Abstract
The stress reactivity hypothesis posits that the magnitude of cardiovascular reactions to acute stress tasks is related with future blood pressure status, heart hypertrophy and atherosclerosis. We assessed the stress reactivity hypothesis and aimed to identify which physiological indices (blood pressure, heart-rate, cortisol, salivary immunoglobulin A (sIgA)) related to self-reported mental and physical health. We also assessed if physiological reactions elicited by an acute stressor were more related than basal assessments. Participants provided physiological samples, self-reported stress and health-data before and after an assessed 5–7 minute academic oral presentation. In hierarchical regression models, increased systolic and reduced sIgA reactivity was associated with better perceptions of mental health. Reactivity data were more related to self-reported data than basal data. In line with the only 2 studies to assess the reactivity hypothesis with self-perceived health, increased systolic reactivity was best associated with better perceived physical and mental health. The findings suggest that increased SBP reactivity may also be associated with positive health outcomes. Further research is required to determine if increased or decreased sIgA reactivity is most predictive of future morbidity.
Similar content being viewed by others
Introduction
Substantial cardiovascular responses to acute psychological stress as opposed to acute physical exertion may be considered pathophysiological1,2. The stress reactivity hypothesis posits that the magnitude of cardiovascular reactions to acute stress tasks is related with future blood pressure status, heart hypertrophy and atherosclerosis1. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) reactivity, as well as heart rate (HR) reactivity, have all been related to future morbidity; but it is SBP reactivity that appears to be the best predictor2.
Despite the impressive evidence provided by the meta-analysis of 31 prospective studies linking stress reactivity to illness by Chida and Steptoe2, the specific pathways between stress reactivity and cardiovascular risk status have not been determined3. In particular, the interplay between the sympathetic and parasympathetic arms of the autonomic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis requires further enquiry to inform and convey the mechanics of increased reactivity upon morbidity. Additionally, the relationship of stress reactivity to self-perceived health and morbidity may assist both early intervention and our understanding of disease pathology.
Myint and colleagues4 conducted a prospective study with 17,777 participants from the general community who were free from known severe disease. Their results highlight the link between poor self-perceived health and mortality, (particularly cardiovascular disease). Importantly, these findings held after statistically controlling for age, social class and coronary disease factors such as arteriosclerosis. Unexpectedly, the only two studies to assess the stress reactivity hypothesis with self-perceived health report a positive association with SBP, DBP and cortisol reactivity in participants aged 55–605 and 24–636 years. Potentially, these unexpected findings may be explained by chronic stress which is said to blunt reactivity7, but was not measured in either study. Both the abovementioned studies assessed HR, SBP and DBP with acute cognitive stressors with de Rooij and Roseboom5 also assessing salivary cortisol.
Glucocorticoids play a pivotal role in blood pressure regulation and may be a key component of cardiovascular risk8. The relationship between increased cortisol secretion and increased blood pressure and obesity8 may explain why most studies have considered the stress reactivity hypothesis solely in relation to cardiovascular and HPA axis measures9.
Despite recommendations to assess immune parameters, minimal research has occurred5. Salivary immunoglobulin A (sIgA), which is postulated to be reflective of the functional status of the entire mucosal system10, appears a good candidate, but its relationship with acute stressors is unclear with increases, reductions and no change all being reported11. The protective function of sIgA is well understood with luminal sIgA secretions impacting virus excretion, intracellular neutralization and pathogen adherence to mucosal epithelial cells12. Consideration of sIgA reactivity to an acute stressor in addition to cortisol, cardiovascular measures and self-perceived health may assist in disentangling the relationship between acute stress and sIgA.
Using an afternoon academic oral presentation as a psychological stressor we gathered assessments of cortisol, sIgA, HR, DBP and SBP, at the same time points one week prior and on the day of an assessed oral academic presentation. Our aim was to ascertain what association the physiological indices had with perceived health after controlling for confounders and self-reported stress, at baseline and after an acute psychological stressor. Further aims were to determine which physiological indices were most associated with perceived health and to identify if the reactivity hypothesis was supported (i.e., physiology difference scores would be more related to self-perceived health than basal measurements).
