Abstract
In vitro studies have shown that hydrogen peroxide (H2O2) produced by high-concentration ascorbate and cell culture medium iron efficiently kills cancer cells. This provided the rationale for clinical trials of high-dose intravenous ascorbate-based treatment for cancer. A drawback in all the in vitro studies was their failure to take into account the in vivo concentration of iron to supplement cell culture media which are characterized by low iron content. Here we showed, using two prostate cancer cell lines (LNCaP and PC-3) and primary astrocytes, that the anticancer/cytotoxic effects of ascorbate are completely abolished by iron at physiological concentrations in cell culture medium and human plasma. A detailed examination of mechanisms showed that iron at physiological concentrations promotes both production and decomposition of H2O2. The latter is mediated by Fenton reaction and prevents H2O2 accumulation. The hydroxyl radical, which is produced in the Fenton reaction, is buffered by extracellular proteins and could not affect intracellular targets like H2O2. These findings show that anticancer effects of ascorbate have been significantly overestimated in previous in vitro studies and that common cell culture media might be unsuitable for redox research.
Similar content being viewed by others
Introduction
A number of finished (phase I) and still ongoing clinical trials have examined the possible benefits of intravenous ascorbate (Asc) therapy in cancer treatment. High pharmacological concentrations of Asc in the blood (approximately 5–10 mM range) are achievable only by intravenous application and appear to be safe and tolerated1,2,3. The key pre-clinical rationale for such trials is found in consistent results from more than 20 in vitro studies which concluded that pharmacological Asc efficiently kills over 50 cancer cell lines, leaving most of the examined primary (normal) cell types unaffected4,5. Furthermore, the mechanisms of Asc's anticancer activity were described by Chen and co-workers6 and later confirmed by others7,8, showing that Asc is a pro-drug for extracellular generation of hydrogen peroxide (H2O2) and that iron is essential for H2O2 production. In brief, Asc reduces iron (Fe3+ to Fe2+), which further reacts with molecular oxygen forming the superoxide radical anion. Superoxide undergoes (non)enzymatic dismutation to produce H2O2. Supra-physiological concentrations of H2O2 enter the cell and exert cytotoxic effects. Both apoptotic and necrotic pathways of cell death were implicated, with necrosis more prevalent at increasing Asc doses4.
A careful inspection of all the available reports regarding the anticancer effects of Asc reveals a systematic omission. Namely, there is not a single study of the four-component system (Asc, iron, molecular oxygen and cancer cell lines) that has examined the effects of different concentrations of iron. All the in vitro studies in question have been conducted using commercial cell culture media, usually RPMI-1640 or DMEM supplemented with 10% (v/v) foetal calf serum (FCS). While DMEM contains only 0.25 μM ferric nitrate (Sigma-Aldrich formulation), iron is not a regular component of RPMI-1640 but probably exists via impurities. Concentrations of iron in FCS are not consistent and vary between manufacturers and batches [usually 2–5 μM in 10% (v/v) FCS]. In one particular study, the concentration of iron in 10% (v/v) FCS was 4.2 ± 1.1 μM9, while another group found ~3 μM Fe in RPMI-1640 with 10% (v/v) FCS10. One peculiar detail is that iron chelators have been used in some studies in order to examine the effects of sequestration of (an unknown amount of) iron on Asc cytotoxicity5. The key drawback in all the studies is that the concentration of iron was not altered, measured or taken into consideration whatsoever.
The fundamental problem behind the drawback lays in the fact that physiological milieus of interest (human plasma and interstitial fluid) contain much more iron compared to cell culture media. Total concentration of iron in plasma is in the range of 10–30 μM11 and even higher in cancer patients12,13, as well as in patients receiving chemotherapy14. The concentration of iron in interstitial fluid (outside the CNS) closely mirrors that found in the plasma11,15, whereas iron appears to accumulate in tumour interstitial fluid16. In addition, Asc may provoke the release of iron from extracellular stores, such as ferritin which could be actively produced and released by cancer cells7. It is important to point out that although plasma and interstitial fluid share very similar redox properties17, the critical in vivo accumulation of H2O2 could take place only in interstitial fluid, as catalase (CAT)-rich erythrocytes buffer H2O2 in the blood. The lack of studies that address the effects of iron at (patho)physiological concentrations is rather perplexing, particularly if we take into account previous findings showing that iron can protect cancer cells from H2O218.
Herein we study the anticancer/cytotoxic activity of Asc under conditions that reflect in vivo settings: (i) in cell culture medium with (supplemented) iron at concentrations that are comparable to those in plasma and interstitial fluid; (ii) in human plasma; and (iii) using tumour spheroid model that mimics biological properties of micro-metastases. We use two human prostate cancer cell lines – LNCaP (low metastatic potential, androgen-dependent) and PC-3 (high metastatic potential, androgen-independent), as well as primary astrocytes. Astrocytes were selected for comparison with cancer cells because they are: (i) ontogenetically different (ectodermal origin) compared to prostate cells (endodermal origin): (ii) acquired from a different species; and (iii) susceptible to Asc cytotoxicity19. Biochemical assays, oximetry, electron paramagnetic resonance (EPR) spectroscopy and immunofluorescence are employed in order to elucidate the interactions between Asc and iron.
