Abstract
Surveillance guidelines for breast cancer survivors recommend regular history and physical and mammography and against routine imaging for detecting distant metastasis. Stage 0, I, II breast cancer cases treated at a major cancer center were identified from the Taiwan Cancer Registry. We used multivariable negative binomial and logistic regression analyses on institutional claims data to examine factors contributing to utilisation patterns of surveillance visits and tests in disease-free survivors. The mean number of surveillance visits during months 13 to 60 after cancer treatment initiation was 18.5 (SD 8.2) among the 2,090 breast cancer survivors followed for at least five years. After adjusting for patient and disease factors, the number of visits was the highest among patients mainly followed by medical oncologists compared to surgeons and radiation oncologists. Patient cohorts treated in more recent years had lower number of visits associated with care coordination effort, the adjusted mean being 19.2 visits for the 2002 cohort and 16.3 visits for the 2008 cohort (p < 0.0001). Although imaging tests were highly utilised, there was a significant decrease in tumor marker testing from the 2002 to the 2008 treatment cohort (adjusted rate 99.4% to 35.1% respectively, p < 0.0001) in association with an institutional guideline change.
Similar content being viewed by others
Introduction
The population of cancer survivors has been increasing rapidly, projected to reach 18 million in the United States by 20221. Breast cancer patients constitute a large proportion of this population due to its high incidence, early diagnosis and excellent prognosis2. Many oncologists continue to monitor their patients long after the risk of recurrence has diminished substantially. As a result, care for cancer survivors represents a significant portion of the oncology practice3. There is growing evidence for oncology workforce shortage in the coming years4,5,6. The quality of cancer care is predicted to be substantially affected by future workforce shortages such that cancer patients could experience delays in prompt diagnosis and treatment, longer wait times, less frequent interaction with clinical services, greater health disparities and decreased clinical trial enrollment. In the 2013 Institute of Medicine report “Delivering High-Quality Cancer Care”7, a key recommendation to ensure quantity and quality of the cancer care workforce is to have a coordinated cancer care team. For survivorship care, this means coordination among cancer specialists, primary care physicians and nurse specialists to ensure efficient, evidence-based and high quality care8,9,10. Many cancer survivors engage with multiple oncology specialists and primary care physicians for overlapping cancer recurrence surveillance, health promotion and preventive health care11,12,13. Clarifying the role of each clinician and coordinating the transition of care from oncology to primary care may help to better utilise the available oncology workforce.
Randomized controlled trials in breast cancer survivors have consistently shown the lack of mortality or quality of life benefit from intensive surveillance with testing for metastasis14,15,16. Surveillance guidelines recommend annual mammography aimed at detecting local recurrence or second breast cancer and do not recommend routine testing for distant metastasis in asymptomatic patients17,18,19,20. In practice, however, both underuse of mammography and overuse of non-recommended surveillance are frequent13,21,22,23,24,25,26,27,28,29. These studies demonstrate the substantial challenges in implementing evidence-based practice in cancer survivorship.
The incidence of breast cancer in Taiwan has risen more than 50% in the last decade30. We anticipate a similar rise in the population of breast cancer survivors in Taiwan. A single-payer fee-for-service National Health Insurance (NHI) was adopted in 1995 that provides accessible and affordable care31,32. However, as patients have unrestricted access to any specialty, primary care physicians are under-utilised and coordination among providers is poor. As in other countries with an aging population and rising cancer incidence, Taiwan is likely to see an exacerbation of the oncology workforce shortage and an escalating health care cost.
Koo Foundation Sun Yat-Sen Cancer Center (KF-SYSCC) has been one of the major cancer centers in Taiwan for over two decades, treating about 10% of all new breast cancer patients in 2009. It adopts a multidisciplinary approach to treatment planning and worked with NHI to pilot a bundled pay-for-performance reimbursement model for breast cancer33. For stage 0, I, II breast cancer patients (77% of all breast cancer patients) treated from 1990 to 2009, the five-year survival rate was between 91% and 98%. As the survivor population grew, there was a noticeable impact on the availability of oncologists to newly diagnosed patients. At the same time, rising volume of surveillance imaging tests for cancer survivors impacted access to these services for patients with active cancer.
