Abstract
We investigated 17 polymorphisms in 11 genes (TS, MTHFR, ERCC1, XRCC1, XRCC3, XPD, GSTT1, GSTP1, GSTM1, ABCC1, ABCC2) for their association with the toxicity of fluoropyrimidines and oxaliplatin in colorectal cancer patients enrolled in a prospective randomized trial of adjuvant chemotherapy. The TOSCA Italian adjuvant trial was conducted in high-risk stage II–III colorectal cancer patients treated with 6 or 3 months of either FOLFOX-4 or XELOX adjuvant chemotherapy. In the concomitant ancillary pharmacogenetic study, the primary endpoint was the association of polymorphisms with grade 3–4 CTCAE toxicity events (grade 2–4 for neurotoxicity). In 517 analyzed patients, grade ≥ 3 neutropenia and grade ≥ 2 neurotoxicity events occurred in 150 (29%) and in 132 patients (24.8%), respectively. Diarrhea grade ≥ 3 events occurred in 34 (6.5%) patients. None of the studied polymorphisms showed clinically relevant association with toxicity. Hopefully, genome-wide association studies will identify new and more promising genetic variants to be tested in future studies.
Similar content being viewed by others
Introduction
Adjuvant chemotherapy is the standard of care for stage III colorectal cancer patients and an accepted treatment option for high-risk stage II patients1. Standard regimens include oxaliplatin combined with bolus/infusional 5-fluorouracil (FOLFOX) or capecitabine (XELOX)1. Unfortunately, several patients experience mild or moderate side effects at some point during treatment. Most frequently reported adverse events of these regimens in randomized adjuvant trials in Western populations are neutropenia (≥grade 3 in 40% to 56% of patients), neurotoxicity (≥grade 3 in 10% to 20% of patients) and diarrhea (≥grade 3 in 10% to 15% of patients)2. Therefore, the safety profile may be suboptimal and causing treatment delay, reduction, cessation and even death in a minority of patients. This is very important in the adjuvant setting, where potentially cured patients undergo an effective prophylactic treatment strategy1. Prediction of an individual patients' risk of severe toxicity could allow for an adequate monitoring and improve overall management and quality of care.
Host non-genetic factors such as medical comorbidity and organ dysfunction may account for differences in the safety profile of adjuvant chemotherapy across populations. However, genetic variability among individuals may play a key role3. Functional germline polymorphisms may contribute to inter-individual differences in the pharmacokinetic and pharmacodynamics of anti-cancer drugs and this may contribute to the differences in toxicity among patients3.
In the last decades, some genetic variants involved in the oxaliplatin and the fluoropyrimidines pathways were identified as potential predictors of toxicity4,5. However, the majority of clinical data have been obtained from retrospective analyses including a limited number of patients. In fact, none of the studied polymorphisms showed sufficient evidence for use in clinical practice4,5. Prospective analyses from randomized clinical trial represent a unique opportunity for evaluating association between genetic variants and clinical outcomes and are necessary for confirming the predictive role for toxicity of candidate polymorphisms6,7,8,9.
TOSCA (Three Or Six Colon Adjuvant) is a large randomized trial addressing the role of a shorter duration of an adjuvant oxaliplatin/fluoropyrimidines regimen in surgically resected stage III and high-risk stage II colorectal cancer10. We adopted this clinical trial for planning a robust pharmacogenetic assessment for toxicity focusing on candidate polymorphisms, which had showed promising associations in previous studies6,7,8,11,12,13.
Patients, Materials and Methods
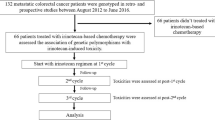
TOSCA trial
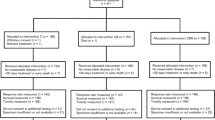
Patients included in this study represent a subgroup of the 3.759 patients with surgically-resected, stage III and high-risk stage II colorectal cancer recruited in TOSCA trial between 2007 and 201110. This is an Italian intergroup, multicentre, randomized, non-inferiority phase III study in high-risk stage II and stage III colon cancer patients treated with 3 or 6 months of either FOLFOX-4 or XELOX adjuvant chemotherapy, sponsored by GISCAD (Italian Group For The Study Of Gastrointestinal Cancer) and supported by Italian Medicines Agency (AIFA)10. Patients eligible for the TOSCA study were asked to give further and specific written informed consent for the pharmacogenetic study. All experiments were performed in accordance with relevant guidelines and regulations and the Local Ethics Committee of each institution approved the Study.