Results
Total concentration of iron in the cell culture medium applied to maintain cells (RPMI-1640 + 10% FCS) was 5.6 ± 1.3 μM. This is considerably lower compared to the iron concentration in plasma (18.4 ± 5.9 μM; p < 0.001). The level of iron in the plasma of six volunteers ranged between 12–28 μM (Supplementary Table S1). Incubation with pharmacological Asc (5 and 10 mM) in cell culture medium resulted in a drastic decrease (~80%) in the number of viable LNCaP and PC-3 cells (Fig. 1a, b). The cell culture medium was then supplemented with iron in the form of ferric ammonium citrate (FAC), in order to mimic the level of iron in plasma/interstitial fluid. The concentrations of supplemented iron were 5, 10, 15 and 30 μM, resulting in the total iron concentrations of approximately 10, 15, 20 and 35 μM (~5 μM already found in the medium + supplemented iron). The addition of iron at a concentration as low as 5 μM (resulting in a lower physiological limit for iron level), annihilated the cytotoxic effects of Asc. All other iron concentrations inhibited the cytotoxic effects of Asc as well. Additional experiments using FeCl3 were performed in order to eliminate the possibility that the observed effects are mediated by FAC and not by iron per se. Ferric chloride completely inhibited the cytotoxic effects of Asc (data not shown). It should be pointed out that iron at physiological concentrations provided protection irrespective of metastatic potential of the two cell lines. A similar experiment was performed on primary astrocytes. Fig. 1c shows that the supplementation of iron also alleviated the cytotoxic effects of Asc on non-cancer cells. Finally, Asc had very little effect on cancer cell viability in human plasma (Fig. 1d). Only a slight decrease in viability was found for LNCaP cells exposed to 10 mM Asc. Supplementary Table S1 shows the results of viability tests for each of 6 plasma samples. Asc (10 mM) provoked a slight decrease of viability of LNCaP cells only in some plasma samples. Of note, no CAT activity could be detected in the plasma using two different assays. This is in line with previous notions that plasma contains no (or very little) CAT20,21. Further, we modified the level of iron in cell culture medium by increasing the volume percent concentration of FCS, where 10% (v/v) increase add ~5 μM to the total iron concentration. It can be observed that cytotoxic effects of Asc were gradually alleviated with increasing FCS percentage (Fig. 1e, f).
Effects of pharmacological ascorbate and physiological iron on the viability of cancer and primary cells according to MTT and CV assays.
(a) LNCaP and (b) PC-3 cells treated in cell culture medium (RPMI-1640 + 10% FCS) with different concentrations of supplemented iron; * - statistically significant (p < 0.05) compared to control with the same amount of supplemented iron. (c) Primary astrocytes treated with Asc (5 mM) and/or iron (30 μM) in cell culture medium. (d) LNCaP (left) and PC-3 (right) in human plasma; Bars not sharing a common letter are significantly different (p < 0.05). (e) LNCaP and (f) PC-3 cells treated in cell culture medium with different % (v/v) of FCS; Bars not sharing a common letter are significantly different (p < 0.05); * - non-significant compared to control with the same % (v/v) of FCS. Statistical analysis was performed using one-way or two-way ANOVA with post hoc Duncan test.
A set of experiments was performed in order to elucidate the mechanisms of iron's cytoprotective activity. Increased ascorbyl radical production (Fig. 2a) and O2 consumption (Fig. 2b) imply that the generation of H2O2 is higher in the presence of iron at physiological concentration compared to cell culture medium iron. Ascorbyl radical is a by-product of Asc-mediated reduction of iron (Fe3+ to Fe2+) and represents a marker of H2O2 production in this system22. The level of H2O2 was estimated by the addition of CAT which resulted in a rapid and transient O2 production from H2O2 breakdown (Fig. 2b). The amount of O2 produced and the rate of O2 production were much smaller/lower in the presence of iron at physiological concentration, compared to the system with cell culture medium concentration of iron. If we take into account that CAT uses two H2O2 molecules for each O2 produced (2H2O2 → 2H2O + O2), the steady-state concentration of H2O2 in the presence of cell culture medium iron is estimated to be around 25 μM. Physiological iron reduced the level of H2O2 to 1.5 μM. This is in contrast to the amount of O2 that was consumed in these systems prior to CAT addition. Further, it can be observed that CAT almost fully restored the level of O2 in the system with cell culture medium concentration of iron. This is not true for physiological iron, implying the production of end-product(s) other than H2O2. Ascorbyl radical is produced in the plasma supplemented with Asc (Fig. 2c), implying that Asc is redox active and that H2O2 is produced in this system. Ascorbyl radical concentrations found in our experiments correspond to levels in the plasma of cancer patients receiving Asc intravenously23. Polarographic measurements on plasma resemble data obtained on cell culture medium with physiological concentration of Fe. Only traces of H2O2 could be detected in plasma supplemented with Asc (Fig. 2d). Altogether these results show that in the presence of pharmacological Asc, physiological Fe promotes H2O2 decomposition, thus not allowing H2O2 accumulation. In the presence of cell culture medium concentration of iron, H2O2 accumulates because its degradation is very slow or completely absent.
The effects of ascorbate and iron on hydrogen peroxide production in cell culture medium and human plasma.
(a) Concentration of ascorbyl radical (marker of H2O2 production) in cell culture medium samples that were collected after incubation of LNCaP or PC-3 cells for the purposes of viability measurements (results presented in Fig. 1); Box: Characteristic EPR signal of ascorbyl radical with spectral simulation (pale); * - statistically significant (p < 0.05) compared to control (no Fe supplemeted). (b) The concentration of molecular oxygen and the rate of O2 consumption in cell culture medium supplemented with Asc (5 mM) or Fe (5 μM) + Asc (5 mM). CAT (600 U) was added at 15 min. The change in O2 concentration following CAT supplementation is presented as mean ± S.D. (c) Concentration of ascorbyl radical in human plasma samples collected after the incubation of LNCaP or PC-3 cells for the purposes of viability measurements; A low level of ascorbyl radical was found in some untreated plasma samples; Bars not sharing a common letter are significantly different (p < 0.05). (d) The concentration of molecular oxygen and the rate of O2 consumption in plasma supplemented with Asc (5 mM). Characteristic polarographic recordings obtained on plasma samples from three healthy volunteers (total Fe concentrations: volunteer (1) 23.0 μM; (2) 15.4 μM; (3) 24.2 μM) are presented. CAT was added at 15 min. Statistical analysis was performed using one-way ANOVA with post hoc Duncan test.