This study sought to examine utilisation patterns of surveillance visits and tests in disease-free breast cancer survivors at this cancer center, where strategies to foster better care coordination and evidence-based practice in cancer survivors are being developed. We hypothesized that physician behavior varied significantly, but in time, care coordination and guideline implementation efforts would promote appropriate utilisation of services. We analyzed patient and physician factors influencing the frequency of outpatient visits and surveillance tests as well as temporal trend, hoping to gain insight in interventions for facilitating efficient and effective healthcare delivery.
Results
Description of the study sample
Of the 5,500 breast cancer patients treated between 2002 and 2009, 4,115 women were diagnosed with stage 0, I and II disease. To avoid including non-surveillance visits or tests, we excluded those with cancer recurrence (n = 366), second cancer (n = 436) and those who died (n = 86) from the final sample (Figure S1).
In our final cohort of 3,094 disease-free early stage breast cancer survivors, the mean age at diagnosis was 48.3 (standard deviation (SD) 10.4) and the median age was 47 (Table 1). This was somewhat younger than the median age of 52 in Taiwan (data in 2010)34 and much younger than the median age of 61 in the United States (data from 2006–2010)35. The majority of patients were free of comorbid conditions (76%) as expected from the age distribution. Among those with comorbid conditions, the most common were mild liver disease (9.7%) and diabetes mellitus (9.0%). Most patients kept their follow-up at the cancer center, with about two thirds (n = 2,090) followed for five years or more.
Physician visits for breast cancer survivors
The mean number of surveillance visits during months 13 to 60 after cancer treatment initiation was 18.5 (SD 8.2) among survivors followed for at least five years (Table 2). As expected, patients had more visits during earlier years following cancer treatment (mean 5.7 visits per patient per year in months 13–24) than in later years (mean 3.8 visits during months 49 to 60). Similarly, the proportion of the survivors seeing more than one specialty was 67% in months 13 to 24, decreasing to 33% in months 61 to 72 (Table S1). Comparing different treatment year cohorts across each post-treatment surveillance year, we found that 2008 and 2009 were the years when number of visits decreased substantially across all cohorts (numbers in bold, Table 2), which coincided with implementation of a care coordination program for breast cancer survivors at the cancer center.
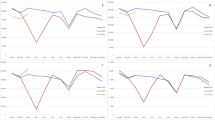
In multivariate analysis, after adjusting for patient and disease factors, we observed an overall downward trend in the number of visits from patients treated in 2002 (adjusted mean 19.2 visits) to patients treated in 2008 (16.3 visits) (p < 0.0001, Figure 1a). The number of visits also differed significantly among different main surveillance physicians, ranging from 16.7 to 22.2 visits (p < 0.0001, Figure 1b). Patients followed mainly by medical oncologists on average had the highest number of visits (21.3), compared to those by general surgeons (17.9) or radiation oncologists (18.6). The factors influencing the number of surveillance visits in months 13 to 60 are summarized in Table 3. Being older or living farther from Taipei was associated with lower number of visits. Survivors who had seen a psychiatrist and those with higher comorbidity scores had more breast cancer visits. Among cancer-related factors, higher cancer stage, having received chemotherapy and receiving hormonal therapy were each associated with greater number of visits. In particular, patients on hormonal therapy had substantially more visits than patients not on it (21.0 vs. 14.0 visits).
Adjusted mean number of surveillance visits during post-treatment months 13 to 60 in breast cancer survivors (a) treated in year 2002 to 2008 and (b) followed by different main surveillance physician or specialty; GS: general surgeon, MO: medical oncologist, RO: radiation oncologist.
The point estimate for the number of visits was the predicted margin after adjusting for patient and disease factors in a negative binomial regression model. The error bars represent 95% confidence intervals.
Surveillance testing for breast cancer recurrence
Among patients who were followed for at least five years, 89% received at least one mammography by the end of year 2 and 68% received annual mammography before the end of year 5 (Table 4). Nearly all patients received breast ultrasound, liver ultrasound and chest X-ray. In multivariate analysis, more outpatient visits was associated with higher odds of testing for annual mammography, annual breast ultrasound, tumor markers, bone scan and CT/MRI/PET-CT (Table 5). In terms of temporal trends, the most significant change was a decrease in tumor marker testing from the 2002 cohort (adjusted testing rate 99.4%) to the 2008 cohort (35.1%) (Figure 2) reflecting a change in the institutional guideline in 2006. We also noted a decreasing trend in the use of mammography, with a concurrent increase in the utilisation of annual breast ultrasound.
Rates of surveillance testing in breast cancer survivors treated in year 2002 to 2008.