Assessment and management of chemotherapy toxicity
Selected hematologic and non-hematologic toxicities (anemia, leukopenia, neutropenia, thrombocytopenia, asthenia, diarrhea, mucositis stomatitis, vomiting, nausea, hepatic toxicity, skin toxicity, neurotoxicity) were assessed at the start of each cycle using Common Toxicity Criteria for Adverse Events (CTCAE) version 2.0. All adverse events at any time were monitored and reported. Toxicity was managed as follows: in case of grade ≥ 3 hematologic toxicity or persistent grade 2 the dose of all drugs was reduced by 25%. In case of grade ≥ 3 non-hematologic toxicity the dose of the related drugs was reduced by 50%. In case of grade ≥ 3 or persistent grade 2 neurotoxicity, oxaliplatin dose was reduced by 20%. Oxaliplatin was definitely stopped if grade ≥ 2 neurosensory symptoms persisted between cycles.
Molecular assessments
This prospective study was planned as a confirmatory analysis of genetic variants, which had shown some putative predictive effect for toxicity in previous studies6,7,8,11,12,13. Seventeen polymorphisms in eleven genes involved in DNA repair and drug metabolism and as drug targets, were selected from various reports as being potentially predictive of 5-fluorouracil (5-FU) or oxaliplatin toxicity (Table 1) in colorectal cancer patients. For each polymorphism, patients were considered in three groups: homozygous wild type (p2); heterozygous (pq); homozygous variant (q2). We also considered the model with merged heterozygous and homoxygous risk variant carriers.
Blood samples were taken before starting adjuvant chemotherapy. Genomic DNA was extracted by means of QIAmp DNA Blood kit (Qiagen, Valencia, CA). Polymorphisms in TS (rs34743033, rs2853542, rs11280056), XRCC1 (rs25487), XRCC3 (rs861539), XPD (rs1799793, rs13181), GSTT1 (positive or null), GSTM1 (positive or null) were assayed as previously reported11. ABCC1 (rs2074087) and ABCC2 (rs3740066, rs1885301, rs4148386) genetic variants were analyzed using HRM (Rotor-Gene 6000®, Corbett Research, Sydney, Australia) or Pyrosequencing (PSQ 96MA®, Biotage AB) technique according to the manufacturer's instructions. Primer sequences and preparative PCR conditions are reported in the supplementary Table S1. Briefly, all amplification reactions were performed in a volume of 25 ul using 2× PCR Master Mix® (Diatheva, Fano, Italy) kit, 25 ng of gDNA and 200 nM of each primer. The intercalating dye EvaGreen® (Biotium Inc, CA, USA) was added for the HRM analyses. HRM conditions are listed in Table S1. ERCC1 (rs11615), MTHFR (rs1801133, rs1801131) and GSTP1 (rs1695) were genotyped with HRM analyses by means of kits containing reagents, enzymes and genotype controls: ERCC1 Asn118Asn HRM kit, MTHFR C677T HRM kit, MTHFR A1298C HRM kit and GSTP1 Ile105Val HRM kit respectively, according to the manufacturer's instructions (Diatheva). All laboratory analyses were performed blind to the patients' treatment and clinical outcomes. Genetic data were then transferred to IRCCS Istituto di Ricerche Farmacologiche “Mario Negri” for statistical analysis.
Analysis plan, sample size and statistics
According to the planned management of toxicity in TOSCA trial, we chose outcome measures and endpoints, which reflects clinically relevant degrees of both hematologic and non-hematologic toxicity. Primary outcome was defined as the occurrence of a grade 3–4 toxicity (grade 2, 3, 4 for neurotoxicity) considering in each patient the maximum grade of toxicity (MGT) reported during treatment. Secondary outcome was the time to toxicity (TTT), defined as the time from date of randomization in TOSCA trial to the date of first grade ≥ 2 event for neurotoxicity and ≥3 event for other toxicities. Subjects without such a toxicity event at the time of analysis were censored at the date they were last known to be event-free while on treatment.