Fig. 3a shows that the incubation of cancer cells with Asc in cell culture medium results in a significant decrease in the level of intracellular thiol (-SH) groups, which are the main targets for H2O2-provoked oxidation24. This is in line with previous findings8,25. However, in the presence of iron at physiological concentration, the Asc-mediated decrease in the level -SH groups was abolished, i.e. iron prevented intracellular oxidation. Fenton reaction (Fe2+ + H2O2 → Fe3+ + OH− + ·OH) appears as a plausible mechanism of removal of extracellular H2O2 in the system with physiological iron. Asc is known to propel the Fenton reaction by maintaining iron in Fe2+ form, which is otherwise unstable under physiological pH26,27. We applied biochemical assays in order to quantify extracellular markers of hydroxyl radical (·OH)-mediated oxidation of proteins and lipids. Fig. 3b shows that the level of oxidation of extracellular proteins was about three times higher in the presence of physiological level of iron compared to culture medium iron concentration. The level of lipid peroxidation was not affected by iron supplementation (Fig. 3c). All these experiments have been also performed using 30 μM supplemented iron with very similar results. Altogether this implies that iron at physiological concentration and pharmacological Asc propel the production of ·OH, most of which are removed by protein oxidation. It is important to point out that we have applied EPR spin-trapping spectroscopy in order to directly detect the production of ·OH. However, in line with our previous experience, spin-trapping in Asc-rich systems is unfeasible because Asc reduces spin-adducts. Finally we tested the ability of pharmacological Asc and physiological Fe to protect cells from exogenous H2O2 (Fig. 3d, e). It can be observed that Asc in the presence of cell culture medium iron, as well as iron supplemented without Asc were incapable of protecting cancer cells. However, pharmacological Asc in combination with physiological Fe promoted degradation of H2O2 and diminished its cytotoxic effects.
The effects of ascorbate and iron on redox settings in cancer cell culture.
(a) Intracellular thiols in LNCaP and PC-3 cells. The results are normalized to 1 × 106 cells/mL. (b) Extracellular carbonyl groups (marker for oxidized proteins) and (c) MDA (marker for oxidized lipids) in supernatants that were collected following incubation of LNCaP and PC-3 cells. (d) Viability of LNCaP and (e) PC-3 cells exposed to H2O2 (200 μM) in the absence or the presence of Asc and/or Fe. Concentrations of supplemented Asc and Fe were 5 mM and 5 μM, respectively. Bars not sharing a common letter are significantly different (p < 0.05). Statistical analysis was performed using one-way ANOVA with post hoc Duncan test.
Two additional mechanisms that might be relevant for Fe-mediated cytoprotection against Asc were examined. It has been speculated that prolonged exposure of cancer cells to Asc might exert cytotoxic effects via provoking iron deficiency28,29. However, Fig. 4 shows that the total intracellular concentration of iron remains unaffected in the presence of extracellular Asc, implying that the cytoprotective effects of iron against Asc-provoked cell death are not related to iron deficiency. Further, it is known that the level of hypoxia inducible factor-1 (HIF-1), a transcription factor that is involved in the regulation of different aspects of cancer cell biology, can be affected by Asc30,31,32, iron33,34 and H2O235. Fig. 5 shows characteristic micrographs, intensities and histograms of HIF-1α immunofluorescence. In LNCaP cells, Asc provoked an increase in HIF-1α level. In addition, it can be observed that percentage distribution of Asc-treated LNCaP cells was shifted towards higher florescence intensities. Asc-provoked increase in HIF-1α level was diminished by iron (Fig. 5a). PC-3 cells showed a higher constitutive level of HIF-1α. The level was not affected by Asc, but the combination of pharmacological Asc and physiological Fe provoked its decrease (Fig. 5b).
Intracellular iron in LNCaP and PC-3 cells.
Cells were exposed to Asc (5 mM) and/or Fe (5 or 30 μM). The results are normalized to 1 × 106 cells/mL. Statistical analysis was performed using one-way ANOVA with post hoc Duncan test. There was no significant difference (p < 0.05) in concentration between any of the treatments.
The level of HIF-1α in cancer cells exposed to Asc (5 mM) and Fe (5 μM).
(a) LNCaP. (b) PC-3. Micrographs showing HIF-1α immunofluorescence and HIF-1α merged with DAPI staining of nuclei, average per-pixel intensities of HIF-1α immunofluorescence (bars not sharing a common letter are significantly different and percentage distribution of cells according to average per-pixel intensities of fluorescence are presented (the number of cells (%) was bracketed to 10 AU steps). Cells were stained 2 h after the treatment. Statistical analysis was performed using one-way ANOVA with post hoc Duncan test. All statistical differences were at the 0.001 level.
Fig. 6 shows the effects of Asc and Asc + Fe on multi-cellular tumour spheroid culture of LNCaP. It can be observed that Asc at both concentrations applied here exerted only weak tumour static effects, which appear not to be affected by iron supplementation.
Effects of pharmacological Asc on the size of tumour spheroids.
(a) Images of LNCaP spheroids obtained at 10× and 2× magnification. (b) The effects of Asc (5 mM) and Fe (5 μM) on spheroid growth. (c) The effects of Asc (10 mM) and Fe (5 μM) on spheroid growth. Area of each sphere was normalized to its area at 0 h (at the start of the treatment). a - significant compared to initial area (0 h); b - significant compared to area at 4 h. Statistical analysis was performed using one-way ANOVA with post hoc Duncan test.
Discussion
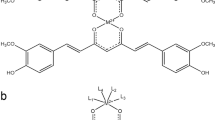
This is the first study of the anticancer effects of Asc that has taken into account physiological concentrations of iron. Schemes depicted in Fig. 7 summarise what is known about the pro-oxidative anticancer activity of Asc in the cell culture medium and what we have shown herein to take place in settings that resemble in vivo conditions. Sub-physiological concentrations of iron in cell culture media allow the accumulation of H2O2, which easily crosses the membrane in order to provoke intracellular oxidative damage resulting in cell death (Fig. 7a). On the other hand, when iron is present at the physiological level (even at the lower physiological limit), the decomposition of H2O2 compensates for H2O2 generation and prevents its accumulation (Fig. 7b). The removal of H2O2 is conducted predominately via the ·OH-generating Fenton reaction. Hydroxyl radical is considered to be the most notorious reactive oxygen species due to its high reactivity (about 109 times less stabile compared to H2O2)36. However, for the same reason, extracellularly-produced hydroxyl radical is incapable of reaching sensitive intracellular targets18. Most hydroxyl radicals are buffered by extracellular proteins and some by Asc and membrane lipids. Oxidised lipids are reduced by Asc/tocopherol coupled antioxidative activity37. Under such settings reactive oxygen species remain in the extracellular compartment leaving cancer cells generally unharmed. It should be stressed out that presented mechanisms are not dependent on cancer cells and types, as documented by using two lines with different metastatic potentials and ontogenetically different non-cancer cells.
Redox activity of Asc/Fe system.
