Abstract
The incidence of postoperative central nervous system infection (PCNSI) is higher than 5%–7%. Successful management of PCNSI requires a combined therapy of surgical debridement and long-term antibiotic treatment. In this study, Duraform soaked in a prepared bacterial solution was placed on the brain surface of rats to induce PCNSI. Virgin poly[(d,l)-lactide-co-glycolide] (PLGA) nanofibrous membranes (vehicle-control group) and vancomycin-eluting PLGA membranes (vancomycin-nanofibres group) were implanted. The wound conditions were observed and serial brain MRI and pathology examinations were performed regularly. PCNSI was consistently induced in a single, simple step. In the vehicle-control group, most rats died within 1 week and the survival rate was low (odds ratio = 0.0357, 95% confidence interval = 0.0057–0.2254). The wounds and affected cerebral tissues necrosed with purulence and increased in mass from the resulting PCNSI volumes. Initially, the mean PCNSI volumes showed no significant difference between the two groups. The PCNSI volume in the rats in the vancomycin-nanofibres group significantly decreased (P < 0.01) and the wound appearance was excellent. Pathologic examinations revealed that the necrosis and leukocyte infiltration area decreased considerably. The experimental results suggest that vancomycin-eluting PLGA nanofibres are favourable candidates for treating PCNSI after surgical debridement.
Similar content being viewed by others
Introduction
Postoperative central nervous system infection (PCNSI) in patients undergoing neurosurgical procedures is a severe illness that requires immediate attention. These infections can manifest themselves as a wound, a bone-flap infection, an epidural abscess, subdural emphysema, a brain abscess, or meningitis1,2,3. Published data show that the incidence of PCNSI is 5%–7%1,4,5 and can be as high as 10% when antibiotic prophylaxis is not administered. Many physicians believe that the incidence is even higher6,7,8. Multiple factors, including cerebral spinal fluid leakage, a clean-contaminated or dirty surgery, an emergency operation, an operation duration longer than 4 hours, reoperation and the male sex, can contribute to an increased risk of PCNSI3,4,5,7,8. Postoperative and posttraumatic infections containing foreign bodies or contaminated retained bone fragments, flaps and brain tissue must be managed. Hence, complete abscess excision and debridement through craniectomy or craniotomy is necessary9,10,11.
Following surgical intervention, parental antibiotic therapy is required. The recommended duration of antibiotic treatment therapy is long, usually 4–8 weeks depending on the therapeutic response and neuroimaging findings9,12. Vancomycin is widely used for treating brain abscesses from a haematogenous spread in postoperative neurosurgical patients who underwent trauma caused by methicillin-resistant Staphylococcus aureus1,11,13,14. Vancomycin should be administered intravenously for a minimum infusion period of 1 hour to minimise infusion-related adverse effects15. In addition, administering vancomycin to patients with a CNS infection requires more than 4–8 weeks of hospitalization, resulting in high hospital costs, the use of many drugs and a low life quality9,12. Furthermore, long-term vancomycin intravenous infusion may cause toxic and other adverse side effects11,15.
In our previous study16, we developed biodegradable vancomycin-loaded poly[(d,l)-lactide-co-glycolide] (PLGA) nanofibrous membranes and evaluated the release characteristics of vancomycin in the cerebral tissues of rats. The results suggested that biodegradable nanofibres can release high concentrations of vancomycin in the cerebral cavity for more than 8 weeks. In this paper, we propose a novel model for experimentally inducing PCNSI in rats. In addition, we demonstrate that biodegradable vancomycin-eluting PLGA nanofibrous membranes can be used to effectively treat PCNSI.
Results
By employing appropriate process parameters (including a proper solvent, polymer concentration and flow rate), we obtained electrospun nanofibrous membranes. Scanning electron micrographs of the electrospun nanofibres (under a magnification of 5,000x) showed the diameters of the spun vancomycin-eluting PLGA nanofibres to range from 375 to 1,200 nm and the porosity of the nanofibrous membranes was high. The model proposed in this study was adopted to consistently induce experimental PCNSI in the rats through a single, simple step; the model accurately represented the clinical situation and yielded reproducible results. Four rats died during the perioperative period; however, PCNSI models were created in 36 rats and confirmed through brain MRI examinations. All of the rats had a subcutaneous abscess, epidural or subdural emphysema and a brain abscess. The rats with PCNSI were randomly divided into two groups that each comprised 18 rats.
