Abstract
Although obstructive sleep apnea (OSA) patients are at high risk of developing cardiovascular disease (CVD), only a small proportion is currently diagnosed. To explore and identify the differentially expressed proteins/peptides of OSA patients with CVDs, a mass spectrometry-based salivary analysis was performed. In our study, eleven peaks were observed differentially expressed in saliva from the non-CVD and CVD groups. Five masses mass peaks (1594.1, 1673.7, 1196.6, 1290.5 and 1447.0 Da) showed an upregulated trend in the CVD group, whereas six mass peaks (3038.6, 2164.3, 2301.4, 3195.0, 2628.4 and 1721.9 Da) were downregulated in the CVD group. In addition, the alpha-2-HS-glycoprotein (AHSG) levels in saliva were verified to be decreased in CVD group compared to non-CVD group. Analysis of the salivary peptidome provides a promising approach to screening for novel biomarkers before further identification and may contribute to early diagnosis of CVD patients with OSA.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVDs) affect a wide range of individuals and remain one of the leading causes of death in the general population. According to the World Health Organization (WHO) report, CVDs such as hypertension, coronary artery disease (CAD) and stroke were responsible for 30% (17.3 million) of the 57 million global deaths in 2008 (Global Atlas on cardiovascular disease prevention and control). Over the past two decades, death from CVDs has increased rapidly in low- and middle-income counties. Currently, in China, CVDs are the top health burden1,2. The causes of CVD are believed to be multifactorial. Several risk factors for CVD are recognized, including tobacco, alcohol, physical inactivity, diabetes and raised blood cholesterol level. Obstructive sleep apnea (OSA) is also believed to be an important independent risk factor for CVDs3,4,5.
OSA is a disease closely related to CVDs, characterized by repetitive partial or complete closure of the pharynges during sleep, resulting in apnea or hypopnea6. OSA and CVDs share certain risk factors, such as obesity and the incidence of vascular diseases in OSA patients is likely to be higher than that of the general population7. The potential of OSA patients to develop cardiovascular system disorders is becoming an important issue to which clinical practitioners and science researchers should pay attention. Although OSA patients are at high risk of developing CVDs, only a small proportion of OSA patients with CADs are currently diagnosed. Undiagnosed CVD patients among the OSA population represent a potential public health burden. Although the underlying molecular causes of cardiac dysfunction in OSA are still not completely understood, several possible biologic mechanisms, such as sympathetic excitation, metabolic dysregulation and inflammation induced by intermittent hypoxia, may be involved8.
Identification of biomarkers involved in the pathogenesis of vascular disease in OSA patients may facilitate early diagnosis and contribute to understanding the complex mechanism of this disease. The development of proteomic/peptidomic-based approaches has been used to identify biomarkers of various diseases, leading to the use of body fluid as a diagnostic tool. Approximately 20% of whole cellular proteins are secreted9, providing information on physiological and pathological processes. Saliva is a complex secretion originating from the oral salivary glands. It contains protein from salivary glands and crevicular fluid, oral bacteria and their products, food debris and desquamated epithelial cells10. Salivary proteomic/peptidomic analysis has become poplar due to its provision of abundant information and convenient non-invasive collection methods. Many studies have confirmed that proteins/peptides from saliva may serve as potential biomarkers of various diseases, both oral and systemic11,12.
Since it was first introduced in the 1980s13, matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS), which is based on the capture of proteins/peptides on chemically modified surfaces, has been used as a powerful tool to analyze proteins and peptides. With the aid of weak cation-exchange (WCX) magnetic beads, low-molecular-weight proteins or peptides in various biologic samples have been selectively separated and enriched, thus facilitating identification of low molecular mass protein or peptide expression patterns. Previously, we identified several peptides that showed increased or reduced expression in the saliva of patients undergoing various orthodontic treatment period14.
In this study, we used MALDI-TOF MS and WCX magnetic beads to assess saliva from OSA patients with and without CVDs. We aimed to identify differentially expressed proteins/peptides of OSA patients with CVDs compared with controls to identify a panel of specific biomarkers for early identification of CVDs in patients with OSA.
