Abstract
The one-step nucleic acid amplification (OSNA) assay is a molecular procedure that can identify deposits of breast cancer (BC) cells in the sentinel lymph node (SLN). We examined the consistency of the OSNA assay with a classic hematoxylin-eosin (H&E)-based immunohistochemistry (IHC) study and evaluated how OSNA-based axillary staging might impact the therapeutic management of BC patients. SLN biopsy results were considered to be positive in 60 patients (40%) in the OSNA group (N = 148) and in 43 (28%) patients in the IHC cohort (N = 153, p = 0.023). There was no difference in the macrometastasis (22% for OSNA, 15% for H&E, p = 0.139) or micrometastasis (19% for OSNA, 13% for H&E, p = 0.166) rates, but we found statistically significant differences in the number of isolated tumor cells (1% for OSNA, 11% for H&E, p < 0.001). There were no differences in the administration rate of adjuvant systemic therapy between the OSNA (66% in the SLN+ patients) and the H&E (74% in the SLN+ patients) groups (p = 0.159). The OSNA assay allows for the detection of SLN metastases more precisely than conventional pathologic methods but does not alter the therapeutic management of SLN+ BC patients.
Similar content being viewed by others
Introduction
The disease status of axillary lymph nodes is the most significant prognostic factor for patients with early-stage breast cancer (BC) and determining this status is essential in the decision-making process of administering adjuvant systemic therapy1,2. The sentinel lymph node (SLN) is defined as the first lymph node that receives lymph drainage from a tumor area; negative findings after an SNL biopsy in clinically node-negative BC patients can prevent unnecessary dissection of the axillary lymph node, which can preclude any morbidity that is associated with this procedure3. Conventional hematoxylin and eosin (H&E)-based histopathological studies are limited to the accurate measurement of the total metastatic volume in a lymph node4. Therefore, common intraoperative techniques that are used to identify tumor deposits, including touch imprint, crash and cytological smear preparations, as well as frozen sections, all lack a sufficient degree of sensitivity. Accordingly, the false-negative results from these techniques range from 26% to 43% compared to the final histopathological results5,6. In this scenario, a definitive SLN analysis is usually performed postoperatively by staining consecutive formalin-fixed tissue sections using conventional H&E-based immunohistochemistry (IHC). Unfortunately, the classical pathologist's evaluation of the tissue sections can sometimes neglect low volume metastases7,8,9. Therefore, there is a need for rapid and reproducible methods with high sensitivity and specificity that can be routinely used for the intraoperative assessment of the SLN involvement status.
Higher sensitivity levels than those provided by classical histological assessments have been developed with molecular approaches based on the reverse-transcriptase polymerase chain reaction (RT-PCR) for the detection of tumor deposits in the lymph nodes of BC patients10,11,12. In this regard, cytokeratin 19 (CK19) has become a suitable marker to identify BC cell deposits in lymph nodes because virtually all BC cells express this cytoskeletal protein. Recently, a new semi-automated molecular method for the rapid intraoperative diagnosis of BC lymph node metastases has been developed using one-step nucleic acid amplification (OSNA). The OSNA-CK19 assay (Sysmex Corporation, Kobe, Japan) is based on the homogenization of lymph node samples followed by real-time amplification and direct quantification of the CK19 mRNA level in the lysate; moreover, the results are available within 30–40 minutes.
Several studies have assessed whether the performance of the OSNA assay is comparable to an extensive histological work-up that includes staining with the classical H&E-based IHC method13,14,15. In these studies, lymph node samples were fragmented approximately into two equal parts, with half of the volume subjected to the OSNA assay and the other half used for the conventional H&E-IHC test. Because metastases are generally not randomly distributed within the lymph nodes16, halving a lymph node may result in inconsistent findings. This result may occur because of the unbalanced spatial distribution of the metastasis that is present in one half and absent in the other. Sampling bias may arise if different parts of the lymph node are used for different diagnostic tests; although this situation has been recognized as a major source of inconsistent results, note that the false-negative rate of the OSNA assay compared to intensive histology has been found within a generally tolerable limit of 10% (i.e., 8.3%)4.
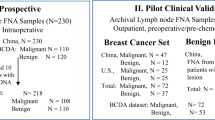
In routine clinical practice at our center, we recently aimed to evaluate the advantages, if any, of the OSNA whole node assay in the SLN. We compared the results of the OSNA assay with those of the classical histopathological analysis in an independent, historical cohort from the same institution. We evaluated a total of 320 patients with early T1-2 BC17,18 and with no clinical nodal involvement and who underwent SLN biopsy at our institution between January 2007 and December 2012. The SLN was analyzed with OSNA in 148 patients using the whole SLN. The OSNA results were then compared to those found with a classical H&E-based IHC study19 of 153 patients who had previously undergone a SLN biopsy. We evaluated the characteristics of the patients in both groups and compared the number and type of metastases that were detected using both methods; we also compared the surgical procedures that were required by the patients in each group. Additionally, we investigated whether the method employed to detect disease involvement of SLNs might impact the administration rate of adjuvant systemic therapy. We now report our results.