Methods
Participants
Australian undergraduate students were recruited from afternoon laboratory classes; 77 met the criteria and agreed to participate, with the gender ratio commensurate with enrolments (17 = male, 60 = female). Participants (age M = 19.4, SD = 1.4) self-excluded on the basis of endocrine disorder, pregnancy, suffering from depression or psychiatric illnesses, or currently taking glucocorticoid medication as these factors can confound cortisol assays13. Those over 30 years of age were excluded to minimize the individual difference error14. Institutional ethics approval was obtained and the study was carried out in accordance with these guidelines. All subjects signed informed consent forms.
Procedure
Students were required to deliver an assessed 5–7 minute oral presentation to their peers that contributed 10% to their final grade. Participants chose from a small list of topics (inherited diseases) and were provided with the criteria they needed to cover in their presentation. They were invited to participate in the study two weeks prior to their presentation. Participants were instructed verbally and via a take home pamphlet of the protocol for the saliva collection and were reminded not to consume caffeine, exercise heavily, or brush their teeth or eat two hours prior to providing samples15.
Physiological samples
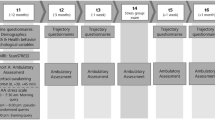
Saliva samples were collected via Salivette© (Sarstedt Inc., Rommelsdorf, Germany) at two time points one week apart. Afternoon cortisol and sIgA samples were collected between 14.15 and 15.00 one week prior to the oral presentation and 20 minutes (cortisol) and 2 minutes (sIgA) post-presentation.
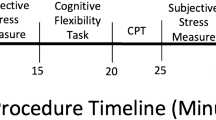
Blood pressure and HR were assessed 1 week prior to the oral presentation (between 14.15 and 15.00) and 1 minute prior to presentation using an automated blood pressure monitor (HEM7203, OMRON, Singapore). Participants were seated and blood pressure readings were collected by a trained researcher using the protocol recommended by the manufacturer. The complete study design is illustrated below (Table 1).
Prior to analysis of the cortisol concentration, samples were thawed and centrifuged at 3000 rpm for 15 minutes to remove debris from the saliva. High sensitivity salivary cortisol EIA kits (No. 1-3002 Salimetrics LLC, PA) were used to determine cortisol levels. The intra- and inter-assay variation of the cortisol kit was 3.35% and 3.75% respectively and the detection limit was 0.03 μg/L. Optical density measurements were performed at 450 nm with a Synergy HT Multi-detection Microplate reader (Bio-Tek instruments Inc., Winooski, VT). Concentrations of the selected compounds were calculated using KC4 v3.4 software (Bio-Tek instruments). Duplicates of each sample were taken and the mean concentration (ng/ml) was calculated.
The calculation of sIgA involved participants passively drooling approximately 1 teaspoon of saliva into a plastic tube (Sarstedt Inc), which is commonly used for salivette collection of saliva (i.e., the cotton salivette had been removed). The samples were frozen, thawed and centrifuged in the same manner as the cortisol samples described above. The sIgA concentration was calculated using the salivary sIgA indirect enzyme immunoassay kit (Salimetrics). Duplicates of each sample were taken and the mean concentration (μg/ml) was calculated.
Psychological measures
Perceived stress
The 10 item Perceived Stress Scale16 was used to assess perceived stress through questions targeting thoughts and feelings during the last month. Participants indicate their responses to each item ranging from 0 indicating ‘never’ to 4 indicating ‘very often’. Cronbach alpha in the current study was α = .99.
A single item Acute Stress question that asked “how would you rate your current level of anxiety?” on a 1(low)–9 (high) Likert scale was used to assess acute stress.
Physical and mental health
The SF-36 General Health Measure (SF-36)17 is a 36 item questionnaire that contains 8 subscales including: physical functioning, role limitations due to physical problems, social functioning, bodily pain, general mental health, role limitations due to emotional problems, vitality and general health perceptions. Higher scores indicate better perceptions of health. These subscales form two composite variables: Mental Health and Physical Health, which were the focus of statistical analyses. In the current study Cronbach alpha was; Physical Health, α = .65 and Mental Health, α = .73.