Results
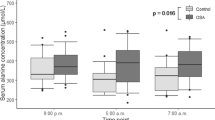
We investigated the differences between CVD-OSA and non-CVD-OSA patients to identify promising protein/peptide biomarkers for early disease prediction. The clinical characteristics of CVD patients and controls are shown in Table 1. Examples of both the raw and processed entire mass spectra of the enriched peptide samples from MALDI-TOF MS are shown in Figure 1. An average of 92 peaks ranging from 1000 to 7000 Da were detected. Of these, 39 showed a p value < 0.05 according to Student's t test and 11 with an average mass area > 300 (3038.6, 2164.3, 2301.4, 1594.1, 1673.7, 3195.0, 1196.6, 1290.5, 2628.4, 1721.9 and 1447.0 Da; Table 2). The p values remains significant after correcting for multiple comparisons using false discovery rate (FDR) correction. Of the 11 peptide masses, five masses (1594.1, 1673.7, 1196.6, 1290.5 and 1447.0 Da) showed an upregulated trend in the CVD group, whereas six potential mass peaks (3038.6, 2164.3, 2301.4, 3195.0, 2628.4 and 1721.9 Da) were downregulated in the CVD group (Figure 2). The most significant differences were exhibited by the 3038.6 and 2164.3 Da peptides (p < 0.01, both showed a decreased tendency in the CVD group; Figure 3).
Differentially presented peptides were used to establish discriminatory models, using four different algorithms (Support Vector Machine, SVM; k-Nearest Neighbor, KNN; Linear Discriminant Analysis, LDA; radial basis function neural network, RBF). The models based on SVM and RBF showed better performances, with 92.31% sensitivity and 70.00% specificity (Table 3). Independent salivary samples (5 from non-CVD-OSA and 10 from CVD-OSA patients) were collected to test the robustness of the models. The models showed high sensitivity of identification of OSA patients with CVDs though the specificity of the models was not high (Table 4).
Moreover, we successfully predicted four (1721.9, 3195.0, 2164.3 and 1447.0 Da) of the 11 differentially expressed peptides (Table 2). Peptides 1721.9 and 3195.0 Da were predicted to be isoform I of the fibrinogen alpha chain (FGA) precursor, 2164.3 and 1447.0 Da were predicted to be alpha-2-HS-glycoprotein (AHSG) precursor and tubulin alpha-4A chain (TUBA4A), respectively.
The expression of AHSG between two groups was predicted to be significantly different (p < 0.01). To further verify it, the presence of AHSG in each salivary sample was measured by western blotting. The AHSG levels in saliva were also observed to be decreased in CVD group compared to non-CVD group (Figure 4).
Salivary AHSG levels are decreased in OSA patients with CVDs compared to control.
(A) Western blotting reveals the presence of AHSG in each salivary sample. The salivary amylase (AMY1A) is used as an internal control to normalize the amount of AHSG. Equal amounts of the total protein were used for each sample. Western blotting were performed in parallel with constant conditions for each blot, including the transfer time for proteins, the concentrations of the antibodies, the exposure time, etc. (B) The relative density of the AHSG bands normalized to AMY1A. The levels of salivary AHSG are lower in OSA-CVD patients compared to non-OSA-CVD subjects. The bands were quantified using ImageJ software (http://rsbweb.nih.gov/ij/). The density of AHSG was divided by that of AMY1A for each sample to normalize the level of AHSG. ** p < 0.01 by two-tailed Student's t-test.
Discussion
Our results have two major implications: first, we identified a salivary peptidome panel based on 11 biomarkers, two of which were significantly differently expressed and were highly predictive of CVDs, thus developing a panel of fingerprints assays to discriminate OSA patients with CVD from controls. Second, our data offer evidence for a pathophysiological link between OSA and CVD. OSA and CVD may share some common biological processes. Both epidemiological and biochemical evidence suggest that inflammation is involved in the pathogenesis of CVDs15,16. Due to intermittent hypoxia and sympathetic activation, systemic inflammation is recognized to be associated with OSA17. This suggests that circulating inflammatory cytokines indicate the severity, stage or prognosis of disorders associated with chronic inflammation, such as cardiac disease and certain tumors18.
AHSG, which is mostly synthesized by liver and secreted into circulating body fluid, has been widely detected in various body fluids, such as plasma19, cerebrospinal fluid20, urine21, semen and saliva22. AHSG is known as an acute-phase protein and its level decreased in acute inflammation situation. More and more evidences suggest the important role of AHSG in the cardiovascular system23. Reduced circulating AHSG levels were observed in patients with OSA and they are associated with OSA severity19. However, the exact role of AHSG in CVDs and OSA remains controversial. Low AHSG levels in body fluids could be a consequence of chronic inflammation, which occur in CVDs and OSA. In our study, we observe a decline of AHSG in salivary samples of OSA patients with CVDs. This study shows that OSA patients with a decreased AHSG level in circulating body fluids are at high risk of developing into CVDs. It's promising that salivary AHSG serves as a biomarker for the predicting clinical outcome in OSA patients.
