Abstract
We performed a meta-analysis to evaluate the therapeutic effects of radiofrequency ablation (RFA) and surgical hepatic resection (HR) in the treatment of small hepatocellular carcinoma (HCC). Thirty-one studies were included in the analysis. A total of 16,103 patients were involved: 8,252 treated with RFA and 7,851 with HR. Compared to the RFA group, the 3, 5-year overall and disease-free survival rates in the HR group were significantly higher. On the other hand, complications were significantly fewer and hospital-stay was significantly shorter in the RFA group than in the HR group. In subgroup analyses, the overall and disease-free survival in the HR group were also significantly higher than those in the RFA group for HCCs ≤ 3 cm, whereas there were no significant differences between the two groups for HCCs ≤ 2 cm. Our analysis showed that although HR was associated with higher complication rate and longer hospital-stay, HR is proposed as the first-line treatment rather than RFA for patients with HCCs larger than 2 cm. For patients with HCCs of 2 cm or less, RFA may be an alternative to HR because of their comparable long-term efficacy.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common malignant tumor and the second leading cause of cancer-related deaths worldwide1. Hepatic resection (HR) represents the most common first-line therapy for patients with HCC; however, the majority of primary liver cancers are not suitable for curative resection at the time of diagnosis2. Factors precluding surgery include extrahepatic metastases, vascular invasion, high-risk anatomical location, excessive size or number of lesions, insufficient remnant liver to support life and co-morbid conditions3. Therefore, several nonsurgical alternative techniques have been developed, such as acetic acid injection, percutaneous ethanol injection (PEI), radiofrequency ablation (RFA) and microwave ablation (MWA). Among these, RFA has been the most widely investigated therapeutic option for unresectable HCCs. Numerous large series have shown that RFA is safe, with minimal morbidity and mortality4. General consensus guidelines from North America and Japan recommend that RFA be used for three or fewer HCCs with a diameter of 3 cm at most5.
Nowadays, RFA has been commonly used as an alternative for patients with small HCCs who are not suitable for HR. However, whether it can compete with surgery as the first-line treatment still remains highly controversial. The results from published studies that examined the efficacy of RFA and HR for small HCC have been inconsistent. Huang et al.6 and Yun et al.7 reported that HR were more favorable regardless of tumor size. Elsewhere, Chen et al.8 and Feng et al.9 concluded that RFA was as effective as HR in the treatment of small HCCs. Additionally, Nashikawa et al.10 and Peng et al.11 recommended RFA as the first-line treatment for small HCCs.
Meta-analysis is a useful tool for revealing trends that might not be apparent in a single study. Pooling of independent but similar studies increases precision and therefore increases the confidence level of the findings12. The aim of this study is to evaluate the evidence from previous studies that directly compare the efficacy of RFA and HR in the treatment of small HCCs by summarizing it quantitatively with a meta-analysis approach.
Results
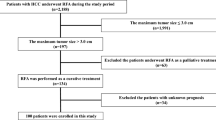
Literature Search
A flow diagram of our literature search was shown in Figure 1. Total searches yielded 1210 entries. After screening based on titles and abstracts, 72 articles appeared to be potentially relevant. Meta-analysis (14 articles) and systematical reviews (6 articles) were then excluded. Among the remaining 52 studies, 21 were eliminated after the full text analysis for the following reason: overlapping data or duplicated reports from the same study population (8 studies), lack of critical data (7 studies) and matching one of the exclusion criteria (6 studies). In the end, a total of 31 studies were selected, including three randomized controlled trials (RCTs) and 28 nonrandomized controlled trials (NRCTs)6,7,8,9,10,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38.
Study Characteristics
The baseline characteristics of included studies are summarized in Table 1. The 31 studies were published between 2004 and 2013 and involved a total of 16,103 patients. 8,252 patients were treated with RFA as the initial treatment and 7,851 patients who were treated with HR. Of these 31 studies, 15 were conducted in China, 6 in Italy, 5 in Japan, 3 in South Korea, 1 in United Kingdom and 1 in United States of America. The mean of age ranged from 41.5 to 68.4 years. The male: female ratio in the pooled data was 2.2:1.