Rates for chest X-ray and liver ultrasound were nearly 100% across all years and for all categories of covariates, thus were not adjusted. For all other tests, rates were adjusted for patient, disease, physician and frequency of visit variables using multiple logistic regression. CXR: chest X-ray; CT: computed tomography; MRI: magnetic resonance imaging; PET: positron emission tomography; mammo: mammography.
Physician specialties differed significantly in surveillance testing by analyses both at the patient level (Table 5) and at the visit level (Figure 3). Patients mainly followed by general surgeons had the highest odds of receiving annual mammography and breast ultrasound, while those mainly followed by medical oncologists had the highest testing odds for tumor markers, bone scan and abdominal CT/MRI or PET-CT. Within each specialty there was also significant variation among physicians (Table 5). When analyzing the probability of ordering specific tests during a surveillance visit, we found that general surgeons were the most likely to order mammograms and medical oncologists were the most likely to order tumor markers and bone scans (Figure 3), consistent with results obtained at the patient level. Non-oncology internists were less likely to order any of the surveillance tests.
Adjusted probability of testing in a breast cancer surveillance visit by physician specialty.
Types of tests are indicated on the horizontal axis. Each bar represents a physician specialty: general surgery (blue), medical oncology (red), radiation oncology (green) and non-oncology medicine (purple). The percentages were predicted probabilities of each test (as a dichotomous outcome in an outpatient visit) after adjusting for patient and disease factors and year of treatment, using repeated-measures logistic regression with generalized estimation equation. P-values were obtained for each surveillance test among four specialties using the likelihood ratio test.
Discussion
This study examined the utilisation pattern of physician visits and surveillance testing in breast cancer survivors at a major cancer center in Taiwan under the single-payer fee-for-service national health insurance and identified areas of health care delivery that were not always concordant with guideline-based care. We found a high volume of physician visits, averaging about 6 visits during year 2 and about 4 yearly visits during the subsequent years 3 to 5. These were higher than the American Society of Clinical Oncology (ASCO) guideline recommendation of history and physical exam every 3 to 6 months for the first 3 years and every 6 to 12 months for years 4 and 517. We observed a significant reduction in the number of visits by about 1 visit per surveillance year, occurring in the years 2008 and 2009, associated with implementation of a clinic for breast cancer survivors staffed by nurse specialists and primary care physicians and the expansion of services to mail test reports and arrange further work-up through telephone. It is likely that this program reduced unnecessary visits.
There was statistically significant between-specialty and between-physician variation in the frequency of visits. Among different physicians, the mean ranged from 16.7 to 22.2 visits in the 4-year surveillance period. Overall, patients followed mainly by medical oncologists had the highest number of visits compared to surgeons and radiation oncologists, even after adjusting for patient differences and disease severity. This could be an area for targeted intervention as follow up by multiple specialties could be consolidated. Oncologists should be encouraged to transfer survivorship care to primary care providers and physician extenders with appropriate treatment summary or survivorship care plan, especially in patients at low risk for recurrence7,17.
Hormonal therapy was associated with significantly more visits. The Taiwan NHI requires patients on any chronic medication be seen by a physician at least every 3 months, which likely affected the excess number of visits among those patients. Policy change to extend the mandatory visit interval could alleviate some burden on the health care system.
International guidelines recommend annual mammography. In this study population, we found adherence to annual mammography during surveillance at only 68% and there was a downward trend from the 2002 to the 2008 treatment cohorts with a concurrent increase in breast ultrasound use. There is a widely held belief that mammography is less sensitive in Asian women and in the younger breast cancer population due to dense breast tissue, with ultrasound considered more effective in this setting. However, there has been no high quality study to support the role of surveillance breast ultrasound in breast cancer survivors. Evidence-based guidelines in the local setting should be developed to implement practices concordant with international guidelines.