(a) In cell culture media. (b) Under in vivo settings with physiological iron concentration. Asc reduces Fe3+ to Fe2+, which react with O2 in order to produce superoxide. The latter is dismutated to H2O2, which can affect cancer cells or be decomposed, depending on iron concentration. The decomposition is mediated via Fenton reaction and the oxidation of extracellular proteins and Asc. It is important to note that in vivo iron is not free but bound to hydroxyl, phosphate ions, small ligands or proteins (not presented). ·Asc - ascorbyl radical; CG - carbonyl groups; ·O2- - superoxide radical anion; ·OH - hydroxyl radical.
It has been shown recently that HIF-1α-signalling cascade is essential for cancer cells' resistance to ascorbate-provoked cytotoxicity31. The level of inducible subunit of HIF-1 (HIF-1α) is regulated by hydroxylation, which is performed by HIF-1 prolyl hydroxylases (HPH), leading to HIF-1α degradation. HPH show a complex net of regulators that involves Asc, Fe2+ and O2, which are required for HPH activity, as well as reducing agents (such as thiols that activate these enzymes), different glucose metabolites and H2O234. Several studies have shown that the supplementation of Asc to cultured cancer cells provokes a drop in HIF-1α level32,33,34. However, we found that Asc provoked an increase in HIF-1α level in LNCaP whereas it did not exert significant effects in PC-3 cells. A plausible explanation is in the opposing effects of Asc and H2O2 on the activity of HPH. Namely, in contrast to Asc, H2O2 is known to inhibit HPH and to provoke an increase in the HIF-1α level35. It is tempting to speculate that H2O2-provoked inhibition of HPH prevailed over the activating effects of Asc in LNCaP cells, which showed low constitutive HIF-1α level and in relation to this a probable high HPH activity. Hydrogen peroxide-mediated inhibition of HPH could take place either via intracellular oxidation of Fe2+ to Fe3+ or via a decrease in the intracellular level of thiols and Asc. In PC-3 cells, constitutive HIF-1α level was high (as noted previously33), so inhibitory effects of H2O2 on HPH could not be exerted/observed, and/or the opposing effects of Asc and H2O2 were balanced. Of note, high constitutive HIF-1α levels have been observed in many highly glycolytic cancer cells and it appears to be related to pyruvate- and oxaloacetate-mediated inhibition of HPH34. The setup changed in the presence of physiological iron. In LNCaP, Asc-provoked increase was significantly reduced, whereas in PC-3 the level of HIF-1α felt below baseline. These effects are most likely related the ability of physiological iron to prevented Asc-provoked H2O2 accumulation. Under such settings, HIF-1α lowering effects of supplemented Asc most likely emerged. It is worth mentioning that the supplementation of iron did not increase the intracellular iron concentration, however Asc might maintain iron in Fe2+ in the intracellular compartment thus increasing HPH activity. Altogether these phenomena are interesting, but appear only to reflect redox settings in our system. In other words, a decrease in the level of pro-survival factor in cells that were protected from the cytotoxic effects of Asc appears not to be directly involved in the mechanisms of protection.
Although our experimental setup took into account the total concentration of iron in relevant biological milieus (plasma and interstitial fluid), redox activity of iron in cell culture media and in vivo is further complicated by a number of iron-binding molecules, such as transferrin and feritin38. The concentrations of transferrin and ferritin as well as their saturation with iron in FCS are not consistent9, so their effects on redox activity of iron in cell culture medium are hard to estimate. Pertinent to this, it was essential to examine the effects of Asc on cancer cells in biological fluid. The absence of anticancer effects in human plasma implies that our setup (medium supplemented with iron) properly reflects in vivo redox milieu. In addition, anticancer effects gradually decreased in cell culture medium with increasing volume percent concentration of FCS, i.e. with increasing resemblance of the applied medium with biological fluid. It can be further argued that the redox activity of the Asc/Fe system in interstitial fluid, which is the main site of Asc's anticancer activity in vivo, could be different compared to plasma, since these differ in composition (for example in their proteome39). However, it has been documented that interstitial fluid and plasma show similar capacities to prevent iron-dependent oxidation17. It is noteworthy that the problems of unsuitability of common cell culture media for redox research, which clearly emerged in this case, have been outlined also by others and might affect the performance of a number of compounds other than Asc40.
The Pauling/Cameron–Creagan/Moertel “conflict” about the applicability of oral Asc in cancer treatment that went on throughout the 1970's and the 1980's ended in disappointment41. As a matter of fact, the concept of oral Asc application suffered from a major error at the very beginning. Namely, the bioavailability of ingested Asc is limited by the refractory response – a set of mechanisms that our organism uses in order to maintain flexible redox poise and normal redox signalling36. The findings of Levine and co-workers that even mega doses of oral Asc cannot raise its level in the blood over modest 200 μM pointed out the problem42. This instigated renewed interest in the application of Asc in cancer treatment, but this time using intravenous administration in order to bypass limited intestinal absorption and to reach millimolar Asc concentrations in the blood and interstitial fluid4,5. This was followed by somewhat spectacular results of a large number of in vitro studies which showed that cancer cells are efficiently killed by pharmacological Asc acting as a pro-drug for H2O2 production. Unfortunately, it appears that research of the anticancer effects of Asc suffered from systematic errors once again and that we are on the verge of yet another disappointment. In addition to findings presented here, other evidence predict a grim future for Asc-based cancer therapy. For example, Asc shows relatively limited efficiency in animal tumour models43. Pertinent to this, we employed tumour spheroid model which shows complexity that is between in vivo tumours and monolayer cultures and which is known to be more resistant to anticancer agents compared to the latter44. Only weak tumour static effects were observed implying that Asc-based therapy might suffer from more than one shortcoming. In addition, completed phase I clinical trials showed no objective anticancer response to treatment with pharmacological Asc1,2,3 and it appears that Asc has already slipped from the group of potential anticancer drugs to a category of chemotherapy adjuvants45,46. Nevertheless, a number of clinical trials are underway and our findings could be used in order to adjust current therapeutic approaches. Co-application of iron chelators in order to reduce redox active iron to a level that promotes the anticancer activity of Asc appears to be realistic. Iron chelation has shown significant in vitro and in vivo anticancer effects irrespective of Asc (most likely by causing iron deficiency)47. There are still many problems with iron chelation therapy, such as limited bioavailability, misdosing and toxicity38, but in order to promote Asc's anticancer effects, less aggressive agents, such as disulfiram, might be sufficient48.