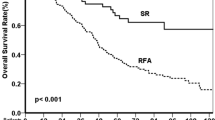
Overall Survival Rate
Overall survival rates at 3- and 5-year in the RFA group were 78.6% and 60.8% respectively. The corresponding rates for the HR group were 83.9% and 71.4% (Table 2). The difference was significant and favorable to HR group at 3-year (31 trials, odds ratio (OR): 0.65, 95% confidence intervals (95% CI): 0.53–0.80, Figure 2A) and at 5-year (20 trials, OR: 0.57, 95% CI: 0.48–0.67, Figure 2B).
Disease-free Survival Rate
Disease-free survival rates at 3- and 5-year were 41.1% and 26.6% respectively in the RFA group, 56.7% and 37.8% in the HR group (Table 2). Disease-free survival rates were significantly higher in the HR group for 3-year (27 trials, OR: 0.50, 95% CI: 0.41–0.61, Figure 3A) and 5-year (20 trials, OR: 0.47, 95% CI: 0.35–0.65, Figure 3B).
Complications and Hospital-Stay
The complication rate was 9.3% for RFA group and 30.1% for HR group (Table 2). Complications were significantly fewer in the RFA group than in the HR group (16 trials, OR: 0.25, 95% CI: 0.17–0.37, Figure 4A). The mean length of hospital-stay was 12.6 days for HR group and 6.8 days for RFA. The HR group had significant longer hospital-stay than RFA group (8 trials, weighted mean difference (WMD):5.83, 95% CI: 4.01–7.66, Figure 4B).
Subgroup Analysis
For tumors smaller than 3 cm, the data presented in Table 2 showed that the difference was significant and favorable to HR group at 3-year (19 trials, OR: 0.62, 95% CI: 0.43–0.89) and at 5-year (16 trials, OR: 0.55, 95% CI: 0.42–0.72). Disease-free survival rates were significantly higher in the HR group for 3-year (17 trials, OR: 0.52, 95% CI: 0.39–0.70) and 5-year (15 trials, OR: 0.57, 95% CI: 0.38–0.87).
In the case of very small tumors (<2 cm), overall survival rates at 3- and 5-year in the RFA group were 80.6% and 69.0% respectively. The corresponding rates for the HR group were 83.7% and 74.2%; disease-free survival rates at 3- and 5-year were 52.4% and 42.5% respectively in the RFA group, 53.7% and 41.6% in the HR group. In terms of overall survival and disease-free survival, there were no significant differences between these two groups.
Sensitivity Analysis and Publication Bias
The results suggested that the influence of each individual data set to the pooled ORs and WMD was not significant. The Egger's test showed no evidence of publication bias for the majority of comparison (Table 2).
Discussion
The choice between RFA and HR for small HCC is still a matter of debate. The results from previous studies that examined the efficacy of RFA and HR in the treatment of small HCC have been inconsistent. The current meta-analysis summarizes the results of 31 studies, with a total of 16,103 patients: 8,252 treated with RFA and 7,851 with HR. Our results showed that HR was associated with better overall and disease-free survival compared with RFA in the treatment of patients with small HCCs.
The main reason for the inferiority of RFA to HR in terms of the survival rates is thought to be its higher local recurrence rate. This could be due to insufficient ablation of the primary tumor, heat sink effect and the limitations of imaging modalities39. Additionally, HR usually removed a relatively suitable margin of the rim of normal liver tissue with the primary tumor and eliminated both the tumor and cancer embolus40. Hence, the relatively complete clearance of targeted tumors and potential tissues of microscopic lesions by surgical resection may explain the superior prognosis of HR for patients with small HCCs.
It had been reported that the beneficial effect of HR was more prominent in patients with HCC of more than 2 cm, because HCC of more than 2 cm had a higher incidence of vascular invasion than HCC of 2 cm or less41. In subgroup analysis, our results showed that for very early-stage HCC (size ≤ 2 cm), there were no significant differences between RFA and HR in terms of overall and disease-free survival. However, the findings need to be carefully interpreted, owing to the fact that this subgroup of patients are likely to have early disease presentation and good tumour biology. Hence, overall satisfactory outcomes can be achieved irrespective of the type of treatment. Although there was no statistically significant difference in terms of disease-free and overall survival, it seems reasonable to offer HR to patients with tumours less than 2 cm if appropriate and RFA as an alternative treatment if resection is not suitable.
On the other hand, our study suggested that RFA was associated with less complications and shorter hospital-stay compared with HR. In clinical practice, RFA can be performed without general anesthesia. Most patients undergoing percutaneous RFA only require 2–3 days' stay42. Therefore, RFA has a considerable advantage over HR in providing a better short-term postoperative result.