Survival rate
In the vehicle-control group, virgin (i.e., not loaded with a drug) PLGA nanofibrous membranes were implanted after the PCNSIs were induced. Vancomycin-eluting PLGA nanofibrous membranes were implanted into the rats in the vancomycin-nanofibres group. In the vehicle-control group, only two rats survived and the other 16 rats died within a few weeks after the operation (nine rats died in the first week, five rats died in the second and two rats died in the fourth). In the vancomycin-nanofibres group, 14 rats survived and four rats died. Two rats died within 1 week and the brain MRI findings on the day on which the vancomycin-eluting membrane was implanted revealed severe initial subdural emphysema and brain abscesses. The PCNSI volumes of these rats (first rat, 463.12 × 10−3 mL; second rat, 458.87 × 10−3 mL) were much higher than the mean PCNSI volume (283.25 ± 118.50 × 10−3 mL). A severe mass effect with midline shift and contralateral ventricle involvement was observed in the MRI image. The third rat died because of severe abdominal distention and a clear scalp wound and the fourth rat died after anaesthesia for the MRI examination. The survival rate in the vehicle-control group (with the virgin PLGA nanofibrous membrane) was much lower than that in the vancomycin-nanofibres group (with the vancomycin-eluting nanofibrous membrane) (odds ratio = 0.0357, 95% confidence interval = 0.0057–0.2254). The Survival curve for vancomycin-nanofibres group is statistically different from the vehicle-control group (P < 0.001). Figure 1 shows Kaplan-Meier curves of a representative survival study. The vancomycin-eluting nanofibrous membrane reduced the risk of death significantly. The mean survival time was 14.44 ± 16.55 days in the vehicle-control group and 46.06 ± 19.73 days in the vancomycin-nanofibres group. The survival time was significantly longer in the vancomycin-nanofibres group (P < 0.001).
Wound appearance
Before implantation of the membranes, the wounds were mildly dehiscent with or without purulence in both the vehicle-control and vancomycin-nanofibres groups (Figure 2 a1, b1 and c1). In the vehicle-control group, the wounds deteriorated progressively; some rats showed pus accumulation with scalp swelling around the surgical site, whereas other rats exhibited wound dehiscence with necrosis and discharge of an odourous pus from the wound. (Figure 2 a2, a3, b2 and b3) By contrast, the wounds of the rats in the vancomycin-nanofibres group were clear and intact. Hair regrowth and excellent healing were evident (Figure 2 c2 and c3). The culture data for all of the wounds revealed the presence of S. aureus.
Gross wound appearance.
a and b show rats from the vehicle-control group and c shows a rat from the vancomycin-nanofibres group. The number on the upper right corner of each image indicates the number of days after the implantation of the PLGA nanofibrous membrane. a1: scalp wound swelling with mild pus discharge. a2: severe wound swelling with eschar formation. a3: rat died and pus accumulation with necrotic brain tissue was noticed when the scalp wound was opened. b1: mild scalp wound swelling. b2: scalp wound necrosis and dehiscence with pus discharge. b3: rat died and exhibited purulence with necrotic brain tissue. c1: mild pus discharge. c2: wound healed adequately with a regrowth of hair. c3: scalp wound was excellent at the end of the study.
MRI examination
Serial brain MRI examinations were performed on the implantation day and at 1, 2, 4, 6 and 8 weeks after implantation of the membranes. Figures 3 and 4 show the serial MRI examination images of the rats in vehicle-control group and vancomycin-nanofibres group, respectively. The mean PCNSI volumes on the day of implantation were 273.18 ± 118.64 × 10−3 mL and 283.25 ± 118.50 × 10−3 mL in the vehicle-control group and vancomycin-nanofibres group, respectively. No significant difference was observed (P = 0.287). However, the volumes increased progressively in the vehicle-control group, whereas they decreased remarkably in the vancomycin-nanofibres group. Half of the rats died within 1 week because of infection area (PCNSI volume) enlargement and wound dehiscence with pus and necrotic brain tissue discharge and only nine rats underwent MRI examination after 1 week. During the first week, the mean volume was 377.94 ± 238.40 × 10−3 mL for the vehicle-control group and 189.94 ± 53.72 × 10−3 mL for the vancomycin-nanofibres group. The mean PCNSI volume was significantly greater in vehicle-control group (P < 0.05). In the vancomycin-nanofibres group, the PCNSI volumes were 127.86 ± 72.17 × 10−3 mL, 34.30 ± 21.88 × 10−3 mL, 31.74 ± 36.61 × 10−3 mL and 6.08 ± 9.61 × 10−3 mL at 2, 4, 6 and 8 weeks, respectively. The volumes decreased significantly (P < 0.01) (Figure 5). At end of this study, the brain MRI images of six rats (6/18) in the vancomycin-nanofibres group showed no PCNSI.