Methods
Cells
Human androgen-dependent and androgen-independent prostate cancer cell lines, LNCaP and PC-3, were a kind gift from Prof. Ferdinando Nicoletti (Department of Biomedical Sciences, University of Catania, Italy). Cell lines were validated by short tandem repeat DNA fingerprinting and matched known American Type Culture Collection (ATCC, Rockville, USA) fingerprints. Cells in logarithmic growth phase were cultured in RPMI-1640 medium supplemented with 10% (v/v) FCS (PAA Laboratories, Pasching, Austria), 2 mM L-glutamine, 0.01% sodium pyruvate and antibiotics (culture medium) (Sigma-Aldrich, St. Louis, MO, USA), at 37°C in a humidified atmosphere with 5% CO2. After standard trypsinisation, cells were seeded in flat-bottomed 96-well plates (Sarstedt, Nümbrecht, Germany) (7 × 103 cells/well for LNCaP and 5 × 103 cells/well for PC-3) for viability determination, or in 6-well plates (3 × 105/well) for other measurements. Astrocytes were isolated from mixed glial cell cultures prepared from brains of newborn Dark Agouti rats as previously described49. Astrocytes were grown in the above-mentioned culture medium supplemented with 4 g/L glucose. They were purified by repetition of trypsinisation (0.25% trypsin and 0.02% EDTA, both from Sigma-Aldrich) and re-plating. The cells used in these experiments were obtained after the third passage. Astrocytes were seeded at 1.5 × 105 cells/mL/well in 24-well plates.
Treatment
Cells were incubated for 2 h in RPMI-1640 with 10% FCS or in undiluted human plasma (collected on the day of experiment), with or without L-ascorbic acid (Sigma-Aldrich) at final concentrations of 5 or 10 mM. Two hour incubation period mimics clinical pharmacokinetics and has been applied previously in similar in vitro studies. Ascorbate stocks were buffered to pH 7.0 with NaOH and prepared immediately before use. Iron was added to cell culture medium at final concentrations of 0, 5, 10, 15 and 30 μM in the form of FAC (17% iron content, Serva, Heidelberg, Germany) or FeCl3 (Sigma-Aldrich). Treatment with H2O2 (200 μM; Carlo Erba Reagents, Milano, Italy) was performed in the absence or the presence of Asc (5 mM) and/or FAC (5 μM). Plasma samples were obtained from six healthy volunteers between the ages of 30 and 45 years (m/f = 3/3), using Vacutainer tubes containing Li-heparin as the anticoagulant per 4 mL of blood (BD, Franklin Lakes, NJ, USA) and centrifugation (2000 g/10 min/4°C). A tourniquet was applied to the upper arm during sampling from antecubital vein and sampling was completed within 90 s following the tourniquet application. A special care was made in order to prevent haemolysis or the collection of erythrocytes or buffy coat. All procedures related to the use of human blood in this study are in conformity with the recommendation provided in The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. The protocols were approved by the local Ethics Committee. Viability experiments were performed in triplicate for each plasma sample. Iron was not supplemented to plasma samples.
Viability assays
Reduction of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-2Htetrazolium bromide (MTT; Sigma-Aldrich) to formazan reflects mitochondrial activity and viability of cultured cells, while the number of adherent, viable cells correlates with crystal violet (CV) (Mol, Belgrade, Serbia) staining. Following 2 h incubation period, supernatants were collected for EPR measurements, while cells were washed with PBS and resuspended in cell culture medium for additional 24 h. To evaluate mitochondrial respiration, MTT solution was added to cell cultures at the final concentration of 0.5 mg/mL, incubated for 1 h, after which produced formazan was dissolved in DMSO. In CV assay, adherent cells were first fixed with 4% PFA for 10 min and subsequently stained with 1% CV for 15 min at room temperature. The cells were then washed, dried and dye was dissolved in 33% acetic acid. Mitochondria-dependent production of formazan and the intensity of absorbed CV by adherent cells were assessed with an automated microplate reader at 570/640 nm. Cell viability was expressed relative to control (untreated cells; same experimental day).
Biochemical assays
Following 2 h incubation, with or without iron (5 μM) and/or Asc (5 mM), supernatants were collected, while cells were washed 3 times with PBS, snap frozen in liquid N2 and stored at −80°C. Frozen cells were detached with a Teflon cell scraper, dissolved in extraction buffer and centrifuged at 30000 g for 90 min. Intracellular content of thiol groups was determined according to Ellman50. Total concentration of intracellular iron was determined according to the method of Rad et al.51. Protein concentration was determined by the method of Bradford52. 2,4-Dinitrophenylhydrazine was used for determining carbonyl content in supernatants according to Levine et al.53. The carbonyl content was calculated from the absorbance measurement at 380 nm and an absorption coefficient of 22000 M−1 cm−1. The level of malondialdehyde (MDA) was measured according to procedure of Ohkawa et al.54. The concentration of iron in the plasma and medium was determined according to the method of Bouda55. CAT activity in plasma was determined using two previously described methods56,57.
EPR measurements
Samples were placed in Teflon tubes with a wall thickness of 0.025 mm and an internal diameter of 0.6 mm (Zeus Industries, Raritan, NJ, USA) and inserted into quartz capillaries. EPR spectra were recorded using a Varian E104-A EPR spectrometer operating at X-band (9.51 GHz) and EW software (Scientific Software Inc., Bloomington, IL, USA). EPR signal of ascorbyl radical in supernatants was recorded using the following settings: modulation amplitude, 2 G; modulation frequency, 100 kHz; microwave power, 20 mW. Simulation and double integration of EPR spectra of ascorbyl radical were performed in order to determine intensities of EPR signal of ascorbyl radical, using WINEPR SimFonia Computer Program (Bruker Analytische Messtechnik GmbH, Karlsruhe, Germany) and simulation parameter: aH = 2.1. The concentration of ascorbyl radical was determined using calibration curve that was prepared with 3-carboxyproxyl (Sigma-Aldrich) as a standard37. For the EPR assay for -SH groups36, cells were trypsinized, washed twice in PBS, resuspended in PBS at a density of 1.5 × 105 cells/100 μL and placed on ice. Thiol-sensitive biradical spin probe RSSR (Enzo Life Sciences International, Plymouth Meeting, PA, USA) was dissolved in DMSO and added to a final concentration of 100 μM. EPR spectra were recorded after 4 min incubation, using the following settings: modulation amplitude, 1 G; modulation frequency, 100 kHz; microwave power, 10 mW. The concentration of -SH groups was determined using calibration curve that was prepared with glutathione as a standard for intracellular thiols.