The treatment compliance was described in terms of treatment interruption and dose intensity, defined as the dose given in mg/m2 per week. Logistic regression and Cox proportional hazard models were used to assess the effects of genotypes on MGT and TTT, respectively, adjusting for treatment duration (6 or 3 months). For each polymorphism, toxicity analysis was performed across the three group genotypes (p2, pq, q2) and after grouping carriers of the heterozygous and homozygous risk genotypes.
Sample size calculation was based on an expected prevalence of at higher risk allele of at least 30% and assuming a 25% risk of toxicity. Accordingly, 440 patients (105 events) would allow the detection of an odds ratio (OR) of at least 2.0 associated to the group with unfavorable genotypes with a power of 90% and a I type error of 5%, for a bilateral test. Deviation from the Hardy-Weinberg equilibrium was assessed using the Pearson χ2 test. Analyses were performed with SAS 9.2 (SAS Institute, Cary, NC). All reported p values are two-sided and confidence intervals (CIs) are at the 95% level. A p value < 0.05 was considered statistically significant.
Results
Patient characteristics and toxicity
From July 2007 to October 2011, 534 patients from 26 experimental centers entered the study. This figure represents 81% of patients randomized in the same period and by the same centers in the main TOSCA trial study. Seventeen patients were not assessable; five patients who were never treated, two patients because of unavailability of treatment data and ten due to technical problems about blood sampling. Therefore, the analysis was conducted on 517 patients.
Characteristics of the 517 patients are shown in Table 2. Patients' baseline characteristics were consistent with those of the whole trial population (data not reported). Most patients were randomized to FOLFOX-4 because option for XELOX regimen was introduced only during the late phase of accrual of this ancillary study. Toxicity caused by adjuvant chemotherapy is reported in Table 3. Again, the spectrum and the frequency of toxicities did not differ from those observed in whole trial population (data on file). The target number of events was reached for neutropenia (150/517 patients, 29%) and neurotoxicity (132/517, 25.5%), only. Dose intensity and treatment interruptions are shown in Table 4 and Table 5, respectively. Dose intensity for patients randomized in 6 months arms is slightly lower than that reported for patients randomized in 3 months arms.
Genetic assessments
Table 1 lists the studied genetic variants and the distribution of genotypes of patients. Consistent with previous observations, genotype frequency did not differ from those observed in Caucasian population. Allele frequencies of all polymorphisms were consistent with the Hardy-Weinberg equilibrium (χ2; p > .05) and with values in the published literature.
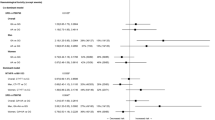
Pharmacogenetics for neutropenia and neurotoxicity
The results of pharmacogenetic analyses in the 517 patients for neutropenia and neurotoxicity are shown in Table 6 and Table 7, respectively. A weak association was observed between the GST-T1/M1null/null genotype (presence of homozygous deletion in both genes) and neutropenia according to MGT (OR 1.99, 95%CI 1.06–3.73; p = 0.03) and TTT (HR 1.70, 95%CI 1.03–2.78; p = 0.04), when compared with wild-type genotype. As far as the ABCC1 rs2074087 genotype and neurotoxicity is concerned, the planned statistical analyses could not be performed due to low model convergence. Regarding neurotoxicity no evidence of association was found between polymorphisms and MGT and TTT.
Other toxicities
Despite the number of events was less than required, therefore decreasing the power of the tests, the analyses showed some statistically significant association. In presence of the ABCC2 (rs 4148386) GG genotype, there was a greater occurrence of grade 3–4 leukopenia (OR 9.82, 95%CI 1.16–83.02; p = 0.036) and the time to leukopenia was shorter (HR 9.40, 95%CI 1.13–78.10; p = 0.038) in comparison to ABCC2AA genotype. TS 3′UTR L allele showed a protective effect for mucositis for MGT (OR 0.07, 95%CI 0.01–0.65; p = 0.020) and TTT (HR 0.07, 95%CI 0.01–0.67; p = 0.021). Risk of vomiting (MGT) was increased in carriers of the TS 5′UTR 2R2R genotype (OR 8.83, 95%CI 1.01–76.91; p = 0.049) compared to TS 5′UTR 3R3R genotype.
