Abstract
A system of self-sustained biological clocks controls the 24-h rhythms of behavioral and physiological processes such as the sleep–wake cycle. The circadian clock system is regulated by transcriptional and translational negative feedback loops of multiple clock genes. Polymorphisms in circadian clock genes have been associated with morningness–eveningness (diurnal) preference, familial advanced sleep phase type (ASPT) and delayed sleep phase type (DSPT). We genotyped single-nucleotide polymorphisms in circadian clock genes in 182 DSPT individuals, 67 free-running type (FRT) individuals and 925 controls. The clock gene polymorphisms were tested for associations with diurnal preference and circadian rhythm sleep disorder (CRSD) phenotypes. The PER3 polymorphism (rs228697) was significantly associated with diurnal preference and the FRT phenotype. The minor allele of rs228697 was more prevalent in evening types than in morning types (sex-adjusted odds ratio (OR), 2.483, Bonferroni-corrected P = 0.012) and in FRT individuals compared with the controls (age- and sex-adjusted OR, 2.021, permutated P = 0.017). Our findings support the notion that PER3 polymorphisms could be a potential genetic marker for an individual's circadian and sleep phenotypes.
Similar content being viewed by others
Introduction
Sleep–wake cycles are regulated by two components, homeostatic drive and circadian drive1. Sleep and wakefulness occur sequentially and sleep propensity increases gradually with extended wakefulness and decreases rapidly during sleep. Sleep propensity is under the control of sleep homeostasis and sleep timing is under the control of circadian clocks. The circadian clock system regulates daily behavioral and physiological rhythms such as body temperature, hormone secretion, blood pressure, metabolism and cognitive performance besides sleep/wakefulness. These rhythms are generated by the central circadian oscillator located in the suprachiasmatic nucleus (SCN) of the hypothalamus and are entrained by environmental cues (e.g., light–dark cycles)2,3. The molecular mechanism of the circadian clock system involves transcription-translation negative feedback loops of multiple clock genes and post-transcriptional and post-translational modification and degradation of clock proteins4,5. The transcription factors BMAL1 and CLOCK form heterodimers, which activate transcription of Cryptochrome (Cry) and Period (Per) by binding to E-box motifs in their promoter regions. CRY and PER proteins gradually accumulate in the cytoplasm. Phosphorylation of CRY and PER is regulated by casein kinase I (CKI). CRY, PER and CKI proteins form complexes that translocate to the nucleus and interact with the BMAL1–CLOCK heterodimers, thereby inhibiting transcription of the Cry and Per genes. Although the circadian function of Timeless (Tim) remains to be determined, Tim is known to modulate neuronal firing rhythms in the SCN6.
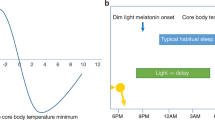
Circadian rhythm sleep disorders (CRSDs) are defined by persistent or recurrent disturbed sleep–wake cycles and comprise several subtypes: advanced sleep phase type (ASPT), delayed sleep phase type (DSPT) and free-running type (FRT). ASPT is characterized by extremely early involuntary sleep timing, DSPT by significantly delayed sleep timing and FRT by sleep timing that occurs with a 30-min to 1-h delay each day. CRSD is thought to result from impairment of the circadian clock system7,8,9. Also, circadian characteristics vary greatly among individuals10,11. The inter-individual differences in daily activity/sleep time are known as morningness–eveningness (diurnal) preference. The morning type manifests earlier timings for sleep and physiological rhythms than the intermediate type and still earlier than the evening type12,13. Individual diurnal preference is morning type during childhood, which subsequently switches to evening type during adolescence before starting to return to morning type in adulthood14,15. Males show evening preference while females show more morning preference, but this gender-related difference disappears in the elderly11,16. The diurnal preference is commonly assessed by self-reported questionnaires, the Horne–Östberg Morningness–Eveningness Questionnaire (MEQ)10 and the recently developed Munich ChronoType Questionnaire (MCTQ)11. The diurnal preference and CRSD phenotypes are thought to be influenced by genetic factors. For example, polymorphisms in the CLOCK, NPAS2, PER2 and TIM genes are associated with diurnal preference17,18, sleep timing19 and sleep disorders20,21,22. Furthermore, the PER3 gene has polymorphisms in the promoter region23, missense polymorphisms that result in amino acid substitution and a variable number tandem repeat (VNTR) consisting of either 4 or 5 repeated 54-bp sequences encoding 18 amino acids (PER34 or PER35)24. These PER3 polymorphisms are associated with diurnal preference and/or DSPT23,24,25. Although the results of some other studies are inconsistent with the associations26,27, a number of genetic studies have shown that genetic factors significantly contribute to individual differences in circadian and sleep phenotypes28,29,30.