The substantial influence of local guidelines was evident in the large decline in rates of tumor marker testing from 2002 (99.4%) to 2008 (35.1%), consistent with an institutional guideline agreed upon by the breast cancer multidisciplinary team in 2006 to stop routine testing. On the other hand, nearly all patients continued to receive liver ultrasound and chest X-rays across the surveillance period consistent with the recommendations by the institutional guideline. These tests to detect asymptomatic metastasis have not been supported by evidence and have not been recommended in the ASCO guidelines since 199617,36,37,38. Despite existing guidelines from ASCO and other international organizations, testing is common even in the United States and Canada21,22,27. There are tremendous challenges to implementing evidence-based surveillance practice including anxiety about recurrence from both cancer survivors and their care providers, competing hospitals or providers who use those tests for surveillance, concerns for litigation and some physicians' belief that the newer drugs for breast cancer might give longer or better survival if recurrences were found sooner39. Previous studies identified a wide variety of physician-level barriers to guideline adherence ranging from physician knowledge (lack of awareness or familiarity), attitudes (lack of agreement, self-efficacy, outcome expectancy and the inertia of previous practice), to behavior (external barriers from patients, guideline and environment)40. It is crucial to understand key local barriers in order to design practice-changing interventions with more potential for effectiveness.
Our study has several limitations. Because the utilisation was evaluated on a population that was treated and followed at a single-institution, we could not address the extent of under- or over-utilisation contributed by providers outside of the institution. Patients without a usual place for follow-up may not get recommended surveillance, while others may get duplicate care from multiple health care providers. The next step in this research would be to examine these relationships in nationwide utilisation data in breast cancer survivors. Second, we assigned a main physician (or specialty) based on the highest frequency of visits. The outcome may not be completely representative for the assigned physician but influenced by the number of specialties patients see. We did sensitivity analysis by including in the regression model the number of specialties seen and the main conclusions about physician visits remained unchanged. Finally, to ascertain the nature of visits or tests being surveillance rather than diagnostic, ICD-9 codes alone may not be adequate. Although we limited the study population to early stage breast cancer patients without known cancer recurrence, second cancer or death and included only visits or tests with the primary diagnosis code of breast cancer, it was still possible that a small number of the tests were done for diagnostic purposes.
To our knowledge, this is the first health care utilisation study in a large sample of breast cancer survivors in Asia. Using reliable and relatively complete datasets from a single institution allowed in-depth analysis of factors affecting the intensity of surveillance. This large patient cohort spanned eight years; temporal trends and physician variations were observed suggesting the important roles of care coordination and local guidelines. The medical and surgical oncology subspecialties have only been established in Taiwan since the early 1990's, thus practice standards have not been fully developed. We expect an even greater practice variation across hospitals and regions in Taiwan.
In summary, there was high utilisation of physician visits and surveillance tests in breast cancer survivors at a cancer center in Taiwan. In patient cohorts treated from 2002 to 2008, the number of visits and tumor marker testing decreased significantly, likely associated with better care coordination and changes in institutional guidelines. There were significant between-physician and between-specialty variations in utilisation. The concerns for overutilisation of health care resources and physician adherence to guidelines are universal in developed countries. The results from this study provide a strong foundation for quality improvement in care delivery to breast cancer survivors.
Methods
Data sources and study population
We identified female breast cancer patients of stage 0, I and II from the Taiwan Cancer Registry who were treated at KF-SYSCC between 2002 and 2009. To avoid including non-surveillance visits or tests, we excluded patients with any breast cancer recurrence (locoregional or metastatic), second malignancy and those who died before the end of the study period (October 31, 2013).
Patient characteristics and information on cancer and treatment modalities were extracted from the cancer registry and the electronic health records. Physician visits, laboratory and imaging tests were extracted from the insurance claims database. The length of follow-up was from the start of the cancer treatment date to the date of their last visit to the cancer center as of October 31, 2013.
Physician visits
We defined the surveillance period conservatively as starting from 1 year after the treatment initiation date to ensure cancer treatment had been completed. We analyzed visits in a 4-year surveillance interval from month 13 to 60, as well as in yearly intervals during months 13 to 24, 25 to 36, 37 to 48, 49 to 60 and 61 to 72. For each surveillance interval, only patients followed through the end of the interval were included in the analysis. Since all patients were disease free, visits with the primary International Classification of Diseases 9th revision (ICD-9) codes of 174 and 233 were identified as breast cancer surveillance visits for inclusion in our analyses41. For each eligible visit we extracted patient identification (ID) number, date of service, provider number, provider specialty, up to five ICD-9 codes and a link number to match with tests ordered through the visit.
Surveillance imaging and serum tumor marker tests
We defined surveillance tests as the following tests ordered through the breast cancer surveillance visits: mammography, breast ultrasound, liver ultrasound, chest X-ray, bone scan, tumor markers (CEA and CA15-3), abdominal computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography-CT (PET-CT). For mammography and breast ultrasound, we included tests performed after six months from cancer treatment initiation. For all other tests, we included ones after one year from treatment initiation to avoid counting tests performed during cancer treatment.