Oximetry
The O2 concentration and the rate of oxygen consumption/production (d[O2]/dt) was determined using a Clark electrode – OX1LP Dissolved Oxygen Package (Qubit Systems Inc, Kingston, ON, Canada) operating with Logger Pro 1 software (Vernier, Beaverton, OR, USA). Experiments were performed in RPMI-1640 + 10% (v/v) FCS with or without the addition of Asc (5 mM) and/or FAC (5 μM). All systems were recorded for 5 min before the addition of Asc and/or Fe, in order to establish the stability of baseline and zero rate of O2 change (not shown). Accumulation of H2O2 was determined by measuring O2 production induced by the addition of CAT to the system58. Although various other assays and probes for H2O2 quantification are available, most of them are likely to be interfered by millimolar concentrations of Asc59. CAT (600 U; Sigma-Aldrich C1345) was added at the point when systems approached a zero rate of O2 consumption. Polarographic measurements were also performed on plasma samples of three volunteers. CAT was supplemented 15 min after the application of Asc (5 mM).
HIF-1α immunofluorescence and quantification
Cells were seeded in glass bottom chambers (Lab-Tek® II Chamber Slide™, Thermo Fisher Scientific, Waltham, MA, USA) at 3 × 104 cells/chamber overnight. Cells were treated with Asc (5 mM) or Asc + Fe (5 μM) for 2 h, washed and resuspended in cell culture medium for additional 2 h at 37°C. Cells were fixed with 4% PFA at 4°C for 15 min and permeabilized in Triton X-100 (0.25%) for 10 min, which was followed by the blocking of non-specific staining with FCS (10%) for 30 min. Then, cells were stained with mouse anti-HIF-1-alpha [H1alpha67] (Abcam, Cambridge, UK) (1/200) antibody overnight at 4°C and visualized with fluorophore-labelled secondary antibody Alexa Fluor 555 donkey anti-mouse (Life Technologies - Invitrogen, Carlsbad, CA, USA) (1/500). Cell nuclei were counterstained with DAPI. Images were acquired using Zeiss Axiovert microscope (Carl Zeiss, Jena, Germany). Fluorescence measurements were performed using Image J (NIH, USA), as described previously60. Mean per-pixel fluorescence intensity of HIF-1α in the cross-section area of nucleus of each cell was evaluated and presented as arbitrary units (AU). In addition, the percentage distribution of cells showing fluorescence intensities within specific range (10 AU steps were used, e.g. 0–10 AU, 10–20 AU, etc) was established. The whole range of fluorescence intensities (0–255 AU) was covered. It is important to note that HIF-1α was not specifically located in nuclei, but this area was selected because it is well defined unlike the cross-section area of the whole cell.
Tumour spheroids
Spheroids were formed using a modified method of Ivascu and Kubbies61. In brief, 1 × 104 LNCaP cells were suspended in 100 μL of ice-cold medium and placed in standard polystyrene 96-well plate with a round bottom (Sarstedt, Nümbrecht, Germany; Prod. No. 82.1582.001). Matrigel® (BD Labware, Bedford, MA, USA) was applied at 2.5% (v/v) using ice-cold pipette tip. Spheroid formation was initiated by centrifugation of the plates at 1000 g for 10 min. The plates were incubated under standard cell culture conditions for 2 days, after which compact spheroid morphology was evident. The number of spheroids was 10–20 per well. It is noteworthy that previously described procedure for formation of a single spheroid used poly-HEMA–coated plates and a lower number of LNCaP cells per mL (1 × 104 cells in 200 μL)61. Spheroids were further untreated or treated with Asc (5 mM or 10 mM), Fe (5 μM), or with both Asc and Fe. Final volume per well was 200 μL. Images of spheroids were acquired immediately after and 4 h and 24 h after the beginning of the treatment, using Zeiss Axiovert microscope and magnifier Leica MZ16 (Leica Microsystems, Heerbrugg, Switzerland). Cells were treated for 24 h. The treatment could not be stopped, i.e. medium change was not possible, because it would result in the movement and/or decomposition of spheroids. For each treatment, cross-section areas of 20 spheroids with distinct round morphology (randomly selected in three wells) were followed up and measured at three time points using Image J. The area of each spheroid at 4 h and 24 h was normalized to the area at the beginning of the treatment.
Statistics
All experiments were performed at least three times on separate experimental days. The data are presented as mean ± standard deviation (S.D.). Statistical differences between the values obtained in different experimental settings were evaluated by the means of ANOVA (two-way or one-way as appropriate) with post hoc Duncan's range test (p < 0.05) using STATISTICA 8.0 (StatSoft Inc, Tulsa, OK, USA).
References
Riordan, H. D. et al. A pilot clinical study of continuous intravenous ascorbate in terminal cancer patients. P. R. Health Sci. J. 24, 269–276 (2005).
Hoffer, L. J. et al. Phase I clinical trial of i.v. ascorbic acid in advanced malignancy. Ann. Oncol. 19, 1969–1974 (2008).
Stephenson, C. M., Levin, R. D., Spector, T. & Lis, C. G. Phase I clinical trial to evaluate the safety, tolerability and pharmacokinetics of high-dose intravenous ascorbic acid in patients with advanced cancer. Cancer Chemother. Pharmacol. 72, 139–146 (2013).
Parrow, N. L., Leshin, J. A. & Levine, M. Parenteral ascorbate as a cancer therapeutic: A reassessment based on pharmacokinetics. Antioxid. Redox Signal. 19, 2141–2156 (2013).
Du, J., Cullen, J. J. & Buettner, G. R. Ascorbic acid: chemistry, biology and the treatment of cancer. Biochim. Biophys. Acta 1826, 443–457 (2012).
Chen, Q. et al. Ascorbate in pharmacologic concentrations selectively generates ascorbate radical and hydrogen peroxide in extracellular fluid in vivo. Proc. Natl. Acad. Sci. USA 104, 8749–8754 (2007).