Serial brain-MRI images of the rats in the vehicle-control group.
a1 and a2 show different rats in the vehicle-control group. The number on the upper right corner of each image indicates the number of days after the implantation of the virgin PLGA nanofibrous membrane. a1: progressive enlargement and ingrowth of PCNSI were observed in the MRI images. The rat died on Day 24 and a large abscess formation with a severe mass effect was noticed. a2: Like most rats in the vehicle-control group, the rat died in 1 week. MRI images revealed that the PCNSI expanded rapidly with an increasing mass effect and contralateral ventricle involvement.
Serial brain MRI images of the rats in the vancomycin-nanofibres group.
The number on the upper right corner of each image indicates the number of days after the implantation of the vancomycin-eluting PLGA nanofibrous membrane. The PCNSI area decreased markedly and no inflammation was found at the end of the study (8 weeks). The arrow indicates the nanofibrous membrane, which degraded progressively.
PCNSI-volume change in the vehicle-control and vancomycin-nanofibres groups.
Data are expressed as mean values. The PCNSI volumes increased in the vehicle-control group and decreased in the vancomycin-nanofibres group as the number of postimplantation days increased. (* statistical significance P < 0.05,  statistical significance P < 0.01).
statistical significance P < 0.01).
Pathology
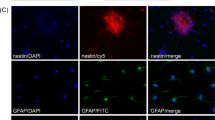
The rats were sacrificed and the brain tissues were obtained surgically on the day of and at 1, 2, 4, 6 and 8 weeks after the implantation of the PLGA membranes or when a rat died accidentally. Haematoxylin-and-eosin-stained sections were evaluated to determine the intensity of the inflammatory response. Figure 6 shows a microscopic image obtained during a pathology examination of a rat in the vehicle-control group (with virgin nanofibres). Marked inflammatory response and brain tissue necrosis with mononuclear (MN) and polymorphonuclear (PMN) leukocyte infiltration were noted. The necrotic centre of the abscesses as well as the intensity of MN and PMN leukocyte infiltration increased significantly over time. In the vancomycin-nanofibres group (Figure 7), the MN and PMN leukocyte infiltration areas decreased over time and no inflammation responses were observed 28 days after the implantation of the vancomycin-eluting nanofibrous membranes.
Microscopic images from the pathological examination of rats in the vehicle-control group at 0, 7, 14 and 21 days after the implantation of the virgin PLGA nanofibrous membranes.
The necrotic centre of the abscess (indicated by the black arrows) increased significantly over time. Marked increases in intensity of MN and PMN leukocyte infiltration were noted.
Microscopic images from the pathological examination of the rats in the vancomycin-nanofibres group at 0, 7, 14 and 28 days after the implantation of the vancomycin-eluting PLGA nanofibrous membranes.
An initial, intense PMN response was observed in the necrotic centres (indicated by a black arrow) of the PCNSIs. The MN and PMN leukocyte infiltration areas decreased over time and no inflammation response was observed 28 days after the implantation.
Discussion
Despite remarkable advances in antimicrobial therapy, neurosurgical techniques and neuroradiological diagnosis, brain abscesses and CNS infections remain a challenge and their mortality rates are still high17,18. Bacterial infection in surgery, especial CNS surgery, can be devastating and is associated with considerable morbidity and poor functional outcomes17,19. The management of postoperative infection requires surgical debridement, the removal of all necrotic tissue and implants and the administration of systemic antibiotics. Nevertheless, antibiotic treatment may be inadequate or ineffective in patients with poorly vascularized infected tissues8,9,12.
