA1c on short-term blood pressure variability in type 2 diabetic patients with diabetic nephropathy. J Zhejiang Univ Sci B. 14, 1033–1040 (2013).
Singleton, J. R., Smith, A. G., Russell, J. W. & Feldman, E. L. Microvascular complications of impaired glucose tolerance. Diabetes 52, 2867–2873 (2003).
Wykretowicz, A. et al. Endothelial function and baroreflex sensitivity according to the oral glucose tolerance test in patients with coronary artery disease and normal fasting glucose levels. Clin Sci (Lond). 109, 397–403 (2005).
Diaz, K. M. et al. Visit-to-visit and 24-h blood pressure variability: association with endothelial and smooth muscle function in African Americans. J Hum Hypertens. 27, 671–677 (2013).
De Angelis, K., Senador, D. D., Mostarda, C., Irigoyen, M. C. & Morris, M. Sympathetic overactivity precedes metabolic dysfunction in a fructose model of glucose intolerance in mice. Am J Physiol Regul Integr Comp Physiol. 302, R950–957 (2012).
Formes, K. J., Wray, D. W., O-Yurvati, A. H., Weiss, M. S. & Shi, X. Sympathetic cardiac influence and arterial blood pressure instability. Auton Neurosci. 118, 116–124 (2005).
Su, H., Wang, J., Zhu, Y., Wang, G. & Cheng, X. Discrepancy among three blood pressure readings within one measurement and relevant influencing factors. Blood Press Monit. 15, 152–157 (2010).
Gupta, A. K., Greenway, F. L., Cornelissen, G., Pan, W. & Halberg, F. Prediabetes is associated with abnormal circadian blood pressure variability. J Hum Hypertens. 22, 627–33 (2008).
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 33, S62–69 (2010).
Bovet, P. et al. Assessing the prevalence of hypertension in populations: are we doing it right? J Hypertens. 21, 509–517 (2003).
Mizushima, S. & Tsushita, K. [New Strategy on Prevention and Control of Noncommunicable Lifestyle-Related Diseases Focusing on Metabolic Syndrome in Japan.]. Asian Perspectives and Evidence on Health Promotion and Education. [Takashi Muto] [31–39] (Springer, Berlin, 2011).
Droumaguet, C. et al. DESIR Study Group. Use of HbA1c in predicting progression to diabetes in French men and women: data from an Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care 29, 1619–1625 (2006).
Expert Panel on Detection,. Evaluation,. and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 285, 2486–2497 (2001).
Alberti, K. G. et al. International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645 (2009).
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 363, 157–163 (2004).
Matsuo, S. et al. Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 53, 982–992 (2009).
Acknowledgements
The authors thank the members of the Aichi Prefectural National Health Insurance Association for their indispensable help with collecting data. This study was partly supported by the Aichi Kidney Foundation.
Author information
Authors and Affiliations
Contributions
R.O. analyzed data and mainly drafted the article, Y.Y., K.T., K.W., N.H. and S.M. provided intellectual content of critical importance to the work described and revised the article and all the authors approved the final version of the article to be published.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Okada, R., Yasuda, Y., Tsushita, K. et al. Within-visit blood pressure variability is associated with prediabetes and diabetes. Sci Rep 5, 7964 (2015). https://doi.org/10.1038/srep07964
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep07964
This article is cited by
-
Prevalence of prediabetes and associated factors among community members in rural Isingiro district
BMC Public Health (2023)
-
Long-term variability and change trend of systolic blood pressure and risk of type 2 diabetes mellitus in middle-aged Japanese individuals: findings of the Aichi Workers’ Cohort Study
Hypertension Research (2022)
-
Pathogenic connection between hypertension and type 2 diabetes: how do they mutually affect each other?
Hypertension Research (2022)
-
Implications of blood pressure variations in older populations
Hypertension Research (2019)
-
Association between within-visit systolic blood pressure variability and development of pre-diabetes and diabetes among overweight/obese individuals
Journal of Human Hypertension (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.