Missense mutations in the PER2 and CKIδ genes have been found in large pedigrees with familial ASPT31,32. These amino acid substitutions in PER2 and CKIδ reduce the phosphorylation level of PER2, thereby shortening the intrinsic circadian period (τ) and giving rise to the familial ASPT phenotype. These findings indicate that clock gene polymorphisms, especially missense polymorphisms, may alter the function of these genes, thereby modifying diurnal preference and sleep–wake patterns. To investigate how genetic variations impact circadian and sleep phenotypes, we genotyped single-nucleotide polymorphisms (SNPs) in a number of circadian clock genes in controls and DSPT and FRT patients and tested these SNPs for associations with diurnal preference in controls and in patients with the CRSD phenotype. Our control subjects' diurnal preference was assessed by the Horne–Östberg MEQ10. Age-adjusted MEQ scores of 16–41 denote evening types, 42–58 denote intermediate types and 59–86 denote morning types. The DSPT and FRT patients were diagnosed according to the International Classification of Sleep Disorders 2 (ICSD-2)33.
Results
Association between PER3 and diurnal preference
The 925 controls consisted of 245 morning types (79 men and 166 women; mean ± SD age-adjusted MEQ score: 62.81 ± 3.77), 594 intermediate types (163 men and 431 women; mean ± SD age-adjusted MEQ score: 51.13 ± 4.31) and 86 evening types (32 men and 54 women; mean ± SD age-adjusted MEQ score: 38.23 ± 3.55). Men showed more evening preference than women (χ2 = 9.077, P = 0.011; adjusted residual = ±2.3). The allele frequency of the 9 SNPs in 6 genes was compared among morning, intermediate and evening types (Table 1). As shown in Table 1, only the SNP rs228697 in PER3 was significantly associated with diurnal preference (χ2 = 9.157, P = 0.010). The major allele C of rs228697 was more common in morning types than in evening types and the minor allele G of rs228697 was more common in evening types than in morning types (sex-adjusted odds ratio (OR), 2.483; 95% confidence interval (CI), 1.339–4.603; Bonferroni-corrected P = 0.012; crude P = 0.004). Subjects with the G-positive genotype (CG, GG) for rs228697 showed lower age-adjusted MEQ scores than those with the G-negative genotype (CC) for rs228697 (mean ± SEM age-adjusted MEQ score: 51.70 ± 0.68 vs 53.26 ± 0.29; F(1, 922) = 4.561; P = 0.033).
Association between PER3 and FRT
We then assessed the probability of the 9 SNPs producing DSPT and FRT phenotypes (Table 2). The SNP distributions did not differ between the controls and DSPT individuals. However, the rs228697 distribution significantly differed between controls and FRT individuals. The frequency of the G allele for rs228697 was significantly increased in FRT individuals compared with controls (age- and sex-adjusted OR, 2.021; 95% CI, 1.160–3.524; permutated P = 0.017; crude P = 0.011). The G-positive genotype (CG, GG) for rs228697 was more prevalent in FRT individuals (CG, GG, 0.284) than in controls (CG, GG, 0.154) with an age- and sex-adjusted OR of 2.253 (95% CI, 1.233–4.118; P = 0.008). Therefore, the PER3 SNP rs228697 was significantly associated with the FRT phenotype in this cohort.