Among various antimicroorganisms, vancomycin is a commonly used antibiotic and a concentration-independent killer of gram-positive pathogens. Vancomycin should be administered intravenously for a minimum infusion period of 1 hours to minimise infusion-related adverse side effects such as nephrotoxicity, ototoxicity and thrombovytopenia15. Vancomycin exhibits concentration-independent activity against S. aureus. Pharmacodynamic studies have shown that the ratio of the area under the concentration-time curve to the minimum inhibitory concentration (AUC/MIC) is themost useful pharmacodynamic parameter for predicting vancomycin effectiveness15,20,21,22. On the basis of in vitro (animal and limited human) data, an AUC/MIC value of 400 has been established as the pharmacokinetic-pharmacodynamic target20,21,22,23. To achieve this target, a high vancomycin dose resulting in a high trough serum concentration is required. Although the administration of vancomycin is associated with certain adverse effects, it has been generally accepted that the potential benefit of a high drug dose outweighs the risk of the mostly reversible adverse effects23. The results of our previous study16 demonstrated that PLGA nanofibres can elute highly effective concentrations of vancomycin (i.e., an AUC/MIC ratio above 1,000–4,500) for more than 6 weeks after implantation. In addition to concentrations in the brain tissue, the concentrations in the fascia and skull have AUC/MIC ratios much greater than 400 for more than 8 weeks. By contrast, the vancomycin concentration in the local (treatment) area through intravenous infusion is much lower than the concentration in the blood. Antibiotics released at a concentration significantly higher than the MIC have considerable potential for rapid bacterial clearing24,25. The trough concentration can be increased to 15–20 mg/L to achieve a highly desirable AUC/MIC ratio of >400; however, the use of these high concentrations is not currently supported by any clinical trials20,26, mainly because higher trough concentrations increase the potential for toxicity20. Local delivery of vancomycin to the target site through a biodegradable vehicle enables easily attaining AUC/MIC ratios much higher than 400 and avoiding potential toxicity and side effects associated with intravenous infusion. The duration of intravenous antibiotic treatments is shorter and the related expenses of hospitalization, antibiotic treatment and repeated imaging examination can be minimised. Biodegradable antibiotic delivery systems are thus highly desirable for preventing and managing surgical infections27,28.
Delivering local antibiotics by using antibiotic-impregnated biodegradable or nonbiodegradable carriers has been proposed to provide a sustained release of antibiotics to infected areas, replacing intravenous antibiotics infusion. Studies have reported that vancomycin is effective even in low doses when delivered in polymethylmethacrylate (PMMA) cement spacers for osseous space maintenance and infection control25,29,30. The concentration of antibiotics eluted from the cement is much higher than the concentration achieved through systemic therapy. However, the nondegradability of PMMA drug delivery systems (i.e., the persistence of the carriers after delivery) limits their clinical application, especially in the CNS. The development of biodegradable carriers is considered advantageous because these carriers may reduce the risk of secondary infection and obviate the need for additional surgery to remove the implant30,31. PLGA is a synthetic, degradable polymer that exhibits favourable biocompatibility. Degradation of this polymer occurs through autocatalytic hydrolysis of the ester bond into oligomers of lactic acid and glycolic acid, which ultimately degrade through the Krebs cycle into CO2 and H2O32,33,34.
Previous studies have reported that drug transport across the blood-brain-barrier (BBB) by nanoparticles appears to be due to a receptor-mediated interaction with brain capillary endothelial cells that is facilitated through certain plasma apolipoproteins adsorbed by nanoparticles in the blood35,36. Nanoparticulate vectors are designed to interact with BBB-forming cells at a molecular level and, thus, can transport drugs or other molecules without interfering with the normal function of the brain33,34,35. Small fibres, particularly those with a size of nearly 100 nm, are therefore likely to be taken up by cells at rates 15 to 250 times faster than those of micron-sized fibres37. Biodegradable vancomycin-eluting PLGA nanofibres directly release vancomycin into the treatment area, thus yielding a high AUC/MIC ratio16. Because of its thinness (approximately 0.1 mm) and light weight, the nanofibrous membrane is ideally used in the mass-sensitive tissue of the CNS16,34. In addition, postoperative and posttraumatic infections increase the risk of wound adhesion. Adhesion between the brain and the scalp can be a source of neurological injury during subsequent exposure of the brain for further operation. Although the complete excision and debridement of postoperative and posttraumatic infections containing foreign bodies or contaminated tissue through craniectomy is required9,10,11,38, the craniectomy necessitates a second operation (cranioplasty) for replacing the bone38. Fibroblasts originating from the scalp muscle or carried by blood into the operative area cause strong adhesion of the tissue. Blocking or reducing the migration of fibroblasts from the musculature or haematoma may be the only means for reducing these adhesions and scar tissue formation. Biophysical barriers can be applied to prevent adhesion between the peridural fibrosis and the dura matter39. Physical barriers are the most widely accepted method for minimising adhesion formation40. Because of its nanoscale structure, the nanofibrous membrane developed in this study provides an additional benefit; it can prevent adhesion between the brain surface and the overlying scalp39,40. In addition, because the antibiotic concentration required for prophylactic use is much lower6,7,8, the vancomycin-loaded nanofibrous membrane can be used in prophylactic therapy after clean-contaminated and dirty surgery to prevent posttraumatic and postoperative CNS infection.