Deubzer, B. et al. H2O2-mediated cytotoxicity of pharmacologic ascorbate concentrations to neuroblastoma cells: potential role of lactate and ferritin. Cell. Physiol. Biochem. 25, 767–774 (2010).
Olney, K. E. et al. Inhibitors of hydroperoxide metabolism enhance ascorbate-induced cytotoxicity. Free Radic. Res. 47, 154–163 (2013).
Kakuta, K., Orino, K., Yamamoto, S. & Watanabe, K. High levels of ferritin and its iron in fetal bovine serum. Comp. Biochem. Physiol. A Physiol. 118, 165–169 (1997).
Wesselius, L. J. et al. Iron uptake promotes hyperoxic injury to alveolar macrophages. Am. J. Respir. Crit. Care Med. 159, 100–106 (1999).
Ganz, T. & Nemeth, E. Hepcidin and disorders of iron metabolism. Annu. Rev. Med. 62, 347–360 (2011).
Bae, Y. J., Yeon, J. Y., Sung, C. J., Kim, H. S. & Sung, M. K. Dietary intake and serum levels of iron in relation to oxidative stress in breast cancer patients. J. Clin. Biochem. Nutr. 45, 355–360 (2009).
Panis, C. et al. Differential oxidative status and immune characterization of the early and advanced stages of human breast cancer. Breast Cancer Res. Treat. 133, 881–888 (2012).
Weijl, N. I. et al. Non-protein bound iron release during chemotherapy in cancer patients. Clin. Sci. (Lond.) 106, 475–484 (2004).
Cavill, I., Staddon, G. & Jacobs, A. Iron kinetics in the skin of patients with iron overload. J. Invest. Dermatol. 58, 96–98 (1972).
Freitas, I. et al. Iron accumulation in mammary tumor suggests a tug of war between tumor and host for the microelement. Anticancer Res. 27, 3059–3065 (2007).
Dabbagh, A. J. & Frei, B. Human suction blister interstitial fluid prevents metal ion-dependent oxidation of low density lipoprotein by macrophages and in cell-free systems. J. Clin. Invest. 96, 1958–1966 (1995).
Hempel, S. L., Buettner, G. R., Wessels, D. A., Galvan, G. M. & O'Malley, Y. Q. Extracellular iron (II) can protect cells from hydrogen peroxide. Arch. Biochem. Biophys. 330, 401–408 (1996).
Herst, P. M., Broadley, K. W., Harper, J. L. & McConnell, M. J. Pharmacological concentrations of ascorbate radiosensitize glioblastoma multiforme primary cells by increasing oxidative DNA damage and inhibiting G2/M arrest. Free Radic. Biol. Med. 52, 1486–1493 (2012).
Halliwell, B. & Gutteridge, J. M. The antioxidants of human extracellular fluids. Arch. Biochem. Biophys. 280, 1–8 (1990).
Halliwell, B. & Gutteridge, J. M. C. Free Radicals in Biology and Medicine. 145–146 (Oxford University Press, Oxford, 2007).
Chen, Q. et al. Pharmacologic ascorbic acid concentrations selectively kill cancer cells: action as a pro-drug to deliver hydrogen peroxide to tissues. Proc. Natl. Acad. Sci. USA 102, 13604–13609 (2005).
Welsh, J. L. et al. Pharmacological ascorbate with gemcitabine for the control of metastatic and node-positive pancreatic cancer (PACMAN): results from a phase I clinical trial. Cancer Chemother. Pharmacol. 71, 765–775 (2013).
Spasojević, I., Jones, D. R. & Andrades, M. E. Hydrogen peroxide in adaptation. Oxid. Med. Cell. Longev. 2012, 596019 (2012).
Park, S. et al. L-Ascorbic acid induces apoptosis in acute myeloid leukemia cells via hydrogen peroxide-mediated mechanisms. Int. J. Biochem. Cell Biol. 36, 2180–2195 (2004).
Riemer, J., Hoepken, H. H., Czerwinska, H., Robinson, S. R. & Dringen, R. Colorimetric ferrozine-based assay for the quantitation of iron in cultured cells. Anal. Biochem. 331, 370–375 (2004).
Tulpule, K., Robinson, S. R., Bishop, G. M. & Dringen, R. Uptake of ferrous iron by cultured rat astrocytes. J. Neurosci. Res. 88, 563–571 (2010).
Kang, J. S. et al. Sodium ascorbate (vitamin C) induces apoptosis in melanoma cells via the down-regulation of transferrin receptor dependent iron uptake. J. Cell. Physiol. 204, 192–197 (2005).
Carosio, R., Zuccari, G., Orienti, I., Mangraviti, S. & Montaldo, P. G. Sodium ascorbate induces apoptosis in neuroblastoma cell lines by interfering with iron uptake. Mol. Cancer 6, 55 (2007).
Kuiper, C., Dachs, G. U., Currie, M. J. & Vissers, M. C. Intracellular ascorbate enhances hypoxia-inducible factor (HIF)-hydroxylase activity and preferentially suppresses the HIF-1 transcriptional response. Free Radic. Biol. Med. 69, 308–317 (2014).
Sinnberg, T. et al. The ROS-induced cytotoxicity of ascorbate is attenuated by hypoxia and HIF-1alpha in the NCI60 cancer cell lines. J. Cell Mol. Med. 18, 530–541 (2014).
Kawada, H. et al. High concentrations of L-ascorbic acid specifically inhibit the growth of human leukemic cells via downregulation of HIF-1α transcription. PLoS One 8, e62717 (2013).
Knowles, H. J., Raval, R. R., Harris, A. L. & Ratcliffe, P. J. Effect of ascorbate on the activity of hypoxia-inducible factor in cancer cells. Cancer Res. 63, 1764–1768 (2003).
Lu, H., Dalgard, C. L., Mohyeldin, A., McFate, T., Tait, A. S. & Verma, A. Reversible inactivation of HIF-1 prolyl hydroxylases allows cell metabolism to control basal HIF-1. J. Biol. Chem. 280, 41928–41939 (2005).
Qutub, A. A. & Popel, A. S. Reactive oxygen species regulate hypoxia-inducible factor 1alpha differentially in cancer and ischemia. Mol. Cell Biol. 28, 5106–5019 (2008).