Discussion
We found that the G allele of rs228697 in PER3 was more common in evening types than in morning types and in FRT individuals than in controls using a very large sample of control individuals and CRSD patients. These findings are in accordance with previous reports23,24,25 suggesting genetic associations between PER3 polymorphisms and diurnal preference and/or CRSD phenotypes. A PER3 haplotype defined by the G allele of rs10462020 and the C allele of rs10462021 has been shown to be related to DSPT24. Furthermore, the 4-repeat allele of PER3 VNTR (PER34) has been associated with extreme evening preference and DSPT, whereas the 5-repeat allele of PER3 VNTR (PER35) has been associated with extreme morning preference25. In addition, the polymorphisms in the PER3 promoter have been associated with DSPT23. Although the SNPs rs10462020 and rs10462021 were excluded from further analysis due to the low minor allele frequency (MAF) < 0.05 and the PER34 and PER35 alleles as well as the previously described polymorphisms in the PER3 promoter, were not directly investigated in this study, the present and previous findings strongly suggest that PER3 polymorphisms can provide potential biomarkers for estimating individual diurnal preference and CRSD phenotypes.
Morning types and evening types have been reported to differ in homeostatic sleep regulation and neurobehavioral functions in response to sleep fragmentation and sleep deprivation29. Mongrain et al. have demonstrated that the morning type exhibits a higher initial level and faster dissipation rate of sleep pressure than the evening type34. These results suggest that diurnal preference may reflect individual differences in both homeostatic and circadian regulation. Moreover, there are inter-individual differences in the impairment of neurobehavioral functions (attention, decision making, etc.) in response to sleep deprivation and sleep restriction35,36,37. A number of studies indicate that genetic traits contribute to individual differences in sleep homeostasis, circadian rhythms and cognitive performance28,38. Individuals homozygous for PER35 demonstrate more morning preference, greater sleep propensity at baseline and after sleep deprivation and a lower level of cognitive performance than those homozygous for PER3439,40. The results of our previous study have implied that an altered expression profile of PER3 may reflect deteriorated homeostatic sleep drive in the elderly41. Additionally, Archer et al. have reported that the polymorphisms in the PER3 promoter are associated with DSPT and that these polymorphisms have an effect on its expression level23. The data reported here showed that the PER3 SNP rs228697 was associated with diurnal preference and FRT phenotype in our large sample of CRSD patients and controls. These findings suggest that the PER3 gene may play a functional role in homeostatic sleep and/or circadian clock systems. Furthermore, PER3 polymorphisms may predict individual differences in vulnerability to sleep deprivation and restriction.
The SNP rs228697 (C/G) corresponds to the SNP in exon 17 of the PER3 gene and causes the amino acid substitution (P864A)24. Although the amino acid substitution of proline (P) to alanine (A) does not make a significant difference to polarity or hydrophobicity, the amino acids P and A differ in their hydropathy index. Accordingly, the P/A substitution could alter the secondary structure and/or phosphorylation status of PER3 leading to dysregulation of the homeostatic sleep and circadian clock systems. It is intriguing that P864A is located in potential Src homology (SH)3 domains in PER3. SH3 domains are found in many proteins in an array of signaling pathways that regulate the cytoskeleton, the Ras gene family and the Src kinase family, as well as many other signaling cascades42,43. The proline-rich motif X-P-X-X-P is defined as the minimal consensus sequence of the SH3-binding sites. X is often an aliphatic amino acid44. The P864A substitution would disrupt two potential SH3-binding motif domains in PER3 (LPDPP(864) and PP(864)VCP), which could alter the binding interaction between PER3 and its partner protein(s), thereby disturbing the function of PER3 in the homeostatic and circadian regulation of sleep. CKI interacts with the scaffolding protein NCK that consists of SH2 and SH3 domains45. As CKI is known to regulate PER protein stability46,47, it is interesting to speculate that the interaction between CKI and PER3 may be partially mediated via the scaffolding afforded by the interactions between the SH3 domain in NCK and the putative SH3 ligand in PER3. However, how this allelic variation of PER3 modifies sleep and circadian phenotypes remains to be determined.