Previous animal models of brain infection (brain abscess) have had the disadvantages of requiring multiple surgical preparations, a stereotaxic headholder, the injection of foreign materials with bacteria and low success rates41,42,43. In addition, previous infection models (particularly those of brain abscesses) did not adequately represent the clinical situations of PCNSIs and posttraumatic central nervous system infections, including subcutaneous emphysema, epidural or subdural abscesses and brain abscesses). In our PCNSI model, commercial Duraform was soaked in a prepared bacterial solution and placed on the brain surface after a craniectomy. PCNSI was induced with a high success rate (near 100%). This PCNSI model is simple, represents the clinical situation and yields reproducible results. In addition, the serial MRI images, gross wound appearances and pathology examination results demonstrated that the postoperative CNS-infected rats treated with biodegradable vancomycin-eluting PLGA nanofibrous membrane recovered adequately. By contrast, most of the rats implanted with the virgin PLGA nanofibrous membrane died within 1 week and only two rats survived at the end of study. These results suggest that electrospun vancomycin-eluting PLGA nanofibres are favourable potentially sustainable drug-delivery vehicles for the treatment or prophylaxis of postoperative CNS infections, including brain abscesses, epidural abscesses and subdural empyema, after surgical debridement.
Methods
Preparation of PLGA and vancomycin nanofibres
The PLGA used in this study was a commercially available material (Resomer RG 503, Boehringer, Ingelheim, Germany) with a lactide:glycolid ratio of 50:50. The drug used was commercial grade vancomycin hydrochloride (Sigma-Aldrich, Saint Louis, MO, USA).
The drug-eluting nanofibrous membranes were prepared using an electrospinning process. The electrospinning setup consisted of an adjustable, high-DC-voltage power supply, a syringe pump and needle (internal diameter 0.42 mm), a ground electrode and an aluminium sheet. The needle was connected to the high-voltage supply, which generated positive DC voltage (up to 35 kV) and current (up to 4.16 mA/125 W). For nanofibre preparation, PLGA (1,250 mg) and vancomycin (250 mg) were first dissolved in 5 mL of 1,1,1,3,3,3-hexafluoro-2-propanol (Sigma-Aldrich, USA). The solution was then delivered and electrospun using a syringe pump at a volumetric flow rate of 1.8 mL/hour. The distance between the needle tip and the ground electrode was 12 cm and the positive voltage applied to the polymer solutions was 17 kV. All electrospinning experiments were conducted room temperature. The electrospun nanofibres were collected in membrane form on the aluminium sheet and the thickness of the membrane was measured to be 0.11 mm.
Bacteria
S. aureus was used as the pathogen. It is the most common etiologic agent in traumatic and iatrogenic abscesses and is a consistent pathogen1,9,10. The bacteria were grown overnight (20 hours) at 37°C in 12 mL of a culture broth (LB broth, GIBCO, Thermo Fisher Scientific, Inc., USA). Before the experiments, the culture was centrifuged at 3,000 g for 15 minutes and the supernatant was decanted. This stock solution was serially diluted by 10-fold and the number of bacteria present in the solutions was determined using the standard microbiological plating and counting technique. The final concentrations of viable organisms ranged from 2.4 to 5 × 107 colony-forming units (CFU)/μL.