Results
Table 1 summarizes the demographic and tumor characteristics of the patients in the H&E-based IHC and OSNA cohorts. There was no significant difference between the IHC and OSNA groups in terms of age, menopausal status, type of surgery, histological type, estrogen receptor status, HER2 status and pathological T classification. Overall, the two study populations were mostly equivalent regarding their demographic and tumor characteristics.
Sentinel node analysis
Using two cohorts that were well-matched for all tumor and patient characteristics, the incidence of any type of metastasis in the cohort of SLN biopsies that were assessed by the OSNA assay was significantly greater than (n = 6 0, 40% of the SLN-positive patients) those in the classical H&E-based IHC cohort (n = 43, 28% of the SLN-positive patients; p = 0.023) (Table 2). Although we observed differences in the prevalence of patients with macrometastases (n = 32, 22% for OSNA, n = 23, 15% for H&E-based IHC) or micrometastases (n = 28, 19% for OSNA, n = 20, 13% for H&E-based IHC), these differences were not statistically significant (p = 0.139 and p = 0.166 for macrometastases and micrometastases, respectively). Conversely, the difference in the proportion of isolated tumor cells (n = 2, 1% for OSNA; n = 17, 11% for H&E-based IHC) was statistically significant (p < 0.001).
Regarding the number of axillary lymphadenectomies (ALND) that were performed (Table 2), a borderline significant trend (p = 0.05) was observed between ALND in the OSNA group (n = 51/148, 34%) and in the classical H&E-based IHC group (n = 37/153, 24%).
Finally, we evaluated whether an improved axillary staging using OSNA significantly impacted the administration rate of adjuvant systemic therapy among SLN+ patients (Table 3). Importantly, the decisions for adjuvant systemic therapy were not significantly affected (p = 0.159) by the type of procedure that evaluated SLN involvement (n = 42/60, 66% in the SLN-positive OSNA patients; n = 32/43, 74% in the SLN-positive H&E-based IHC patients).
Discussion
Several studies have reported that the classical H&E-based IHC SLN analysis method significantly underestimates the axillary staging of BC20,21,22 compared with molecular studies of SLNs by OSNA. We recently confirmed this finding in the Breast Complete Lymphadenectomy OSNA Study for Enhanced Review-I (B-CLOSER-I), a multicenter study that aimed to compare the use of histopathology and OSNA for the pathological staging of axillary lymph nodes after identifying positive SLNs in patients with primary BC23; according to OSNA, the traditional histopathological analysis misclassified 41.8% of patients as negative for axillary node metastasis. However, few reports have evaluated whole SLN tissue using the OSNA assay to eliminate tissue allocation bias. Our current retrospective cohort study confirms that the OSNA assay that involves whole lymph node tissue can significantly detect more metastases than conventional histological examinations of the SLN. Although our findings are consistent with those recently reported by Santaballa et al.22, we failed to observe any differences (between the rates of micrometastases and macrometastases) that could explain the significantly increased proportion of positive SLNs in the OSNA group.
It is commonly argued that the OSNA assay detects a greater number of metastases in SLNs compared to the classic histopathological analysis because of the OSNA assay's ability to detect more low-volume nodal metastases. Although two reports by Godey et al.24 and Klinguer et al.25 reported no differences between the axillary staging using the OSNA and the conventional histopathology; note that both the methodology and the inclusion criteria for the OSNA and IHC cohorts were different than those employed in our current study. Interestingly, we observed a remarkably significant decrease in the ITC rate in the OSNA assay cohort. These findings support the study performed by Visser et al.13, who reported that ITC (i.e., measuring up to 0.2 mm in maximum diameter) detected by IHC could not be detected by OSNA-CK19 and were classified as lymph node negative. At present, lymph nodes that contain ITC detected by routine histology are considered to be clinically negative metastatic lymph nodes and are designated as N0(i+) using the TNM classification. Most ITC are found in the lymph nodes of BC patients by cytokeratin immunohistochemical stain but not by H&E staining26; the clinical relevance of ITC is largely unknown and ALND is not recommended in cases with ITC27.