OSA patients share obstructive hypoventilation and hypoxemia, while some who suffer from CVDs have health conditions that differ from those of “healthy” patients. Hypoxia stimulates changes in proteins or peptides in the body and so expression in cells and surrounding fluids. Saliva is a promising source for the early prediction of CVDs in OSA patients. However, a larger sample size is needed to validate the reliability of our prediction model. Additional typical cases of CVDs should be examined to confirm the differentially expressed peptides we report here. The detection of these peptides is meaningful for further understanding of the interaction between CVDs and OSA. Despite their defects and confusing results, MS methods can be used as an initial method for screening peptides of interest before further validation. Analysis of body fluids remains a promising method of identifying novel peptide markers of disease.
Methods
Ethics statement
This study was approved by the Peking University Biomedical Ethics Committee. All subjects provided written consent before participating in the study.
Study participants and sample collection
A total of 23 patients (14 males, nine females) diagnosed with OSA and seeking treatment at Orthodontic Department at Beijing Anzhen Hospital were recruited. Additional 15 subjects with OAS were recruited for validation. Table 5 shows the detailed parameters of the participants. The OSA patients were divided into two groups: OSA patients with CVD (CVD group) and OAS patients without CVD (non-CVD group). The clinical diagnosis of cardiovascular diseases was conducted by the Cardiovascular Center of Anzhen hospital.
All subjects were asked to refrain from drinking and eating the previous evening. Oral hygiene practices were forbidden 2 h before saliva collection. Prior to saliva sample collection, subjects were taught how to stimulate the sublingual caruncle with the tip of their tongue. The detailed collection process was according to our previous saliva sample protocol14. A ~2–6 mL whole saliva sample was collected into a 50-mL sterile centrifuge tube. The tubes were kept on ice during the collection procedure.
Sample preparation
The saliva samples were centrifuged at 12,000 rpm for 10 min at 4°C. Ethylene diamine tetraacetic acid (1 mM; Sigma, St. Louis, MO, USA) and 1 mM phenylmethyl sulfonylfluoride (Sigma) were added to the supernatants. One-hundred-microliter aliquots of saliva supernatant from each subject were transferred into fresh tubes and stored at −80°C before further analysis. To preserve the protein and peptide content of the saliva, repeated freeze-thaw cycles were avoided.
Protein concentration was determined using a Lowry assay (BioTek, Hercules, CA, USA). The weak-cation-exchange (WCX) magnetic bead kit (SPE-C; Bioyong Tech, Beijing, China) was used to enrich low-molecular-weight proteins/peptides from the salivary suspension according to the operation manual. In brief, the saliva samples were fractionated with the assistance of magnetic beads. After binding, washing and eluting, the eluted low-molecular-mass proteins or peptides were subjected to MS analysis.
Mass spectrum analysis
MALDI-TOF MS analysis was performed using an UltraFlex III MALDI-TOF mass spectrometer (Bruker Daltonics, Germany). Five microliters of HCCA substrate solution (0.4 g/L, in acetone and ethanol) and 0.8–1.2 μL of the elute were mixed. Next, 0.8–1.2 μL of this mixture was applied to a metal target plate and dried at room temperature. Finally, the prepared sample was analyzed by MALDI-TOF MS. All samples were spotted in triplicate in the same assay with a good reproducibility. Instrument calibration parameters were determined using a standard peptide and protein mixture.
Data processing and protein/peptide identification
Raw spectra acquired from the MALDI experiments were processed using the BioExplorer statistical package (BioyongTech). Each spectrum was normalized, baseline-corrected and smooth-applied using default parameters. All quality peaks (signal-to-noise ratio > 5) with a mass-to-charge radio (m/z) value of 1,000–10,000 were obtained. Student's t-test was used to compare the peptide peak intensities in the two groups. Finally, each statistic was corrected for multiple comparisons using false discovery rate (FDR) controlling procedure (with a FDR of 0.05)24, which predicts the proportion of false positives in the significant observations. Corrected P values of <0.05 were regarded as statistically significant.