Surgical procedure
All of the animal experiments were performed in accordance with relevant guidelines and regulations of the National Institute of Health of Taiwan. All animal-related procedures have been reviewed and approved by the Institutional Animal Care and Use Committee (IACUC) of Taipei Medical University (IACUC approval number: LAC-100-0163). Efforts were made to minimize the number of animals used and their suffering. Forty Wistar rats, each weighing 200–300 g, were anesthetized using an intraperitoneal injection of 6% chloral hydrate (0.6 mL/kg body weight). After shaving and sterilization of the incision area, a 1.5-cm scalp incision was made lateral to the midline between the ear and the eye. The temporalis muscle and periosteum were dissected using a scalpel and a small craniotomy (approximately 1 × 1 cm) was made using an electric burr (Figure 8a). Several commercially available Duraform dural grafts (Codman & Shurtleff, Inc., Raynham, USA) with a size of 1 × 1 cm were soaked in the prepared bacterial solution before implantation (Figure 8b). After local haemostasis, the soaked Duraform was implanted and covered by the postcraniectomy brain surface of the rats (Figure 8c). The skin was then closed in a single layer of 3-0 nylon. Four days later, the implanted Duraform was removed. The rats were randomly subdivided into two groups with 18 rats in each group. A virgin PLGA nanofibrous membrane (0.8 × 0.8 cm) was implanted and covered the brain surface of the rats in the vehicle-control group, whereas a vancomycin-eluting PLGA membrane (0.8 × 0.8 cm) was implanted in the rats in the vancomycin-nanofibres group (Figure 8d). The scalp wound was sutured with 3-0 nylon. After surgery, the rats were housed randomly, with three or four rats in a single cage. Any rats that experienced intraoperative brain injuries, died within the first postoperative day, or exhibited failure of PCNSI formation were excluded from the study.
Surgical procedure: a. Craniectomy (approximately 1 × 1cm) was performed using an electric burr. b. Duraform grafts with a size of 1 × 1 cm were soaked in the diluted S. aureus solution. c. Soaked Duraform was implanted into the surface of the rats' brains (covering the craniectomy area). d. The virgin or vancomycin-eluting PLGA nanofibrous membrane was implanted after the removal of the Duraform.
MRI and microscopic examinations
The gross wound appearances were observed daily and aerobic and anaerobic wound cultures were performed when discharge from the wounds was observed. All MRI scans were performed using a 7 Tesla Biospec MR imager (Bruker, Ettlingen, Germany). Before membrane implantation, T1- and T2-weighted images were obtained to ensure that the PCNSI models were successfully created (excluding epidural haemorrhage, subdural haemorrhage and intracerebral haemorrhage). T2-weighted images were obtained as a reference for identifying the PCNSI region at 1, 2, 4, 6 and 8 weeks after the implantation of the nanofibrous membrane. The PCNSI volume was defined as the volume of the subcutaneous abscess, epidural abscess, subdural emphysema and brain abscess. The PCNSI volume was reconstructed and calculated using the open-source, FDA-approved Digital Imaging and Communication in Medicine (DICOM) imaging software (OsiriX). At each time-point (1, 2, 4, 6 and 8 weeks) or when a rat died accidentally, a minimum of one rat in each group was sacrificed and its brain tissues were carefully removed for pathological examination. The brain tissue was fixed in 10% formalin and embedded in paraffin. Coronal sections 6 μm in thickness were prepared and stained with haematoxylin and eosin.
Statistical analysis
The Kaplan-Meier method was used to compare overall survival among rats in different groups. Data (PCNSI volumes) were collected from the samples and analysed using a paired sample t test (PCNSI volumes among time points in a single group) and one-way ANOVA (PCNSI volumes at the same time point between the vancomycin-nanofibres group and the vehicle-control group). Statistical analyses were performed using Stata SE, version 10.0 (Stata, College Station, TX). Data were expressed as the means ± standard deviation and the threshold for significance was a P value less than 0.05.
References
McClelland, S., 3rd & Hall, W. A. Postoperative central nervous system infection: incidence and associated factors in 2111 neurosurgical procedures. Clin. Infect. Dis. 45, 55–59 (2007).
Nathoo, N., Nadvi, S. S. & van Dellen, J. R. Cranial extradural empyema in the era of computed tomography: a review of 82 cases. Neurosurgery. 44, 748–753 (1999).
Korinek, A. M. Risk factors for neurosurgical site infections after craniotomy: a prospective multicenter study of 2944 patients. The French Study Group of Neurosurgical Infections, the SEHP and the C-CLIN Paris-Nord. Service Epidemiologie Hygiene et Prevention. Neurosurgery. 41, 1073–1079 (1997).
Blomstedt, G. C. Infections in neurosurgery: a retrospective study of 1143 patients and 1517 operations. Acta Neurochi. 78, 81–90 (1985).
McClelland, S., 3rd. Postoperative intracranial neurosurgery infection rates in North America versus Europe: a systematic analysis. Am. J. Infect. Control. 36, 570–573 (2008).
Korinek, A. M. et al. Risk factors for adult nosocomial meningitis after craniotomy: role of antibiotic prophylaxis. Neurosurgery. 59, 126–133 (2006).