Spasojević, I. Free radicals and antioxidants at a glance using EPR spectroscopy. Crit. Rev. Clin. Lab. Sci. 48, 114–142 (2011).
Sharma, M. K. & Buettner, G. R. Interaction of vitamin C and vitamin E during free radical stress in plasma: an ESR study. Free Radic. Biol. Med. 14, 649–653 (1993).
Kell, D. B. Iron behaving badly: inappropriate iron chelation as a major contributor to the aetiology of vascular and other progressive inflammatory and degenerative diseases. BMC Med. Genomics 2, 2 (2009).
Wiig, H., Tenstad, O., Iversen, P. O., Kalluri, R. & Bjerkvig, R. Interstitial fluid: the overlooked component of the tumor microenvironment? Fibrogenesis Tissue Repair. 3, 12 (2010).
Halliwell, B. Oxidative stress in cell culture: an under-appreciated problem? FEBS Lett. 540, 3–6 (2003).
Wittes, R. E. Vitamin C and cancer. N. Engl. J. Med. 312, 178–179 (1985).
Levine, M. et al. Vitamin C pharmacokinetics in healthy volunteers: evidence for a recommended dietary allowance. Proc. Natl. Acad. Sci. USA 93, 3704–3709 (1996).
Tian, J., Peehl, D. M. & Knox, S. J. Metalloporphyrin synergizes with ascorbic acid to inhibit cancer cell growth through fenton chemistry. Cancer Biother. Radiopharm. 25, 439–448 (2010).
Zhang, X. et al. Induction of mitochondrial dysfunction as a strategy for targeting tumour cells in metabolically compromised microenvironments. Nat. Commun. 5, 3295 (2014).
Cullen, J. J., Spitz, D. R. & Buettner, G. R. Comment on “Pharmacologic ascorbate synergizes with gemcitabine in preclinical models of pancreatic cancer,”. i.e., all we are saying is, give C a chance. Free Radic. Biol. Med. 50, 1726–1727 (2011).
Wilson, M. K., Baguley, B. C., Wall, C., Jameson, M. B. & Findlay, M. P. Review of high-dose intravenous vitamin C as an anticancer agent. Asia. Pac. J. Clin. Oncol. 10, 22–37 (2014).
Dixon, S. J. & Stockwell, B. R. The role of iron and reactive oxygen species in cell death. Nat. Chem. Biol. 10, 9–17 (2014).
Spasojević, I. et al. Bioavailability and catalytic properties of copper and iron for Fenton chemistry in human cerebrospinal fluid. Redox Rep. 15, 29–35 (2010).
McCarthy, K. D. & de Vellis, J. Preparation of separate astroglial and oligodendroglial cell cultures from rat cerebral tissue. J. Cell. Biol. 85, 890–902 (1980).
Ellman, G. Tissue sulfhydryl groups. Arch. Biochem. Biophys. 82, 70–77 (1959).
Rad, A., Janic, B., Iskander, A. S. M., Soltanian-Zadeh, H. & Arbab, A. Measurement of quantity of iron in magnetically labeled cells: comparison among different UV/VIS spectrometric methods. BioTechniques 43, 627–636 (2007).
Bradford, M. M. A rapid and sensitive method for the quantification of microgram quantities of protein utilizing the principles of protein-dye binding. Anal. Biochem. 72, 248–254 (1976).
Levine, R. L. et al. Determination of carbonyl content in oxidatively modified proteins. Methods Enzymol. 186, 464–478 (1990).
Ohkawa, H., Ohishi, N. & Yagi, K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal. Biochem. 95, 351–358 (1979).
Bouda, J. Determination of iron with bathophenanthroline without deproteinisation. Clin. Chim. Acta. 21, 159–160 (1968).
Iwase, T. et al. A simple assay for measuring catalase activity: a visual approach. Sci. Rep. 3, 3081 (2013).
Claiborne, A. Handbook of Methods for Oxygen Radical Research. 76–81 (CRC Press Inc, Boca Raton, 1984).
Clément, M. V., Ramalingam, J., Long, L. H. & Halliwell, B. The in vitro cytotoxicity of ascorbate depends on the culture medium used to perform the assay and involves hydrogen peroxide. Antioxid. Redox Signal. 3, 157–163 (2001).
Rawal, M. et al. Manganoporphyrins increase ascorbate-induced cytotoxicity by enhancing H2O2 generation. Cancer Res. 73, 5232–5241 (2013).
Bajić, A. et al. Fluctuating vs. continuous exposure to H2O2: the effects on mitochondrial membrane potential, intracellular calcium and NF-κB in astroglia. PLoS One 8, e76383 (2013).
Ivascu, A. & Kubbies, M. Rapid generation of single-tumor spheroids for high throughput cell function and toxicity analysis. J. Biomol. Screen. 11, 922–932 (2006).
Acknowledgements
This work was supported by the Ministry of Science, Education and Technological Development of the Republic of Serbia, grant numbers 173013 and 173014. We thank Jana Blaževski and Filip Petković at the Department of Immunology, Institute for Biological Research “Siniša Stanković” for excellent technical assistance.
Author information
Authors and Affiliations
Contributions
I.S. and D.M.I. designed the research; M.M., J.B.P., M.S., D.M.I., S.M. and I.S. performed the experiments; I.S., J.B.P., M.M. and M.S. analysed the data. I.S., D.J., M.M., J.B.P. and D.M.I. wrote the paper.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary Information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Mojić, M., Pristov, J., Maksimović-Ivanić, D. et al. Extracellular iron diminishes anticancer effects of vitamin C: An in vitro study. Sci Rep 4, 5955 (2014). https://doi.org/10.1038/srep05955
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep05955
This article is cited by
-
Noninvasive evaluation of 18F-FDG/18F-FMISO-based Micro PET in monitoring hepatic metastasis of colorectal cancer
Scientific Reports (2018)
-
Coordinate and redox interactions of epinephrine with ferric and ferrous iron at physiological pH
Scientific Reports (2018)
-
Effect of cobalt(II) chloride hexahydrate on some human cancer cell lines
SpringerPlus (2016)
-
Molecular mechanisms of pharmacological doses of ascorbate on cancer cells
Wiener Medizinische Wochenschrift (2015)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.