Predictor variables
Patient characteristics as covariates included age at diagnosis, education, marital status, residential area within the country, Charlson comorbidity score and whether the patient had seen psychiatry during surveillance as a proxy for presence of psychiatric conditions such as anxiety or depression. Charlson score42,43,44 was calculated using ICD-9 codes from all available inpatient and outpatient claims data and then grouped into 0, 1 and 2 or above.
Breast cancer characteristics variables included stage at diagnosis (0, I, II) and treatment received (chemotherapy, radiotherapy, and/or hormonal therapy). We also included the year of treatment to analyze temporal trends in utilisation of health services. Cohorts treated in year 2002 to 2008 were analyzed, where five years of follow-up data was available. We excluded surgery type and tumor receptor status in the regression analysis due to incomplete data for these variables and concerns about multicollinearity. As would be expected, surgery type was highly correlated with radiotherapy (Pearson r = 0.63) and tumor receptor status with hormonal therapy (Pearson r = 0.84).
For each patient, we assigned a main surveillance physician based on the physician providing the highest number of breast cancer visits to that patient during the surveillance interval. Similarly, a main surveillance specialty (general surgery, medical oncology, or radiation oncology) was assigned based on the specialty that provided the highest number of breast cancer visits to a given patient. A small number of patients who had no surveillance visits (thus no physician) at the cancer center (n = 133) were therefore excluded from analysis.
Statistical Analysis
We used descriptive statistics to characterize the study population and calculated the mean number of physician visits during each surveillance interval and for each categorical level of the predictor variables. We used simple linear regression with the year of treatment as a continuous variable to examine linear trend in the number of visits in each surveillance interval.
We performed multivariable analyses on physician visits during the 4-year surveillance period of months 13 to 60 with patients as the units of analysis. Subjects with missing values in any variable (6.5% of sample) were dropped from the analysis. To analyze factors affecting the number of visits, we used negative binomial regression with the robust variance estimator45. A Poisson model was first fitted but there was significant overdispersion. The negative binomial model gave a better fit shown by likelihood ratio test. The effects of the main surveillance physician and of the main surveillance specialty were analyzed separately since the two variables were correlated (Pearson r = 0.67). Following negative binomial regression we obtained post-estimation adjusted mean visits (predicted margins)46 for each predictor category.
For surveillance tests, we calculated the proportions of patients receiving each of the tests during surveillance months 13 to 60. We then used multiple logistic regression to identify factors associated with the probability of a patient receiving the test. The outcomes included annual mammography, annual breast ultrasound, tumor markers, bone scan and combined abdominal CT or MRI or PET-CT. The number of physician visits was categorized into tertiles and included as a predictor in these analyses. We calculated adjusted odds ratios with confidence intervals for significant predictors of each outcome and obtained predicted testing probabilities for each treatment year cohort and each physician. A separate analysis was done to examine the probability of ordering a test by each specialty using visits as the units of analysis. Adjusted testing probabilities by specialty were calculated using repeated-measures logistic regression with generalized estimation equation (GEE)47.
All tests of statistical significance were two-sided using an alpha value of 0.05. Analyses were carried out using SAS 9.4 (SAS institute Inc., Cary, NC) or Stata 13 (StataCorp, College Station, TX). The study protocol was approved by the Institutional Review Board of KF-SYSCC and the methods were carried out in accordance with the approved guidelines and regulations.
References
de Moor, J. S. et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev 22, 561–570, 10.1158/1055-9965.epi-12-1356 (2013).
Berry, D. A. et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 353, 1784–1792, 10.1056/NEJMoa050518 (2005).
AAMC (Association of American Medical Colleges), Forcasting the supply of and demand for oncologists: A report to the American Society of Clinical Oncology from the AAMC Center for Workforce Studies. (2007) Available at: https://www.asco.org/sites/default/files/oncology_workforce_report_final.pdf. (Accessed: February 5, 2014).
Erikson, C., Salsberg, E., Forte, G., Bruinooge, S. & Goldstein, M. Future supply and demand for oncologists: challenges to assuring access to oncology services. J Oncol Pract 3, 79–86, 10.1200/jop.0723601 (2007).
Etzioni, D. A., Liu, J. H., Maggard, M. A., O'Connell, J. B. & Ko, C. Y. Workload projections for surgical oncology: will we need more surgeons? Ann Surg Oncol 10, 1112–1117 (2003).