Korinek, A. M. et al. Risk factors for neurosurgical site infections after craniotomy: a critical reappraisal of antibiotic prophylaxis on 4,578 patients. Br. J. Neurosurg. 19, 155–162 (2005).
Walcott, B. P., Redjal, N. & Coumans, J. V. Infection following operations on the central nervous system: deconstructing the myth of the sterile field. Neurosurg. Focu. 33, E8 (2012).
Cavusoglu, H., Kaya, R. A., Turkmenoglu, O. N., Colak, I. & Aydin, Y. Brain abscess: analysis of results in a series of 51 patients with a combined surgical and medical approach during an 11-year period. Neurosurg. Focu. 24, E9 (2008).
Mampalam, T. J. & Rosenblum, M. L. Trends in the management of bacterial brain abscesses: a review of 102 cases over 17 years. Neurosurger. 23, 451–458 (1988).
Liu, C. et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin. Infect. Dis. 52, e18–55 (2011).
Moorthy, R. K. & Rajshekhar, V. Management of brain abscess: an overview. Neurosurg. Focus. 24, E3 (2008).
Tunkel, A. R. et al. Practice guidelines for the management of bacterial meningitis. Clin. Infect. Dis. 39, 1267–1284 (2004).
Wang, Q. et al. Postoperatively administered vancomycin reaches therapeutic concentration in the cerebral spinal fluid of neurosurgical patients. Surg. Neurol. 69, 126–129 (2008).
ASHP therapeutic position statement on the preferential use of metronidazole for the treatment of Clostridium difficile-associated disease. Am. J. Health Syst. Pharm. 55, 1407–1411 (1998).
Tseng, Y. Y., Kao, Y. C., Liao, J. Y., Chen, W. A. & Liu, S. J. Biodegradable drug-eluting poly[lactic-co-glycol acid] nanofibers for the sustainable delivery of vancomycin to brain tissue: in vitro and in vivo studies. ACS Chem. Neurosci. 4, 1314–1321 (2013).
Yang, S. Y. Brain abscess: a review of 400 cases. J. Neurosurg. 55, 794–799 (1981).
Tseng, J. H. & Tseng, M. Y. Brain abscess in 142 patients: factors influencing outcome and mortality. Surg. Neurol. 65, 557–562 (2006).
Seydoux, C. & Francioli, P. Bacterial brain abscesses: factors influencing mortality and sequelae. Clin. Infect. Dis. 15, 394–401 (1992).
Rybak, M. J. et al. Therapeutic monitoring of vancomycin in adults summary of consensus recommendations from the American Society of Health-System Pharmacists, the Infectious Diseases Society of America and the Society of Infectious Diseases Pharmacists. Pharmacotherapy. 29, 1275–1279 (2009).
Patel, N. et al. Vancomycin: we can't get there from here. Clin. Infect. Dis. 52, 969–974 (2011).
Nicasio, A. M. et al. Evaluation of once-daily vancomycin against methicillin-resistant Staphylococcus aureus in a hollow-fiber infection model. Antimicrob. Agents Chemother. 56, 682–686 (2012).
Rybak, M. J. et al. Vancomycin therapeutic guidelines: a summary of consensus recommendations from the infectious diseases Society of America, the American Society of Health-System Pharmacists and the Society of Infectious Diseases Pharmacists. Clin. Infect. Dis. 49, 325–327 (2009).
Sakoulas, G. et al. Relationship of MIC and bactericidal activity to efficacy of vancomycin for treatment of methicillin-resistant Staphylococcus aureus bacteremia. J. Clin. Microbiol. 42, 2398–2402 (2004).
Shi, M. et al. Antibiotic-releasing porous polymethylmethacrylate constructs for osseous space maintenance and infection control. Biomaterials. 31, 4146–4156 (2010).
Lodise, T. P., Patel, N., Lomaestro, B. M., Rodvold, K. A. & Drusano, G. L. Relationship between initial vancomycin concentration-time profile and nephrotoxicity among hospitalized patients. Clin. Infect. Dis. 49, 507–514 (2009).
Liu, S. J., Wen-Neng Ueng, S., Lin, S. S. & Chan, E. C. In vivo release of vancomycin from biodegradable beads. J. Biomed. Mater. Res. 63, 807–813 (2002).
Le Ray, A. M. et al. Vancomycin encapsulation in biodegradable poly(epsilon-caprolactone) microparticles for bone implantation. Influence of the formulation process on size, drug loading, in vitro release and cytocompatibility. Biomaterials. 24, 443–449 (2003).