Data analysis
Removal of 5 multivariate outliers was necessary based on leverage and standardised residuals. The reduced sample consisted of 15 males and 57 females. Bonferroni corrected paired t-tests and Cohen's d were used to assess if the oral presentation significantly impacted self-reports of stress and the physiological indices. Hierarchical linear regression analysis was employed to compare and determine the contributions of stress (Step 2; chronic and acute stress) and physiology (Step 3; systolic and diastolic blood pressure, heart rate, cortisol and sIgA) after controlling for possible confounders (Step 1; Age, Gender), on physical and mental health at baseline and after the stressor (stressor-baseline difference).
Results
Preliminary analyses
A one-way ANOVA was conducted to compare male and female participants on all physiological and self-reported variables to ensure that the data could be classified as one group. Females were significantly more chronically stressed than males; t(70) = 2.97, p = 0.004. No other significant physiological or self-reported differences were recorded. Given the small N of males we also conducted female-only analyses and can report very similar effect sizes (with most being larger) for all regression models used.
The PSS and Physical and Mental health subscales were compared with normative data (Table 2).
At baseline, all students reported acute stress scores < 5 (0–9 scale), 64% of the acute stress scores on the day of presentation were >5. To assess if the oral presentation was viewed as stressful by participants a group of Bonferroni corrected (0.05/5 = 0.01) paired t-tests were used to measure differences between basal and stressor conditions (i.e., 1 week pre-presentation and day of presentation) (Table 3).
All assessments were significantly higher during the stressor condition (all p < 0.001) According to Cohen18 the effect of the stressor was considered small for DBP and SBP, medium for HR and large for acute stress, cortisol and sIgA.
Hierarchical regressions
The regression analysis revealed that multicollinearity of independent variables would not confound interpretation with all tolerance levels substantially above .2019. Inspection of the scatterplots of the standardised residuals against standardised predicted values indicated assumptions of linearity, homoscedasticity and independence were also met. The contribution of the physiological variables at Step 3 in the baseline models (Table 4) was not significant, though the R2 change for physical health (.11) represents a medium effect. Decreased DBP and reduced chronic stress were significantly associated and most uniquely related with self-reported physical health. The entire baseline model was significantly related to mental health; F(9, 62) = 2.170, p = 0.036, R2 = .24, but not physical health; F(9, 62) = 1.629, p = 0.127, R2 = .19,
The set of physiological difference scores (stressor-basal) was not significantly associated with perceptions of physical health; however SBP was related (Table 5). The physiological variables only explained an additional 2% of the variance for physical health when compared with the basal regression. The set of physiological difference scores was significantly associated with perceptions of mental health and explained a further 10% compared with Step 3 in the basal model. Decreased sIgA and increased SBP difference scores were both significantly related with better mental health. The entire reactivity model was significantly associated with physical; F(9, 67) = 2.044, p = 0.02, R2 = .25 and mental health; F(9, 62) = 3.911, p = 0.049, R2 = .36.
Discussion
Our findings largely align with the two previous studies that assessed the reactivity hypothesis with self-perceived health5,6 and support the hypothesis with SBP the most significantly related physiological variable with mental and physical health. sIgA was significantly related with mental health and approaching significance for physical health (B = −.20, p = 0.084). As anticipated, the reactivity models were more related with physical and mental health than the basal models.
While there is much evidence suggesting relationships between increased cardiovascular reactivity and a variety of negative health outcomes2 there is also evidence that reduced cardiovascular reactivity may place individuals at increased risk for diseases such as obesity20. Importantly, the positive association between SBP reactivity and self-perceived health is commensurate with the two other investigations that have assessed cardiovascular reactivity with self-perceived stress5,6. This association holds after statistically controlling for chronic stress in a sample reporting below normative stress and may suggest that increased cardiovascular reactivity may also be related with positive health outcomes. Chronic stress as assessed by the PSS was the most strongly related variable in 3 of the 4 regressions and underscores the need to assess this construct.