Wallace, A. H. et al. Projecting the need for gynecologic oncologists for the next 40 years. Obstet Gynecol 116, 1366–1372, 10.1097/AOG.0b013e3181fc3a22 (2010).
Institute of Medicine. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis (Washington, D.C. The National Academy Press, 2013).
Grunfeld, E. et al. Randomized trial of long-term follow-up for early-stage breast cancer: a comparison of family physician versus specialist care. J Clin Oncol 24, 848–855, 10.1200/JCO.2005.03.2235 (2006).
Oeffinger, K. C. & McCabe, M. S. Models for delivering survivorship care. J Clin Oncol 24, 5117–5124, 10.1200/JCO.2006.07.0474 (2006).
Howell, D. et al. Models of care for post-treatment follow-up of adult cancer survivors: a systematic review and quality appraisal of the evidence. J Cancer Surviv 6, 359–371, 10.1007/s11764-012-0232-z (2012).
Earle, C. C. & Neville, B. A. Under use of necessary care among cancer survivors. Cancer 101, 1712–1719, 10.1002/cncr.20560 (2004).
Snyder, C. F. et al. Preventive care in prostate cancer patients: following diagnosis and for five-year survivors. J Cancer Surviv 5, 283–291, 10.1007/s11764-011-0181-y (2011).
Snyder, C. F. et al. Comparing care for breast cancer survivors to non-cancer controls: a five-year longitudinal study. J Gen Intern Med 24, 469–474, 10.1007/s11606-009-0903-2 (2009).
Palli, D. et al. Intensive vs clinical follow-up after treatment of primary breast cancer: 10-year update of a randomized trial. National Research Council Project on Breast Cancer Follow-up. JAMA 281, 1586 (1999).
Rosselli Del Turco, M. et al. Intensive diagnostic follow-up after treatment of primary breast cancer. A randomized trial. National Research Council Project on Breast Cancer follow-up. JAMA 271, 1593–1597 (1994).
The GIVIO investigators. Impact of follow-up testing on survival and health-related quality of life in breast cancer patients. A multicenter randomized controlled trial. The GIVIO Investigators. JAMA 271, 1587–1592 (1994).
Khatcheressian, J. L. et al. Breast cancer follow-up and management after primary treatment: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 31, 961–965, 10.1200/jco.2012.45.9859 (2013).
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Breast Cancer (2014) Available at: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#breast. (Accessed: February 5, 2014).
Senkus, E. et al. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 24 Suppl 6, vi7–23, 10.1093/annonc/mdt284 (2013).
NICE (National Institute for Health and Care Excellence) Clinical Guidelines. Early and locally advanced breast cancer: Diagnosis and treatment (2009) Available at: http://publications.nice.org.uk/early-and-locally-advanced-breast-cancer-cg80/guidance#follow-up. (Accessed: February 5, 2014).
Hahn, E. E., Hays, R. D., Kahn, K. L., Litwin, M. S. & Ganz, P. A. Use of imaging and biomarker tests for posttreatment care of early-stage breast cancer survivors. Cancer 119, 4316–4324, 10.1002/cncr.28363 (2013).
Keating, N. L., Landrum, M. B., Guadagnoli, E., Winer, E. P. & Ayanian, J. Z. Surveillance testing among survivors of early-stage breast cancer. J Clin Oncol 25, 1074–1081, 10.1200/JCO.2006.08.6876 (2007).
Keating, N. L., Landrum, M. B., Guadagnoli, E., Winer, E. P. & Ayanian, J. Z. Factors related to underuse of surveillance mammography among breast cancer survivors. J Clin Oncol 24, 85–94, 10.1200/JCO.2005.02.4174 (2006).
Snyder, C. F. et al. Prevention, screening and surveillance care for breast cancer survivors compared with controls: changes from 1998 to 2002. J Clin Oncol 27, 1054–1061, 10.1200/JCO.2008.18.0950 (2009).
Field, T. S. et al. Under utilization of surveillance mammography among older breast cancer survivors. J Gen Intern Med 23, 158–163, 10.1007/s11606-007-0471-2 (2008).
Wirtz, H. S. et al. Factors associated with long-term adherence to annual surveillance mammography among breast cancer survivors. Breast Cancer Res Treat 143, 541–550, 10.1007/s10549-013-2816-3 (2014).