Discussion
This study assessed 17 polymorphisms in 11 genes thought to be associated with toxicity of fluoropyrimidines or oxaliplatin. To the best of our knowledge this is the first and the largest prospective pharmacogenetic analysis in a randomized trial of adjuvant chemotherapy in colorectal cancer. Candidate polymorphisms were selected on the basis of previous promising data from retrospective or single arm studies. The prospective accrual of patients achieved the required number of events for neutropenia and neurotoxicity, however only GST-T1/M1 was statistically associated to neutropenia and the strength of this association was very low. Therefore, no polymorphism showed a clinically relevant association with neurotoxicity and neutropenia. The results on the other toxicities should be looked at with caution because of the low number of events.
To date, five randomized clinical trials in colorectal cancer have incorporated pharmacogenetic analysis6,7,8,9, but only one study in the adjuvant setting14. In the US Intergroup N9741 pharmacogenetic analysis there were 114 patients treated with IFL chemotherapy, 299 patients treated with FOLFOX-4 regimen and 107 patients who received IrOX chemotherapy6. Therefore, despite the 520 initial patients assessed for pharmacogenetic analyses, this remarkable study population was diluted among three treatments arms, with a small number of patients assessable for an oxaliplatin-based regimen. In this study, ≥grade 3 neutropenia, neurotoxicity and diarrhea occurred in the 27%, 13% and 13% of patients respectively. In the FOLFOX-4 regimen analysis, the GST-P1 TT genotype carriers were more likely to suffer from febrile neutropenia and to discontinue the treatment because of neurotoxicity, carriers of the GST-M1 null genotype were at increased risk of neutropenia6. In the Fédération Francophone de Cancérologie Digestive 2000-05 trial, metastatic colorectal cancer patients were randomized to receive 5-FU plus leucovorin followed by FOLFOX-6, followed by FOLFIRI (arm A), or FOLFOX-6 followed by FOLFIRI (arm B). The pharmacogenetic analysis included 346 patients who received more regimens in a different sequence7. There was a remarkable frequency of ≥grade 2 neurotoxicity (about half of the patients) and ≥grade 3 myelotoxicity in about one-third of the patients. The XPD C allele (rs13181) was significantly associated with an increased risk of FOLFOX-induced hematologic toxicity (p = 0.01). In the pharmacogenetic analysis associated with the randomized FOCUS UK trial, 1.188 patients were assessed8. In this study, metastatic colorectal cancer patients were randomized to receive three treatment strategies according to a different sequence of the following regimens: 5-FU alone, irinotecan alone, 5-FU with irinotecan and 5-FU with oxaliplatin. Only 280 patients were assessable for first- or second-line oxaliplatin-based chemotherapy. No significant pharmacogenetic association was found in this study8. The most recently published analysis in metastatic colorectal cancer patients depicts the results of a large panel of genetic variants in a robust sample of more than 2,000 patients enrolled in the COIN trials in UK9. Again, this study ruled out clinically relevant associations between pharmacogenetics and clinical outcomes of patients treated with fluoropyrimidine/oxaliplatin with or without cetuximab9.
As far as the adjuvant setting is concerned, the recently published pharmacogenetic study from the QUASAR2 trial has investigated the role of fluoropyrimidine-related polymorphisms in 927 patients who were randomized between capecitabine and capecitabine with bevacizumab. Of the 36 assessed polymorphisms only four TS and DPYD genetic variants were associated with grade ≥ 3 global toxicity, but with modest predictive power14.
Considering the characteristics of the above mentioned studies, we would emphasize the remarkable sample size in the adjuvant setting of our oxaliplatin-based study population, as well as the quality of pharmacogenetic analyses in a prospective and controlled collection of clinical data10. It seems that we recorded a lower frequency of grade ≥ 2 neurotoxicity and grade > 3 neutropenia than previously reported in the literature2. Generally, we observed a global lower incidence of toxicity events than expected. This finding is likely related to the accuracy of physicians in the monitoring of patients with early detection of signs of side-effects and consequently, their conservative attitudes towards treatment delays and dose-reductions.