The acute psychological stressor clearly induced a stress response as evidenced by the large effect sizes attained pre-post stressor. Interestingly, it was reduced sIgA reactivity that was associated with improved health perceptions. An argument could be made that in response to acute stress, increased sIgA reactivity may be considered adaptive. The counter-argument could be that those who did not trigger HPA activation may have better coping skills or are less physiologically reactive. Future researchers are encouraged to collect prospective evidence to resolve this argument. HR, DBP and SBP account for 77% of the outcome variables in acute psychological stress research with cortisol the next most prominent at 5%9; sIga has been scarcely assessed, but the findings from this investigation suggest further empirical enquiry may be justified.
Poor self-perceived health is related with mortality (coronary disease in particular)4, increased stress reactivity (SBP, DBP) is related with disease states2 and our findings align with others5,6 suggesting increased stress reactivity is related to better perceived health. While the results from these earlier studies5,6 are prospective and used large samples (N = 725 and N = 1318 respectively), more data is required before reasonable explanations can be devised for the discrepancies reported when self-perceived health as opposed to diagnosed health states, are used as the outcome variable. We would cautiously offer that potentially there may be a set-point where reactivity below this zone is considered adaptive and reactivity above, indicative of dysregulation.
The present investigation could be criticized for using a relatively healthy cohort of university students. However, it should be noted that the sample presented with poorer physical and mental health scores when compared with normative data (SF-36)21 with effect sizes ranging from moderate (i.e., physical health) to high (i.e., mental health). Additionally, it could be argued the sample was well selected as the strongest and most consistent support for the reactivity hypothesis with future blood pressure status is derived from similar youthful samples20.
The use of a non-standardised acute stressor limits the ability to compare our findings with studies that have used the more common Trier Social Stress Test (TSST). However, the use of a mandatory assessed oral presentation (similar to the TSST) as an acute psychological stressor with the student sample before a group of peers (rather than a smaller group of non-peers), may also be viewed as an improvement on laboratory testing with volunteers that may have less meaning and real-world applicability to the participant, a criticism that has been directed at earlier studies22. Nevertheless, individual motivations to perform well may have been a factor and a measure of this information may have contributed to the explanation of the findings attained. Finally, the cross-sectional design prohibited any inference of causality.
These limitations are balanced, however, by several strengths. In particular, we assessed multiple biological indices over stressor and basal conditions and accounted for acute and chronic perceptions of stress. This enabled a fuller depiction of these indices with relation to perceived health than many investigations. Further, we selected a basal period that was 7 days prior to the psychological stressor which limits the influence of the potential confound of anticipatory anxiety on basal physiology. Unlike the previous 2 studies that assessed the reactivity hypothesis with self-reported health5,6, we controlled for the influence of chronic stress on acute stress physiology. Finally, this would appear to be only the third study to assess the reactivity hypothesis with self-perceived health.
Conclusions
The present investigation concluded that the ‘reactivity’ physiological indices were significantly associated with perceived mental health with SBP and sIgA having the strongest associations. Disentangling the physiological pathways that lead to distinct disease states is an important and emerging area of research in this field. While there is much evidence supporting the ability of the SF-36 and reactive physiology to separately predict various disease states, the aim for future researchers will be to determine if the combination of physiological and self-reported information leads to enhanced predictive validity and influences evidence-based stress intervention.
References
Carroll, D., Phillips, A. C., Der, G., Hunt, K. & Benzeval, M. Blood pressure reaction to acute mental stress and blood pressure status: data from the 12-year follow-up of the West of Scotland study. Psychosom Med. 73, 737–742 (2011).
Chida, Y. & Steptoe, A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: a meta-analysis of prospective evidence. Hypertension. 55, 1026–1032 (2010).
Lambert, G., Schlaich, M., Lambert, E., Dawood, T. & Esler, M. Stress reactivity and its association with increased cardiovascular risk: A role for the sympathetic nervous system? Hypertension. 55, 20 (2010).
Myint, P. K. et al. Relation Between Self-Reported Physical Functional Health and Chronic Disease Mortality in Men And Women in the European Prospective Investigation Into Cancer (EPIC–Norfolk): A Prospective Population Study. Ann Epidemiol. 16, 492–500 (2006).
de Rooij, S. R. & Roseboom, T. J. Brief Reports: Further evidence for an association between self-reported health and cardiovascular as well as cortisol reactions to acute psychological stress. Psychophysiology. 47, 1172–1175 (2010).