Grunfeld, E., Hodgson, D. C., Del Giudice, M. E. & Moineddin, R. Population-based longitudinal study of follow-up care for breast cancer survivors. J Oncol Pract 6, 174–181, 10.1200/jop.200009 (2010).
Mandelblatt, J. S. et al. Patterns of care in early-stage breast cancer survivors in the first year after cessation of active treatment. J Clin Oncol 24, 77–84, 10.1200/JCO.2005.02.2681 (2006).
Treanor, C. & Donnelly, M. An international review of the patterns and determinants of health service utilisation by adult cancer survivors. BMC Health Serv Res 12, 316, 10.1186/1472-6963-12-316 [doi] (2012).
Taiwan Cancer Registry (2009) Available at: http://tcr.cph.ntu.edu.tw/main.php?Page=A5B2. (Accessed: April 3, 2014).
Chiang, T. L. Taiwan's 1995 health care reform. Health Policy 39, 225–239 (1997).
Ho Chan, W. S. Taiwan's healthcare report 2010. EPMA J 1, 563–585, 10.1007/s13167-010-0056-8 (2010).
Porter, M. E., Baron, J. F. & Wang, C. J. Koo Foundation Sun Yat-Sen Cancer Center: Breast Cancer Care in Taiwan. Harvard Business School Case 710-425 (2009).
Bureau of Health Promotion. Taiwan Cancer Registry Annual Report 2010 (2013) Available at: http://www.hpa.gov.tw/BHPNet/Portal/File/StatisticsFile/201305061037065219/99%E5%B9%B4%E7%99%8C%E7%97%87%E7%99%BB%E8%A8%98%E5%A0%B1%E5%91%8A.pdf. (Accessed: August 18, 2013).
Surveillance, Epidemiology & and End Results Program, SEER Stat Fact Sheets: Breast Cancer. (2013) Available at: http://seer.cancer.gov/statfacts/html/breast.html. (Accessed: April 3, 2014).
Recommended breast cancer surveillance guidelines. American Society of Clinical Oncology. J Clin Oncol 15, 2149–2156 (1997).
Khatcheressian, J. L. et al. American Society of Clinical Oncology 2006 update of the breast cancer follow-up and management guidelines in the adjuvant setting. J Clin Oncol 24, 5091–5097, 10.1200/jco.2006.08.8575 (2006).
Smith, T. J. et al. American Society of Clinical Oncology 1998 update of recommended breast cancer surveillance guidelines. J Clin Oncol 17, 1080–1082 (1999).
Smith, T. J. Breast cancer surveillance guidelines. J Oncol Pract 9, 65–67, 10.1200/JOP.2012.000787 (2013).
Cabana, M. D. et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA 282, 1458–1465 (1999).
Cooper, G. S. et al. Use of guideline recommended follow-up care in cancer survivors: routine or diagnostic indications? Med Care 44, 590–594, 10.1097/01.mlr.0000215902.50543.77 (2006).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40, 373–383 (1987).
Deyo, R. A., Cherkin, D. C. & Ciol, M. A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45, 613–619 (1992).
Romano, P. S., Roos, L. L. & Jollis, J. G. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol 46, 1075–1079, discussion 1081–1090 (1993).
Cameron, A. C. & Trivedi, P. K. Microeconometrics Using Stata. (College Station, TX, Stata Press, 2009).
Williams, R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. The Stata Journal 12, 308–331 (2012).
Zeger, S. L. & Liang, K. Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics 42, 121–130 (1986).
Acknowledgements
We thank Catherine Crespi, PhD, for review of the statistical methods used in the study. Dr. Patricia Ganz was supported in part by the Conquer Cancer Foundation ASCO Professorship in Breast Cancer Comparative Effectiveness Research. Dr. Yong A. Wang was supported in part by an institutional grant from Koo Foundation Sun Yat-Sen Cancer Center.
Author information
Authors and Affiliations
Contributions
Y.A.W. and P.A.G. conceptualized the research project, wrote and revised the manuscript. A.C.F. contributed in data preparation, statistical analyses and discussion of results. Y.A.W. was in charge of data extraction, statistical analyses, project execution, manuscript preparation and writing. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplemental Info
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Wang, Y., Feng, AC. & Ganz, P. Health Services Utilisation in Breast Cancer Survivors in Taiwan. Sci Rep 4, 7466 (2014). https://doi.org/10.1038/srep07466
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep07466
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.