FRT is defined by sleep timing that occurs with a 30-min to 1-h delay each day. Therefore, prolongation of τ has been considered a critical factor for determining the FRT phenotype7,8,9. Free-running patterns in sleep–wake cycles are often observed in blind individuals48. Because totally blind individuals are not capable of perceiving photic signals, some may show free-running sleep patterns as a consequence of the loss of photic entrainment. Thus, the pathophysiology of sighted individuals with FRT might also be associated with an impaired photic entrainment mechanism as well as with prolonged τ. We recently reported that sighted FRT patients have a longer τ than intermediate types, but not when compared with evening types49. Moreover, the results of the present study demonstrate that extreme evening preference and FRT are associated with the same polymorphism in the PER3 gene. Based upon these findings, there may be a genetic trait or traits shared by individuals with extreme evening preference and FRT phenotypes. In contrast, DSPT was not associated with any polymorphisms in the PER3 gene or other clock genes investigated in this study. It appears likely that this results from the heterogeneity of the DSPT population. Not only circadian clock defects, but also psychiatric problems and/or consequent reduction of social (non-photic) entrainment are thought to be causative factors for the development of DSPT phenotypes50.
There are some limitations to this study. It would be difficult to conduct a replication study using another sample of patients due to the extremely low prevalence of CRSDs in the Japanese population (0.13%)51. Other groups have shown associations of PER3 and diurnal preference and/or CRSD phenotypes using their samples23,24,25. We did not control for medical treatments in our subjects, such as medication and light therapy, although these treatments would only alter the medical condition of patients and not their diagnoses.
In conclusion, our findings corroborate the involvement of PER3 in regulating the homeostatic sleep and/or circadian systems. The PER3 gene has the potential to serve as a biomarker for evaluating genetic traits of sleep and circadian phenotypes and as a research target to understand the mechanism underling the pathophysiology of FRT. Life styles have dramatically changed during the past century. Shift work and jet lag induce acute sleep deprivation and chronic sleep restriction, which is associated with deteriorated neurobehavioral performance35,52. Furthermore, a misalignment between endogenous circadian rhythms and sleep–wake cycles known as internal desynchronization is thought to cause sleep shortage and circadian rhythm disturbance, leading to elevated risks for autonomic disorders, cardiovascular diseases, metabolic diseases and mood disorders53,54,55. Therefore, predicting sleep and circadian phenotypes may help develop interventions to improve quality of life and potentially prevent various diseases.
Methods
Subjects
The study population consisted of 182 DSPT individuals (111 men and 71 women; mean ± SD age: 26.68 ± 9.25 years), 67 FRT individuals (48 men and 19 women; mean ± SD age: 26.72 ± 9.79 years) and 925 controls (274 men and 651 women; mean ± SD age: 36.45 ± 12.10 years). Patient subjects and controls were all unrelated, sighted Japanese men and women who were recruited at medical and research institutes on mainland Japan. None of the controls had a history of sleep disorders or psychosis. The DSPT and FRT patients were diagnosed by trained psychiatrists according to the International Classification of Sleep Disorders II (ICSD-II, 1990, 1997)33. The diagnostic criteria for DSPT are (1) inability to fall asleep and wake up spontaneously at the desired time; (2) persistent delayed phase of the major sleep episode in relation to the desired time for sleep; (3) symptoms present for at least 1 month; and (4) sleep of normal quality and duration when not required to maintain a conventional sleep–wake schedule. The criteria for FRT are (1) insomnia or excessive sleepiness related to misalignment between the endogenous circadian rhythm and the 24-h light–dark cycle; (2) chronic sleep–wake cycle with a longer period than 24 h; and (3) symptoms present for at least 1 month. Ten DSPT patients had comorbidities as follows: bipolar, one; major depression, three; pervasive developmental disorder, two; seasonal affective disorder, two; sleep apnea syndrome, two. Seventeen FRT patients had comorbidities as follows: bipolar, one; major depression, one; seasonal affective disorder, one. The protocol was approved by the respective institutional ethical review boards. All subjects provided written informed consents. The present study was conducted according to the principles of the Declaration of Helsinki.