Previous meta-analysis studies had compared the efficacy of RFA versus HR in treating small HCCs, but the results remain inconsistent. Zhou et al. found that HR was superior to RFA in the treatment of HCC patients, particularly for tumors > 3 cm; for tumors ≤ 3 cm HR did not differ significantly from RFA for survival43. However, Xu et al. showed that HR was associated with significantly improved survival benefits compared with RFA for HCC ≤ 3 cm44. Cucchetti et al. recently conducted a systematical review and recommended to offer RFA to very small HCCs (<2 cm), since in this instance complete necrosis is most likely to be achieved. For larger tumors, namely > 2 cm and especially if >3 cm, surgical removal is to be preferred5. These results are consistent with our findings. In addition, we considered the current meta-analysis had following improvements: 1) the number of total studies were substantial. Especially, eight recent studies published since 2012 were included, which significantly increased the statistical power of the analysis; 2) we extended our literature search to non-English language journals and identified additional seven studies published in Chinese and Korean that were not captured by previous reviews; 3) more than 16,000 patients from six different countries were included to yield results that are broader in scope and richer in meaning.
Despite these advantages, some limitations of the current meta-analysis should be acknowledged. The literature review retrieved 31 eligible studies; of them, three RCTs were available whereas the remaining 28 studies were represented by retrospective observational studies. Except for RCTs, there are few “head-to-dead” comparisons between HR and RFA for technically resectable HCCs. In fact, several studies present the use of RFA for treatment of ‘unresectable’ tumours, mainly associated with advanced disease (Child–Pugh B/C HCC, or multiple tumours)10,16,18,21,26,32,33,34,35,36,37,38, or in older patients unfit for surgery7,13,14,18,30,31. Therefore, the results could be potentially biased since HR and RFA patients represent different populations as regards clinical characteristics that are known to influence postoperative outcomes. Although the large pooled population included in the meta-analysis could accommodate the limitations derived from such heterogeneity, further RCTs are warranted to validate the results of the current study. Meanwhile, the between-study heterogeneity observed in the majority of our analyses maybe due to any potentially relevant differences between the study designs and methodologies, such as populations from which the study samples are drawn, as well as number of patients included in each study. We attempted to accommodate this heterogeneity by implementing the random-effects evaluation model. This does not completely rule out the effect of heterogeneity between studies, but one may expect a limited influence.
By summarizing up-to-date studies with regard to the comparison of HR and RFA for small HCC, our results show that HR may provide better disease-free survival and long-term overall survival, whereas RFA is associated with lower treatment-related complication rate and shorter hospital-stay. However, these findings need to be confirmed by future RCTs. In addition, other ablation therapy like microwave ablation has recently gained great attention because of advances in microwave technology. Several studies have shown that MWA maybe as effective as HR and RFA in treating small HCC45,46,47,48. In the future, a systematic analysis and comparison of HR, MWA and RFA in the treatment of small HCC may be indispensable.
Methods
Search Strategy
This study was conducted in adherence to the PRISMA Statement guidelines49. A systematic literature search was performed using Pubmed, MEDLINE, EMBASE and CNKI (China Knowledge Resource Integrated Database) databases. No restriction was set for languages or date of publication. The following search key words were used: surgical resection, hepatic resection or hepatectomy; radiofrequency or radio-frequency; and liver cancer or hepatocellular carcinoma.
Data Extraction and Quality Assessment
Data were extracted independently by two authors (Q.X and K.S) and cross-checked to reach a consensus. The following variables were extracted from each study: (1) first author and year of the publication; (2) study design and patients characteristics; (3) clinical outcomes. The primary endpoint was efficacy, including overall and disease-free survival rates at 3 and 5 years. The secondary endpoints included complications and hospital-stay. The quality of all selected articles was assessed by using the nine-star Newcastle-Ottawa Scale50.
Eligibility Criteria
Studies were included to fulfill the following criteria: (1) compare the initial therapy effects of RFA and HR for the treatment of small HCC, no matter the etiology of liver disease, differences in viral hepatitis, or cirrhotic status. In the present study, small HCC was defined as tumor(s) ≤ 5 cm in size; (2) report on at least one of the clinical outcomes mentioned above; (3) if dual or multiple studies were reported by the same institution and authors, the one of higher quality or the most recent publication was selected.