To predict the differentially expressed peptides between the groups, the same group samples were pooled and then analyzed by liquid chromatography-mass spectrometry (LC-MS). Liquid chromatography was performed on a nano Acquity UPLC system (Waters Corporation, Milford, USA) connected to a LTQ Orbitrap XL mass spectrometer (Thermo Scientific, Bremen, Germany) equipped with an online nano-electrospray ion source (Michrom Bioresources, Auburn, USA). Peptides were resuspended with 12 μl solvent A (5% acetonitrile, 0.1% formic acid in water). 10 μl peptide solution was loaded onto the Captrap Peptide column (2 mm × 0.5 mm, Michrom Bioresources, Auburn, USA) at a 20 μl/min flow rate of solvent A for 5 min and then was separated on a Magic C18AQ reverse phase column (75 μm id × 15 cm, Michrom Bioresources, Auburn, USA) with a linear gradient. Starting from 5% B (90% acetonitrile, 0.1% formic acid in water) to 45% B in 70 min. The column was re-equilibrated at initial conditions for 15 min. The column flow rate was maintained at 300 nL/min and column temperature was maintained at 35°C. The electrospray voltage of 1.8 kV versus the inlet of the mass spectrometer was used.
LTQ Orbitrap XL mass spectrometer was operated in the data-dependent mode to switch automatically between MS and MS/MS acquisition. Survey full-scan MS spectra with one microscan (m/z 300–1800) was acquired in the Obitrap with a mass resolution of 60,000 at m/z 400, followed by MS/MS of the eight most-intense peptide ions in the LTQ analyzer. For MS/MS, we used an isolation window of 2 m/z. Single charge state was rejected and dynamic exclusion was used with two microscans in 10 s and 90 s exclusion duration. For MS/MS, precursor ions were activated using 35% normalized collision energy at the default activation q of 0.25 and an activation time of 30 ms. The spectrum were recorded with Xcalibur (version 2.0.7) software. The tandem MS spectra were analyzed using BioworkBrowser version 3.3.1 SP1 and the resulting mass lists were used for a database search with Sequest™ [Database IPI Human (3.45)]. The searching parameters were set up as follows: the mass tolerance of parent ions and fragment ions were 20 ppm and 0.5 Da, respectively; no enzyme cleavage mode; the variable modification was oxidation of methionine; Peptide identification was accepted with Xcorr of greater than or equal to 3.00 for triply and 2.50 for doubly charged ions and all with ΔCn ≥ 0.1, Peptide probability < = 0.01.
Western blotting analysis
Salivary protein concentration was determined using BCA kit (Solarbio, China). Salivary total protein (15 μg) underwent electrophoresis in 10% SDS-PAGE gels using Mini-PROTEAN Tetra Cell System (Bio-Rad, USA). Proteins were then transferred to NC membranes. The total protein load was checked visually by Ponceau staining before immunodetection. The membranes were blocked overnight at 4°C with 10% skimmed milk in Tris-buffered saline (TBS, PH 7.4) followed by washing with TBS buffer containing 0.05% tween 20 (TBST). Membranes were incubated with the primary antibody specific for alpha-2-HS-glycoprotein (Sino Biological Inc., China; 10318-R001; 1:2000) and salivary amylase (anti-AMY1A antibody, Sigma-Aldrich Co., USA, 1:5000) at room temperature for 1 h. Infrared (IR)-labeled secondary antibody (Gene Company Limited, Hong Kong; Goat anti-rabbit IgG, 1:15000) for 0.5 h at room temperature. The excess secondary antibody was removed by washing with TBST. The immunoreactive bands were visualized by Odyssey scanner (Gene Company Limited, Hong Kong). Western blotting bands were quantified using Image J software (http://rsbweb.nih.gov/ij/).
References
Wei, X. et al. Characteristics of high risk people with cardiovascular disease in chinese rural areas: clinical indictors, disease patterns and drug treatment. PLoS One 8, e54169 (2013).
Hu, S. S. et al. Outline of the report on cardiovascular disease in China, 2010. Biomedical and environmental sciences: BES 25, 251–256 (2012).
Ursavas, A. & Ege, E. [Obstructive sleep apnea and cardiovascular diseases]. Anadolu Kardiyol Derg 3, 150–155 (2003).
Marin, J. M. et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA 307, 2169–2176 (2012).
Das, A. M. & Khan, M. Obstructive sleep apnea and stroke. Expert Rev Cardiovasc Ther 10, 525–535 (2012).
Sunderram, J. & Androulakis, I. P. Molecular mechanisms of chronic intermittent hypoxia and hypertension. Crit Rev Biomed Eng 40, 265–278 (2012).
Peker, Y., Hedner, J., Kraiczi, H. & Loth, S. Respiratory disturbance index: an independent predictor of mortality in coronary artery disease. Am J Respir Crit Care Med 162, 81–86 (2000).