Xie, Z. et al. Treatment of osteomyelitis and repair of bone defect by degradable bioactive borate glass releasing vancomycin. J. Control. Release. 139, 118–126 (2009).
Kanellakopoulou, K. & Giamarellos-Bourboulis, E. J. Carrier systems for the local delivery of antibiotics in bone infections. Drugs. 59, 1223–1232 (2000).
El-Husseiny, M., Patel, S., MacFarlane, R. J. & Haddad, F. S. Biodegradable antibiotic delivery systems. J. Bone Joint Surg. 93, 151–157 (2011).
Beduneau, A., Saulnier, P. & Benoit, J. P. Active targeting of brain tumors using nanocarriers. Biomaterials. 28, 4947–4967 (2007).
Barbu, E., Molnar, E., Tsibouklis, J. & Gorecki, D. C. The potential for nanoparticle-based drug delivery to the brain: overcoming the blood-brain barrier. Expert Opin. Drug Deliv. 6, 553–565 (2009).
Tseng, Y. Y., Liao, J. Y., Chen, W. A., Kao, Y. C. & Liu, S. J. Sustainable release of carmustine from biodegradable poly[((D,L))-lactide-co-glycolide] nanofibrous membranes in the cerebral cavity: in vitro and in vivo studies. Expert Opin. Drug Deliv. 10, 879-888 (2013).
Kreuter, J. & Gelperina, S. Use of nanoparticles for cerebral cancer. Tumori. 94, 271–277 (2008).
Olivier, J. C. Drug transport to brain with targeted nanoparticles. NeuroRx. 2, 108–119 (2005).
Decuzzi, P., Pasqualini, R., Arap, W. & Ferrari, M. Intravascular delivery of particulate systems: does geometry really matter? Pharm. Res. 26, 235–243 (2009).
Stiver, S. I. Complications of decompressive craniectomy for traumatic brain injury. Neurosurg. Focus. 26, E7 (2009).
Kasimcan, M. O., Bakar, B., Aktas, S., Alhan, A. & Yilmaz, M. Effectiveness of the biophysical barriers on the peridural fibrosis of a postlaminectomy rat model: an experimental research. Injury. 42, 778–781 (2011).
Hu, C. et al. Long-term drug release from electrospun fibers for in vivo inflammation prevention in the prevention of peritendinous adhesions. Acta Biomater. 9, 7381–7388 (2013).
Wood, J. H., Doppman, J. L., Lightfoote, W. E., 2nd, Girton, M. & Ommaya, A. K. Role of vascular proliferation on angiographic appearance and encapsulation of experimental traumatic and metastatic brain abscesses. J. Neurosurg. 48, 264–273 (1978).
Long, W. D. & Meacham, W. F. Experimental method for producing brain abscesses in dogs with evaluation of the effect of dexamethasone and antibiotic therapy on the pathogenesis of intracerebral abscesses. Surg. Forum. 19, 437–438 (1968).
Winn, H. R., Mendes, M., Moore, P., Wheeler, C. & Rodeheaver, G. Production of experimental brain abscess in the rat. J. Neurosurg. 51, 685–690 (1979).
Acknowledgements
This work was supported in part by the National Science Council of Taiwan (Contract No. NSC102-2314-B-038-043) and Chang Gung Memorial Hospital (Contract No. CMRPD2C0131). We thank the staff at the 7T animal MRI Core Lab of Neurobiology and Cognitive Science Center, National Taiwan University for their technical and facility supports.
Author information
Authors and Affiliations
Contributions
S.J.L. and Y.Y.T. conceptualized the experiments, designed and directed the experiments and edited the manuscript. Y.Y.T. designed and performed the animal experiments and wrote the manuscript. Y.C.W. oversaw research activities and experiment and involved in processing nanofibrous membranes. C.H.S. carried our pharmacological evaluation and statistical analyses.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Tseng, YY., Wang, YC., Su, CH. et al. Biodegradable Vancomycin-eluting Poly[(d,l)-lactide-co-glycolide] Nanofibres for the Treatment of Postoperative Central Nervous System Infection. Sci Rep 5, 7849 (2015). https://doi.org/10.1038/srep07849
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep07849
This article is cited by
-
Nanoparticles and nanoformulated drugs as promising delivery system in treatment of microbial-induced CNS infection: a systematic review of literature
Journal of NeuroVirology (2021)
-
Theranostic 3-Dimensional nano brain-implant for prolonged and localized treatment of recurrent glioma
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.