Letters, editorials and reviews without original data, case reports and studies lacking control groups were excluded. The following studies were also excluded: 1) those dealing with liver metastases or recurrence after hepatectomy; 2) those with no clearly reported outcomes of interest; 3) those sample size for either the RFA group or HR group smaller than 30.
Statistical Analysis
The meta-analysis was performed using the RevMan 5.2 software and R software with “meta” package from the Bioconductor project51,52. For dichotomous variables, OR was estimated with a 95% CI. For continuous variables, WMD was calculated. The significance of the pooled effects was determined by Z-test. Statistical heterogeneity among studies was evaluated with Q-test and I2 statistics53. Study-specific results were combined using a random-effects model, which considers both within-study and between-study variation54. Sensitivity analysis was performed to evaluate the stability of the results. Each study involved in the meta-analysis was removed each time to reflect the influence of the individual data set on the pooled effects. An estimation of potential publication bias was executed by the funnel plot, in which the SE of log (OR) of each study was plotted against its log (OR). Funnel plot asymmetry was assessed by the method of Egger's linear regression test, a linear regression approach to measure funnel plot asymmetry on the natural logarithm scale of the OR54. The significance of the intercept was determined by the t-test suggested by Egger (p-value < 0.05 was considered representative of statistically significant publication bias).
References
Ferlay, J. et al. Cancer incidence and mortality worldwide: GLOBOCAN 2012 v1.0, IARC Cancer Base No. 11. (2013).Available from: http://globocan.iarc.fr, accessed on 01/10/2014
Yang, J. D. & Roberts, L. R. Hepatocellular carcinoma: A global view. Nat Rev Gastroenterol Hepatol 7, 448–58 (2010).
Poon, R. T., Fan, S. T., Tsang, F. H. & Wong, J. Locoregional therapies for hepatocellular carcinoma: a critical review from the surgeon's perspective. Ann Surg 235, 466–86 (2002).
Minami, Y. & Kudo, M. Radiofrequency ablation of hepatocellular carcinoma: Current status. World J Radiol 2, 417–24 (2010).
Cucchetti, A., Piscaglia, F., Cescon, M., Ercolani, G. & Pinna, A. D. Systematic review of surgical resection vs radiofrequency ablation for hepatocellular carcinoma. World J Gastroenterol 19, 4106–18 (2013).
Huang, J. et al. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann Surg 252, 903–12 (2010).
Yun, W. K. et al. Superior long-term outcomes after surgery in child-pugh class a patients with single small hepatocellular carcinoma compared to radiofrequency ablation. Hepatol Int 5, 722–9 (2011).
Chen, M. S. et al. A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg 243, 321–8 (2006).
Feng, K. et al. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J Hepatol 57, 794–802 (2012).
Nishikawa, H. et al. Comparison of percutaneous radiofrequency thermal ablation and surgical resection for small hepatocellular carcinoma. BMC Gastroenterol 11, 143 (2011).
Peng, Z. W. et al. Radiofrequency ablation versus hepatic resection for the treatment of hepatocellular carcinomas 2 cm or smaller: a retrospective comparative study. Radiology 262, 1022–33 (2012).
Ramasamy, A., Mondry, A., Holmes, C. C. & Altman, D. G. Key issues in conducting a meta-analysis of gene expression microarray datasets. PLoS Med 5, e184 (2008).
Hung, H. H. et al. Survival rates are comparable after radiofrequency ablation or surgery in patients with small hepatocellular carcinomas. Clin Gastroenterol Hepatol 9, 79–86 (2011).
Hong, S. N. et al. Comparing the outcomes of radiofrequency ablation and surgery in patients with a single small hepatocellular carcinoma and well-preserved hepatic function. J Clin Gastroenterol 39, 247–52 (2005).
Lupo, L. et al. Single hepatocellular carcinoma ranging from 3 to 5 cm: radiofrequency ablation or resection? HPB (Oxford) 9, 429–34 (2007).
Montorsi, M. et al. Survival and recurrences after hepatic resection or radiofrequency for hepatocellular carcinoma in cirrhotic patients: a multivariate analysis. J Gastrointest Surg 9, 62–7; discussion 67–8 (2005).
Cho, C. M. et al. The comparative results of radiofrequency ablation versus surgical resection for the treatment of hepatocellular carcinoma. Korean J Hepatol 11, 59–71 (2005).