Markers and genotyping
A total of 30 SNPs in 7 genes, CLOCK, CRY2, NPAS2, PER1, PER2, PER3 and TIM, were selected (Table 3). These genes have been previously validated in some populations (http://www.ncbi.nlm.nih.gov/snp/). Overall, 28 SNPs resulted in amino acid substitutions and 2 SNPs, rs1801260 and rs2304672, were in the 5′ UTR of CLOCK and PER2, respectively. The SNP rs1801260 was associated with evening preference in a Japanese population18 and rs2304672 was found in a Japanese pedigree of familial ASPT21. Thirty SNPs including rs1801260 and rs2304672 were genotyped in 925 Japanese controls. The Hardy–Weinberg equilibrium (HWE) was tested for each marker. The SNPs showing monomorphism with low frequency (MAF < 0.05) or not in HWE (P < 0.05) were excluded from further analysis. Therefore, 9 SNPs in 6 genes, CLOCK, NPAS2, PER1, PER2, PER3 and TIM, were genotyped in 249 CRSD individuals.
Blood samples were collected from all subjects and used for DNA isolation. Genomic DNA was extracted from leukocytes with the QIAamp DNA Blood Midi Kit (QIAGEN K.K., Tokyo, Japan). Genotyping was performed by a TaqMan SNP Genotyping assay (Applied Biosystems, Foster City, CA) according to the manufacturer's instructions. The genotyping assay IDs for 27 SNPs are listed in Table 3 and the primers and TaqMan probes for rs2640909, rs35802556 and rs10462021 are listed in Table 4.
Self-assessment
The Japanese version of the Horne–Östberg MEQ10 was administered to assess subjects' diurnal preference; this tool has been validated in a Japanese population56. Because diurnal preference changes with age, MEQ scores were adjusted by age (age-adjusted MEQ score, MEQ score + 0.3512 × (39.212 − age))57. Age-adjusted MEQ scores of 16–41 denote evening types, 42–58 denote intermediate types and 59–86 denote morning types. Thus, lower MEQ scores indicate evening preference.
Statistical analysis
HWE was estimated using Haploview 4.1 (http://www.broad.mit.edu/mpg/haploview/)58. The chi-squared test was performed to compare the allele frequency and genotype distribution for each SNP marker among diurnal preference groups (morning, intermediate and evening types). The sex-adjusted ORs and 95% CIs with Bonferroni correction were calculated to evaluate the rs228697 frequency across the three diurnal preference groups. One-way analysis of variance adjusted for sex was performed to compare age-adjusted MEQ scores between subjects with genotype CG or GG for rs228697 and those with genotype CC for rs228697. The chi-squared and permutation tests (N = 10,000) were performed to evaluate the difference in allele frequency between patients (DSPT or FRT) and controls using Haploview 4.1. The age- and sex-adjusted ORs and 95% CIs were calculated to evaluate the rs228697 frequency between FRT patients and controls. P < 0.05 was considered to be statistically significant. Statistical analysis was performed using SPSS ver.11.5.1J (SPSS Japan Inc., Tokyo, Japan), unless otherwise stated.
References
Daan, S., Beersma, D. G. & Borbely, A. A. Timing of human sleep: recovery process gated by a circadian pacemaker. Am J Physiol 246, R161–183 (1984).
Yamazaki, S. et al. Resetting central and peripheral circadian oscillators in transgenic rats. Science 288, 682–685 (2000).
Yoo, S. H. et al. PERIOD2::LUCIFERASE real-time reporting of circadian dynamics reveals persistent circadian oscillations in mouse peripheral tissues. Proc Natl Acad Sci U S A 101, 5339–5346 (2004).