However, this did not jeopardize the study plan of the ancillary pharmacogenetic study and a sufficient number of events for neurotoxicity and neutropenia was observed. Unfortunately, given the low rate of other severe toxicities, we cannot rule out the risk of observing false-negative associations in these cases.
A number of drug- and host-related variables contribute to pharmacodynamic and pharmacokinetic changes of chemotherapy drugs. Therefore, because of the moderate functional effects of polymorphism in the enzyme/target activity, their clinical impact may be masked according study populations and clinical settings. This may also explain the heterogeneity of results across pharmacogenetic studies. On the whole, we highlight the necessity for large-scale validation trials before pharmacogenetic findings from small studies are incorporated into clinical practice12,13,14,15. In fact, our findings, together with the results of the analyses in metastatic colorectal cancer6,7,8,9 and other malignancies3, mitigate the positive expectations for the routine use of pharmacogenetics. It is a matter of fact that in spite of the growing burden of small, retrospective published studies on the predictive/prognostic role of polymorphisms in colorectal cancer patients, only UDP glucuronosyltransferase 1 family, polypeptide A1 (UGT1A1) and dihydrophyrimidine dehydrogenase (DPYD) genetic variants have shown a promising level of evidence for clinical practice16. However, we did not study the UGT1A1*28 genotype analysis since it is typically associated with Irinotecan pharmacokinetic and toxicity16. As far as the DPYD IVS14 + 1G > A splice mutation is concerned, we did not include this variant for 5-fluorouracil toxicity analysis because of its very low frequency16. In fact, there were 2 heterozygous carriers in the 346 patients (0.5%) of the French trial6, 4 heterozygous carriers in the 520 patients (0.7%) of US trial7 and 12 heterozygous carriers in the 1088 patients (1.1%) of FOCUS trial8.
Pharmacogenetics may still offer a unique opportunity for tailoring the administration of chemotherapy and novel biologic agents to cancer patients. Hopefully, new sophisticated techniques such as SNP arrays and genome-wide association studies (GWAS) will identify new and more promising genetic variants to be tested in future studies17,18.
References
Price, T. J. et al. Current opinion on optimal treatment for colorectal cancer. Expert Rev Anticancer Ther 13, 597–611 (2013).
Sugihara, K. et al. Safety analysis of FOLFOX4 treatment in colorectal cancer patients: a comparison between two Asian studies and four Western studies. Clin Colorectal Cancer 11, 127–37 (2012).
Hertz, D. L. & McLeod, H. L. Use of pharmacogenetics for predicting cancer prognosis and treatment exposure, response and toxicity. J Hum Genet 58, 346–52 (2013).
Deenen, M. J., Cats, A. & Beijnen, J. H. Part 4: pharmacogenetic variability in anticancer pharmacodynamic drug effects. Oncologist 16, 1006–20 (2011).
Deenen, M. J., Cats, A., Beijnen, J. H. & Schellens, J. H. Part 3: Pharmacogenetic variability in phase II anticancer drug metabolism. Oncologist 16, 992–1005 (2011).
McLeod, H. L. et al. Pharmacogenetic predictors of adverse events and response to chemotherapy in metastatic colorectal cancer: results from North American Gastrointestinal Intergroup Trial N9741. J Clin Oncol 28, 3227–33 (2010).
Boige, V. et al. Pharmacogenetic assessment of toxicity and outcome in patients with metastatic colorectal cancer treated with LV5FU2, FOLFOX and FOLFIRI: FFCD 2000-05. J Clin Oncol 28, 2556–64 (2010).
Braun, M. S. et al. Association of molecular markers with toxicityoutcomes in a randomized trial of chemotherapy for advanced colorectal cancer: the FOCUS trial. J Clin Oncol 27, 5519–28 (2009).
Madi, A. et al. Comprehensive pharmacogenetic profiling of advanced colorectal cancer. J Clin Oncol 31, suppl; abstr 3509 (2013).