Gao, W. et al. Therapeutic effect of radiofrequency ablation in unsuitable operative small hepatocellular carcinoma. Chin J Med Imaging Technol 23, 254–257 (2007).
Zhou, T., Qiu, Y., Kong, W., Zhang, W. & Ding, Y. Comparing the effect of radiofrequency ablation and surgical resection for the treatment of small hepatocellular. J Hepatobiliary Surg 15, 424–427 (2007).
Abu-Hilal, M. et al. Surgical resection versus radiofrequency ablation in the treatment of small unifocal hepatocellular carcinoma. J Gastrointest Surg 12, 1521–6 (2008).
Guglielmi, A. et al. Radiofrequency ablation versus surgical resection for the treatment of hepatocellular carcinoma in cirrhosis. J Gastrointest Surg 12, 192–8 (2008).
Santambrogio, R. et al. Surgical resection versus laparoscopic radiofrequency ablation in patients with hepatocellular carcinoma and Child-Pugh class a liver cirrhosis. Ann Surg Oncol 16, 3289–98 (2009).
Liu, H., Hu, J., Weng, H., Feng, L. & Cao, H. Effect and safety of radiofrequency catheter ablation for single small hepatocellular carcinoma. Pract Clin Med 12, 16–18 (2011).
Du, J. et al. The curative effect of percutaneous RFA and radical resection to small hepatocellular carcinoma. Clin J Med Offic 40, 570–572 (2012).
Peng, Z. W. et al. Radiofrequency ablation versus hepatic resection for the treatment of hepatocellular carcinomas 2 cm or smaller: a retrospective comparative study. Radiology 262, 1022–33 (2012).
Wang, J. H., Wang, C. C., Hung, C. H., Chen, C. L. & Lu, S. N. Survival comparison between surgical resection and radiofrequency ablation for patients in BCLC very early/early stage hepatocellular carcinoma. J Hepatol 56, 412–8 (2012).
Desiderio, J. et al. Could radiofrequency ablation replace liver resection for small hepatocellular carcinoma in patients with compensated cirrhosis? A 5-year follow-up. Langenbecks Arch Surg 398, 55–62 (2013).
Lai, E. C. & Tang, C. N. Radiofrequency ablation versus hepatic resection for hepatocellular carcinoma within the Milan criteria–a comparative study. Int J Surg 11, 77–80 (2013).
Tohme, S. et al. Radiofrequency ablation compared to resection in early-stage hepatocellular carcinoma. HPB (Oxford) 15, 210–7 (2013).
Wong, K. M. et al. Survival comparison between surgical resection and percutaneous radiofrequency ablation for patients in Barcelona Clinic Liver Cancer early stage hepatocellular carcinoma. Indian J Gastroenterol 32, 253–7 (2013).
Guo, W. X. et al. Percutaneous radiofrequency ablation versus partial hepatectomy for multicentric small hepatocellular carcinomas: a nonrandomized comparative study. World J Surg 34, 2671–6 (2010).
Hasegawa, K. et al. Comparison of resection and ablation for hepatocellular carcinoma: a cohort study based on a Japanese nationwide survey. J Hepatol 58, 724–9 (2013).
Hiraoka, A. et al. Efficacy of radiofrequency ablation therapy compared to surgical resection in 164 patients in Japan with single hepatocellular carcinoma smaller than 3 cm, along with report of complications. Hepatogastroenterology 55, 2171–4 (2008).
Imai, K. et al. Comparison between hepatic resection and radiofrequency ablation as first-line treatment for solitary small-sized hepatocellular carcinoma of 3 cm or less. Hepatol Res 43, 853–864 (2013).
Ueno, S. et al. Surgical resection versus radiofrequency ablation for small hepatocellular carcinomas within the Milan criteria. J Hepatobiliary Pancreat Surg 16, 359–66 (2009).
Vivarelli, M. et al. Surgical resection versus percutaneous radiofrequency ablation in the treatment of hepatocellular carcinoma on cirrhotic liver. Ann Surg 240, 102–7 (2004).
Zhang, J., Liu, H., Zhou, L., Cui, P. & Si, C. The effectiveness of radiofrequency ablation for the treatment of liver cancer. J Hepatobiliary Surg 19, 30–33 (2011).