Reppert, S. M. & Weaver, D. R. Coordination of circadian timing in mammals. Nature 418, 935–941 (2002).
Lowrey, P. L. & Takahashi, J. S. Genetics of circadian rhythms in Mammalian model organisms. Adv Genet 74, 175–230 (2011).
Barnes, J. W. et al. Requirement of mammalian Timeless for circadian rhythmicity. Science 302, 439–442 (2003).
Okawa, M. & Uchiyama, M. Circadian rhythm sleep disorders: characteristics and entrainment pathology in delayed sleep phase and non-24-h sleep-wake syndrome. Sleep Med Rev 11, 485–496 (2007).
Ebisawa, T. Analysis of the molecular pathophysiology of sleep disorders relevant to a disturbed biological clock. Mol Genet Genomics 288, 185–193 (2013).
Hida, A., Kitamura, S. & Mishima, K. Pathophysiology and pathogenesis of circadian rhythm sleep disorders. J Physiol Anthropol 31, 7 (2012).
Horne, J. A. & Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol 4, 97–110 (1976).
Roenneberg, T., Wirz-Justice, A. & Merrow, M. Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythms 18, 80–90 (2003).
Duffy, J. F., Dijk, D. J., Hall, E. F. & Czeisler, C. A. Relationship of endogenous circadian melatonin and temperature rhythms to self-reported preference for morning or evening activity in young and older people. J Invest Med 47, 141–150 (1999).
Baehr, E. K., Revelle, W. & Eastman, C. I. Individual differences in the phase and amplitude of the human circadian temperature rhythm: with an emphasis on morningness-eveningness. J Sleep Res 9, 117–127 (2000).
Carskadon, M. A., Wolfson, A. R., Acebo, C., Tzischinsky, O. & Seifer, R. Adolescent sleep patterns, circadian timing and sleepiness at a transition to early school days. Sleep 21, 871–881 (1998).
Roenneberg, T. et al. A marker for the end of adolescence. Curr Biol 14, R1038–1039 (2004).
Adan, A. & Natale, V. Gender differences in morningness-eveningness preference. Chronobiol Int 19, 709–720 (2002).
Katzenberg, D. et al. A CLOCK polymorphism associated with human diurnal preference. Sleep 21, 569–576 (1998).
Mishima, K., Tozawa, T., Satoh, K., Saitoh, H. & Mishima, Y. The 3111T/C polymorphism of hClock is associated with evening preference and delayed sleep timing in a Japanese population sample. Am J Med Genet B Neuropsychiatr Genet 133B, 101–104 (2005).
Gamble, K. L. et al. Shift work in nurses: contribution of phenotypes and genotypes to adaptation. PLoS One 6, e18395 (2011).
Iwase, T. et al. Mutation screening of the human Clock gene in circadian rhythm sleep disorders. Psychiatry Res 109, 121–128 (2002).
Satoh, K., Mishima, K., Inoue, Y., Ebisawa, T. & Shimizu, T. Two pedigrees of familial advanced sleep phase syndrome in Japan. Sleep 26, 416–417 (2003).
Serretti, A. et al. Insomnia improvement during antidepressant treatment and CLOCK gene polymorphism. Am J Med Genet B Neuropsychiatr Genet 137B, 36–39 (2005).
Archer, S. N. et al. Polymorphism in the PER3 promoter associates with diurnal preference and delayed sleep phase disorder. Sleep 33, 695–701 (2010).
Ebisawa, T. et al. Association of structural polymorphisms in the human period3 gene with delayed sleep phase syndrome. EMBO Reports 2, 342–346 (2001).
Archer, S. N. et al. A length polymorphism in the circadian clock gene Per3 is linked to delayed sleep phase syndrome and extreme diurnal preference. Sleep 26, 413–415 (2003).
Robilliard, D. L. et al. The 3111 Clock gene polymorphism is not associated with sleep and circadian rhythmicity in phenotypically characterized human subjects. J Sleep Res 11, 305–312 (2002).