Caples, S. M., Gami, A. S. & Somers, V. K. Obstructive sleep apnea. Ann Intern Med 142, 187–197 (2005).
Tamas, J., Mak, M., Klebovich, I., Vereczkey, L. & Toth, E. Mass spectrometric characterization of some human metabolites of flumecinol. Biomed Environ Mass Spectrom 15, 229–232 (1988).
Chiappin, S., Antonelli, G., Gatti, R. & De Palo, E. F. Saliva specimen: a new laboratory tool for diagnostic and basic investigation. Clin Chim Acta 383, 30–40 (2007).
Aurer, A., Jorgic-Srdjak, K., Plancak, D., Stavljenic-Rukavina, A. & Aurer-Kozelj, J. Proinflammatory factors in saliva as possible markers for periodontal disease. Coll Antropol 29, 435–439 (2005).
Giusti, L. et al. Proteome analysis of whole saliva: a new tool for rheumatic diseases--the example of Sjogren's syndrome. Proteomics 7, 1634–1643 (2007).
Tanaka, K., Waki, H. & Ido, Y. Protein and polymer analyses up to m/z 100 000 by laser ionization time-of-flight mass spectrometry. Rapid Commun. Mass Spectrom 2, 151 ¨C153 (1988).
Zhang, J. et al. Magnetic bead-based salivary peptidome profiling analysis during orthodontic treatment durations. Biochem Biophys Res Commun 421, 844–849 (2012).
Davis, N. E. Atherosclerosis--an inflammatory process. J Insur Med 37, 72–75 (2005).
Tracy, R. P. Epidemiological evidence for inflammation in cardiovascular disease. Thromb Haemost 82, 826–831 (1999).
Levy, P. et al. Sleep deprivation, sleep apnea and cardiovascular diseases. Front Biosci (Elite Ed) 4, 2007–2021 (2012).
Jarai, T. et al. Mass spectrometry-based salivary proteomics for the discovery of head and neck squamous cell carcinoma. Pathol Oncol Res 18, 623–628 (2012).
Barcelo, A. et al. Reduced plasma fetuin-A levels in patients with obstructive sleep apnoea. The European respiratory journal 40, 1046–1048, 10.1183/09031936.00011912 (2012).
Harris, V. K. et al. Cerebrospinal fluid fetuin-A is a biomarker of active multiple sclerosis. Multiple sclerosis (Houndmills, Basingstoke, England), 10.1177/1352458513477923 (2013).
Zhou, H. et al. Exosomal Fetuin-A identified by proteomics: a novel urinary biomarker for detecting acute kidney injury. Kidney international 70, 1847–1857, 10.1038/sj.ki.5001874 (2006).
Yasuda, T. et al. Alpha-2-HS-glycoprotein (AHSG) polymorphism in semen and saliva. Electrophoresis 17, 793–796, 10.1002/elps.1150170429 (1996).
Mori, K., Emoto, M. & Inaba, M. Fetuin-A and the cardiovascular system. Advances in clinical chemistry 56, 175–195 (2012).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological), 289–300 (1995).
Acknowledgements
The authors acknowledge the support of the physicians from the Orthodontic Department at Beijing Anzhen Hospital for their assistance in the sampling procedure. This work was supported by grants 81200762 from National Natural Science Foundation of China.
Author information
Authors and Affiliations
Contributions
J.X.L. and F.C. conceived the study and participated in its design; H.Z. and R.X.L. carried out a major portion of the study, including work design, sample collection, sample preparation and data analysis; H.Z. drafted the manuscript; S.N.Z., J.N.Z. and Q.W.M. participated in the data analysis.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Zheng, H., Li, R., Zhang, J. et al. Salivary biomarkers indicate obstructive sleep apnea patients with cardiovascular diseases. Sci Rep 4, 7046 (2014). https://doi.org/10.1038/srep07046
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep07046
This article is cited by
-
A Review on Saliva-Based Health Diagnostics: Biomarker Selection and Future Directions
Biomedical Materials & Devices (2024)
-
A comparative pharmacogenomic analysis of three classic TCM prescriptions for coronary heart disease based on molecular network modeling
Acta Pharmacologica Sinica (2020)
-
Short-term effects of continuous positive airway pressure on oxidative stress in severe sleep apnea
Sleep and Breathing (2019)
-
Metabolomics Profiling for Obstructive Sleep Apnea and Simple Snorers
Scientific Reports (2016)
-
Saliva in the diagnosis of diseases
International Journal of Oral Science (2016)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.