Phillips, A. C., Der, G. & Carroll, D. Self-reported health and cardiovascular reactions to psychological stress in a large community sample: Cross-sectional and prospective associations. Psychophysiology. 46, 1020–1027 (2009).
Miller, G. E., Chen, E. & Zhou, E. S. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol Bull. 133, 25–45 (2007).
Fraser, R. et al. Cortisol effects on body mass, blood pressure and cholesterol in the general population. Hypertension. 33, 1364–1368 (1999).
Chida, Y. & Hamer, M. Chronic psychosocial factors and acute physiological responses to laboratory-induced stress in healthy populations: a quantitative review of 30 years of investigations. Psych Bull. 134, 829–885 (2008).
Kirschbaum, C. & Hellhammer, D. H. Salivary cortisol in psychobiological research: An overview. Neuropsychobiology 22, 150–69 (1989).
Murphy, L., Denis, R., Ward, C. P. & Tartar, J. L. Academic stress differentially influences perceived stress, salivary cortisol and immunoglobulin-A in undergraduate students. Stress 13, 366–371 (2010).
Woof, J. M. & Kerr, M. A. The function of immunoglobulin A in immunity. J Pathol. 208, 270–82 (2007).
Evans, P. et al. Social class, sex and age differences in mucosal immunity in a large community sample. Brain Behav Immun. 14, 41–48 (2000).
Miletic, I. D., Schiffman, S. S., Miletic, V. D. & Sattely-Miller, E. A. Salivary IgA secretion rate in young and elderly persons. Physiol Behav. 60, 243–248 (1996).
Broderick, J. E., Arnold, D., Kudielka, B. M. & Kirschbaum, C. Salivary cortisol sampling compliance: comparison of patients and healthy volunteers. Psychoneuroendocrinology. 29, 636–650 (2004).
Cohen, S., Kamarck, T. & Mermelstein, R. A global measure of perceived stress. J Health Soc Behav. 24, 385–396 (1983).
Ware, J. E., Kosinski, M. & Keller, S. K. SF-36 Physical and mental health summary scales: A user's manual. 1994; Boston: The Health Institute.
Cohen, J. A power primer. Psych Bull. 112, 155–159 (1992).
Tabachnick, B. G. & Fidell, L. S. Using multivariate statistics. 6th ed.(Pearson Education, Boston, 2013).
Carroll, D., Phillips, A. C. & Der, G. Body mass index, abdominal adiposity, obesity and cardiovascular reactions to psychological stress in a large community sample. Psychosom Med. 70, 653–660 (2008).
Hopman, W. M. et al. Canadian normative data for the SF-36 health survey. Canadian Multicentre Osteoporosis Study Research Group. Can Med Assoc J. 163, 265–271 (2000).
Schwartz, A. R. et al. Toward a causal model of cardiovascular responses to stress and the development of cardiovascular disease. Psychosom Med. 65, 22–35 (2003).
Author information
Authors and Affiliations
Contributions
B.W. designed the study, analysed the data and wrote the first and final draft of this manuscript. S.O.B. collected the data, assisted with ethics application, data analysis and edited the manuscript. A.H. assisted with design, analysis of physiological specimens and editing of the manuscript. S.K. assisted with the design and editing of the manuscript and revisions.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Wright, B., O'Brien, S., Hazi, A. et al. Increased systolic blood pressure reactivity to acute stress is related with better self-reported health. Sci Rep 4, 6882 (2014). https://doi.org/10.1038/srep06882
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep06882
This article is cited by
-
Assessing aerobic physical efficiency through temple surface temperature measurements during light, heavy exercise, and recovery
Scientific Reports (2023)
-
Acute glucose influx-induced mitochondrial hyperpolarization inactivates myosin phosphatase as a novel mechanism of vascular smooth muscle contraction
Cell Death & Disease (2021)
-
Testing the cross-stressor hypothesis under real-world conditions: exercise as a moderator of the association between momentary anxiety and cardiovascular responses
Journal of Behavioral Medicine (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.