André, T. et al. The IDEA (International Duration Evaluation of Adjuvant Chemotherapy) Collaboration: Prospective Combined Analysis of Phase III Trials Investigating Duration of Adjuvant Therapy with the FOLFOX (FOLFOX4 or Modified FOLFOX6) or XELOX (3 versus 6 months) Regimen for Patients with Stage III Colon Cancer: Trial Design and Current Status. Curr Colorectal Cancer Rep 9, 261–269 (2013).
Ruzzo, A. et al. Pharmacogenetic profiling in patients with advanced colorectal cancer treated with first-line FOLFOX-4 chemotherapy. J Clin Oncol 25, 1247–54 (2007).
Cecchin, E. et al. A prospective validation pharmacogenomic study in the adjuvant setting of colorectal cancer patients treated with the 5-fluorouracil/leucovorin/oxaliplatin (FOLFOX4) regimen. Pharmacogenomics J 13, 403–9 (2013).
Lee, K. H. et al. Pharmacogenetic analysis of adjuvant FOLFOX for Korean patients with colon cancer. Cancer Chemother Pharmacol 71, 843–51 (2013).
Rosmarin, D. et al. Genetic Markers of Toxicity From Capecitabine and Other Fluorouracil-Based Regimens: Investigation in the QUASAR2 Study, Systematic Review and Meta-Analysis. J Clin Oncol 32, 1031–9 (2014).
Afzal, S. et al. Combinations of polymorphisms in genes involved in the 5-Fluorouracil metabolism pathway are associated with gastrointestinal toxicity in chemotherapy-treated colorectal cancer patients. Clin Cancer Res 17, 3822–9 (2011).
Moen, E. L., Godley, L. A., Zhang, W. & Dolan, M. E. Pharmacogenomics of chemotherapeutic susceptibility and toxicity. Genome Med 4, 90 (2012).
Gillis, N. K., Patel, J. N. & Innocenti, F. Clinical Implementation of Germline Cancer Pharmacogenetic Variants during the Next-Generation Sequencing Era. Clin Pharmacol Ther 95, 269–80 (2013).
Guchelaar, H. J., Gelderblom, H., van der Straaten, T., Schellens, J. H. & Swen, J. J. Pharmacogenetics in the cancer clinic: from candidate gene studies to next-generation sequencing. Clin Pharmacol Ther 95, 383–5 (2014).
Acknowledgements
This work was supported by FanoAteneo, Diatheva srl and POR MARCHE FESR 2007–2013.
Author information
Authors and Affiliations
Contributions
A.R., Francesco G., E.G. and M.M. conceived and performed the study design, performed the manuscript preparation and data interpretation. Fabio G. performed coordination study. Francesca G., I.F., Fabio G. and E.R. performed statistical analysis, data interpretation and manuscript preparation. S.L., M.R., B.M., V.Z., N.P., C.M., R.L., M.T.I., E.V., P.S., S.B., V.R., L.F., M.N., E.B., A.B., D.T., S.L., C.V., F.B., A.S. and L.F., collected samples and patients' data and commented the manuscript. R.L., L.F. and A.S. participated in the study design and data interpretation and helped to draft the manuscript. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Ruzzo, A., Graziano, F., Galli, F. et al. Genetic markers for toxicity of adjuvant oxaliplatin and fluoropyrimidines in the phase III TOSCA trial in high-risk colon cancer patients. Sci Rep 4, 6828 (2014). https://doi.org/10.1038/srep06828
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep06828
This article is cited by
-
Association of DNA repair gene variants with colorectal cancer: risk, toxicity, and survival
BMC Cancer (2020)
-
Is a pharmacogenomic panel useful to estimate the risk of oxaliplatin-related neurotoxicity in colorectal cancer patients?
The Pharmacogenomics Journal (2019)
-
Sex-Related Differences in Impact on Safety of Pharmacogenetic Profile for Colon Cancer Patients Treated with FOLFOX-4 or XELOX Adjuvant Chemotherapy
Scientific Reports (2019)
-
Chemotherapy-induced peripheral neurotoxicity: management informed by pharmacogenetics
Nature Reviews Neurology (2017)
-
Dihydropyrimidine dehydrogenase pharmacogenetics for predicting fluoropyrimidine-related toxicity in the randomised, phase III adjuvant TOSCA trial in high-risk colon cancer patients
British Journal of Cancer (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.