Osland, T. M., Bjorvatn, B. R., Steen, V. M. & Pallesen, S. Association study of a variable-number tandem repeat polymorphism in the clock gene PERIOD3 and chronotype in Norwegian university students. Chronobiol Int 28, 764–770 (2011).
Takahashi, J. S., Hong, H. K., Ko, C. H. & McDearmon, E. L. The genetics of mammalian circadian order and disorder: implications for physiology and disease. Nature Rev Genet 9, 764–775 (2008).
Goel, N., Basner, M., Rao, H. & Dinges, D. F. Circadian rhythms, sleep deprivation and human performance. Prog Mol Biol Transl Sci 119, 155–190 (2013).
Barclay, N. L. & Gregory, A. M. Quantitative genetic research on sleep: a review of normal sleep, sleep disturbances and associated emotional, behavioural and health-related difficulties. Sleep Med Rev 17, 29–40 (2013).
Toh, K. L. et al. An hPer2 phosphorylation site mutation in familial advanced sleep phase syndrome. Science 291, 1040–1043 (2001).
Xu, Y. et al. Functional consequences of a CKIdelta mutation causing familial advanced sleep phase syndrome. Nature 434, 640–644 (2005).
American Academy of Sleep Medicine. ICSD-2. The International Classification of Sleep Disorders 2nd ed.: Diagnostic and Coding Manual, (Westchester, IL, 2005).
Mongrain, V., Carrier, J. & Dumont, M. Circadian and homeostatic sleep regulation in morningness-eveningness. J Sleep Res 15, 162–166 (2006).
King, A. C., Belenky, G. & Van Dongen, H. P. Performance impairment consequent to sleep loss: determinants of resistance and susceptibility. Curr Opin Pulm Med 15, 559–564 (2009).
Van Dongen, H. P., Baynard, M. D., Maislin, G. & Dinges, D. F. Systematic interindividual differences in neurobehavioral impairment from sleep loss: evidence of trait-like differential vulnerability. Sleep 27, 423–433 (2004).
Van Dongen, H. P., Maislin, G. & Dinges, D. F. Dealing with inter-individual differences in the temporal dynamics of fatigue and performance: importance and techniques. Aviat Space Environ Med 75, A147–154 (2004).
Goel, N. Genetics of Sleep Timing, Duration and Homeostasis in Humans. Sleep Med Clin 6, 171–182 (2011).
Viola, A. U. et al. PER3 polymorphism predicts sleep structure and waking performance. Curr Biol 17, 613–618 (2007).
Maire, M. et al. Sleep ability mediates individual differences in the vulnerability to sleep loss: Evidence from a PER3 polymorphism. Cortex 52, 47–59 (2014).
Hida, A. et al. Expression profiles of PERIOD1, 2 and 3 in peripheral blood mononuclear cells from older subjects. Life Sci 84, 33–37 (2009).
Pawson, T. & Schlessingert, J. SH2 and SH3 domains. Curr Biol 3, 434–442 (1993).
Pawson, T. Protein modules and signalling networks. Nature 373, 573–580 (1995).
Alexandropoulos, K., Cheng, G. & Baltimore, D. Proline-rich sequences that bind to Src homology 3 domains with individual specificities. Proc Natl Acad Sci U S A 92, 3110–3114 (1995).
Lussier, G. & Larose, L. A casein kinase I activity is constitutively associated with Nck. J Biol Chem 272, 2688–2694 (1997).
Akashi, M., Tsuchiya, Y., Yoshino, T. & Nishida, E. Control of intracellular dynamics of mammalian period proteins by casein kinase I epsilon (CKIepsilon) and CKIdelta in cultured cells. Mol Cell Biol 22, 1693–1703 (2002).
Shirogane, T., Jin, J., Ang, X. L. & Harper, J. W. SCFbeta-TRCP controls clock-dependent transcription via casein kinase 1-dependent degradation of the mammalian period-1 (Per1) protein. J Biol Chem 280, 26863–26872 (2005).