Bu, X., Wang, Y., Ge, Z., Wang, Z. & Zhang, D. Comparison of radiofrequency ablation and surgical resection for small primary liver carcinoma. Chin Arch Gen Surg 3, 127–131 (2009).
Reuter, N. P., Woodall, C. E., Scoggins, C. R., McMasters, K. M. & Martin, R. C. Radiofrequency ablation vs. resection for hepatic colorectal metastasis: therapeutically equivalent? J Gastrointest Surg 13, 486–91 (2009).
Ni, J. et al. Percutaneous ablation therapy versus surgical resection in the treatment for early-stage hepatocellular carcinoma: a meta-analysis of 21,494 patients. J Cancer Res Clin 139, 2021–2033 (2013).
Wakai, T. et al. Long-term outcomes of hepatectomy vs percutaneous ablation for treatment of hepatocellular carcinoma < or = 4 cm. World J Gastroenterol 12, 546–52 (2006).
Ma, Y. et al. Association between vitamin D and risk of colorectal cancer: a systematic review of prospective studies. J Clin Oncol 29, 3775–82 (2011).
Zhou, Y. et al. Meta-analysis of radiofrequency ablation versus hepatic resection for small hepatocellular carcinoma. BMC Gastroenterol 10, 78 (2010).
Xu, G. et al. Meta-analysis of surgical resection and radiofrequency ablation for early hepatocellular carcinoma. World J Surg Oncol 10, 163 (2012).
Lu, M. D. et al. Percutaneous microwave and radiofrequency ablation for hepatocellular carcinoma: a retrospective comparative study. J Gastroenterol 40, 1054–60 (2005).
Ohmoto, K. et al. Comparison of therapeutic effects between radiofrequency ablation and percutaneous microwave coagulation therapy for small hepatocellular carcinomas. J Gastroenterol Hepatol 24, 223–7 (2009).
Qian, G. J. et al. Efficacy of microwave versus radiofrequency ablation for treatment of small hepatocellular carcinoma: experimental and clinical studies. Eur Radiol 22, 1983–90 (2012).
Shi, J. et al. Comparison of microwave ablation and surgical resection for treatment of hepatocellular carcinomas conforming to Milan criteria. J Gastroenterol Hepatol 29, 1500–7 (2014).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62, e1–34 (2009).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25, 603–5 (2010).
Ihaka, R. & Robert, G. R: A Language for Data Analysis and Graphics. J Comput Graph Stat 5, 299–314 (1996).
Reimers, M. & Carey, V. J. Bioconductor: an open source framework for bioinformatics and computational biology. Methods Enzymol 411, 119–34 (2006).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat Med 21, 1539–58 (2002).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin Trials 7, 177–88 (1986).
Author information
Authors and Affiliations
Contributions
X.M., Q.X. and S.K. wrote the main manuscript. Q.X. and S.K. collected the data. Q.X., X.Y. and S.K. performed the statistical analysis and prepared figures 1–4. All authors reviewed the manuscript.
Ethics declarations
Competing interests
Q.X., X.Y. and X.M. are employees of bioMérieux (Shanghai) Co., Ltd. No other potential conflicts of interest were disclosed by authors.
Additional information
Financial support Our study was supported by bioMe´rieux company.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Xu, Q., Kobayashi, S., Ye, X. et al. Comparison of Hepatic Resection and Radiofrequency Ablation for Small Hepatocellular Carcinoma: A Meta-Analysis of 16,103 Patients. Sci Rep 4, 7252 (2014). https://doi.org/10.1038/srep07252
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep07252
This article is cited by
-
Comparison of laparoscopic hepatectomy and percutaneous radiofrequency ablation for the treatment of small hepatocellular carcinoma: a meta-analysis
BMC Surgery (2024)
-
Dorsal approach with Glissonian approach for laparoscopic right anatomic liver resections
BMC Gastroenterology (2021)
-
Prediction early recurrence of hepatocellular carcinoma eligible for curative ablation using a Radiomics nomogram
Cancer Imaging (2019)
-
Microwave ablation compared with hepatic resection for the treatment of hepatocellular carcinoma and liver metastases: a systematic review and meta-analysis
World Journal of Surgical Oncology (2019)
-
Efficacy and safety of radiofrequency ablation versus minimally invasive liver surgery for small hepatocellular carcinoma: a systematic review and meta-analysis
Surgical Endoscopy (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.