Lockley, S. W. et al. Relationship between melatonin rhythms and visual loss in the blind. J Clin Endocrinol Metab 82, 3763–3770 (1997).
Kitamura, S. et al. Intrinsic circadian period of sighted patients with circadian rhythm sleep disorder, free-running type. Biol Psychiatry 73, 63–69 (2013).
Shirayama, M. et al. The psychological aspects of patients with delayed sleep phase syndrome (DSPS). Sleep Med 4, 427–433 (2003).
Yazaki, M., Shirakawa, S., Okawa, M. & Takahashi, K. Demography of sleep disturbances associated with circadian rhythm disorders in Japan. Psychiatry Clin Neurosci 53, 267–268 (1999).
Van Dongen, H. P., Maislin, G., Mullington, J. M. & Dinges, D. F. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep 26, 117–126 (2003).
Dinges, D. F. et al. Cumulative sleepiness, mood disturbance and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep 20, 267–277 (1997).
Scheer, F. A., Hilton, M. F., Mantzoros, C. S. & Shea, S. A. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A 106, 4453–4458 (2009).
Puttonen, S., Harma, M. & Hublin, C. Shift work and cardiovascular disease - pathways from circadian stress to morbidity. Scand J Work, Environ Health 36, 96–108 (2010).
Ishihara, K., Saitoh, T., Inoue, Y. & Miyata, Y. Validity of the Japanese version of the Morningness-Eveningness Questionnaire. Percept and Motor Skills 59, 863–866 (1984).
Hida, A. et al. Individual traits and environmental factors influencing sleep timing: a study of 225 Japanese couples. Chronobiol Int 29, 220–226 (2012).
Barrett, J. C., Fry, B., Maller, J. & Daly, M. J. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21, 263–265 (2005).
Acknowledgements
We thank Kentaro Nozaki, Naoko Ayabe, Chihaya Osawa and Keiko Hiyama for their assistance. Part of this study is the result of “Understanding of Molecular and Environmental Bases for Brain Health” carried out under the Strategic Research Program for Brain Sciences from the Ministry of Education, Culture, Sports, Science and Technology of Japan. This study was supported by Grants-in-Aid for Scientific Research (#21390335, #22791161 and #24621015) from the Japan Society for the Promotion of Science, an Intramural Research Grant (#23-3) for Neurological and Psychiatric Disorders from the National Center of Neurology and Psychiatry and a grant from the Takeda Research Foundation.
Author information
Authors and Affiliations
Contributions
A.H. and K.M. designed the research. A.H., S.K., Y.K., M.K., H.O., H.K., M.U., T.E., Y.I., Y.K., M.O., K.T. and K.M. performed the research. A.H., S.K., M.K. and H.O. analyzed the data. A.H. and K.M. wrote the manuscript. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Hida, A., Kitamura, S., Katayose, Y. et al. Screening of Clock Gene Polymorphisms Demonstrates Association of a PER3 Polymorphism with Morningness–Eveningness Preference and Circadian Rhythm Sleep Disorder. Sci Rep 4, 6309 (2014). https://doi.org/10.1038/srep06309
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep06309
This article is cited by
-
Machine learning and expression analyses reveal circadian clock features predictive of anxiety
Scientific Reports (2022)
-
The interindividual variability of sleep timing and circadian phase in humans is influenced by daytime and evening light conditions
Scientific Reports (2021)
-
A missense variant in PER2 is associated with delayed sleep–wake phase disorder in a Japanese population
Journal of Human Genetics (2019)
-
Site-specific hourly resolution wet bulb globe temperature reconstruction from gridded daily resolution climate variables for planning climate change adaptation measures
International Journal of Biometeorology (2019)
-
Genetic association of human Corticotropin-Releasing Hormone Receptor 1 (CRHR1) with Internet gaming addiction in Korean male adolescents
BMC Psychiatry (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.