Using relatively large, matched study groups in which the baseline patient characteristics were well-balanced, our study revealed a 12% increase in the number of positive SLNs using the OSNA assay compared to the results yielded by IHC. Given that the prognostic value of SLN positivity has not been unambiguously clarified, the clinical relevance of an improved axillary staging system using OSNA might be difficult to establish. In our study, an improved detection of OSNA-positive SLNs significantly augmented the number of ALNDs that were performed. Until a few years ago, all patients with metastatic SLNs required an axillary lymphadenectomy. Based on the recommendations of the 2011 St. Gallen Consensus Conference18 as well as on the findings of the ACOSOG Z0011 study28, the presence of micrometastasis in the SLN biopsy is no longer considered to be an indication for axillary clearance. ALND might also be avoided in cases of macrometastases in patients with only one or two positive SLNs, who have undergone breast-conserving surgery and who have received post-operative whole-breast radiation and systemic adjuvant therapy. Accordingly, a recent meta-analysis by Tiernan et al.29 has argued that the OSNA assay could be appropriate only to some patients with macrometastases who may benefit from an ALND during the same procedure, thus avoiding a second procedure.
As mentioned in the “Patients and Methods” section and following the recommendations of the 2011 St. Gallen Consensus Conference18, our center has not considered the presence of micrometastases in SLN biopsies as an indication for further axillary surgery since 2012. The current consensus is to maintain the indication of ALND in all patients with positive SLNs based on the recommendations of the 2013 Spanish Society of Senology and Breast Pathology (SESPM)30. This recommendation includes patients with an SLN tumor load of more than 15,000 copies of CK19 mRNA per μl, patients diagnosed with macrometastases in the SLN, according to the Seventh Edition of TNM (except in the context in which patients fulfill “low risk” criteria for the primary tumor), patients who meet the test criteria of the ACOSOH Z0011 study31 and patients who are included in clinical trials20,21,22. Nevertheless, the full analysis of whole lymph nodes by the OSNA assay allows us to perform lymphadenectomy in the same surgical procedure in all cases. This analysis is not always possible when the patients are evaluated by the H&E-based IHC method, for which the full results cannot be obtained until later. Indeed, the performance of a single axillary surgery can preclude not only a second surgery and accelerate the initiation of adjuvant therapy25, but it might also save the hospital a significant amount of money because fewer hospital beds and operating rooms would be needed33. Consistent with the findings of Francissen et al.34, an internal review of the subjects who were included in our current study revealed that 13% of the patients with a negative intraoperative histological indication of metastasis yielded a positive result for metastasis in the SLN. This significant false-negative rate is mainly attributed to the failure to detect micrometastases, which has been found to range from 30% to 40% compared to the final histopathological results. Based on available evidence, BC patients with intraoperative histologically undetected micrometastases should not undergo a second surgery. In this new scenario, the improved axillary staging by the OSNA assay raises some clinical questions. Is the correlation between BC survival and tumor load assessed by OSNA comparable to that obtained with the classical histopathological axillary staging? What is the risk of negative SLN involvement in patients with metastatic SLN (as detected by OSNA) and the pertinence of ALND? Although some authors have tried to establish a correlation between OSNA-determined tumor burden and the possibility of axillary involvement32, we are still lacking an unambiguous response to the relevance of a quantitative assessment of the total tumoral load in the SLN using the OSNA assay.
An accurate knowledge of the disease status of the axillary lymph nodes is the most significant prognostic factor in the decision-making process with regards to the administration of adjuvant systemic therapy in patients with early-stage BC. However, while the OSNA method for the intraoperative analysis of BC SLNs can obviate a second operation in the axilla and thereby expedite the progression to adjuvant therapy, there is still a lack of research indicating how OSNA-based axillary staging might impact the therapeutic management of BC patients. This dearth is meaningful because adjuvant systemic therapy will be offered to those patients with SLN involvement. To the best of our knowledge, this report is the first to show that the rate of administration of adjuvant systemic therapy among BC patients with metastatic SLNs is not significantly affected by the type of procedure that is used to identify the deposits of BC cells in the lymph nodes. In our study, an improved axillary staging system that employs the OSNA assay failed to significantly alter the decisions regarding adjuvant systemic therapy.
Our study confirms that the OSNA assay allows for a more precise detection of SLN metastases compared to conventional pathology. An improved axillary staging system using OSNA provides a more reliable indicator of the need for an ALND in the same surgical procedure and does not alter the therapeutic management of BC patients with cancer that has spread to the SLNs.
Methods
Patients
We performed a retrospective cohort study of two homogeneous populations of BC patients at the Hospital Universitari de Girona Dr. Josep Trueta in Girona, Spain. This study consisted of 320 consecutive subjects with no clinical lymph node involvement, according to a physical examination and ultrasound of the axilla. The study was performed in accordance with relevant guidelines and regulations. The study was reviewed and approved by the institutional review board (IRB) of Dr. Josep Trueta Hospital. According to the IRB review, the investigators irreversibly anonymized (stripped of any link to the original patient) all the tissues and existing data in such a manner that subjects cannot be identified, directly or through identifiers linked to the subjects. Most patients had pT1-2 BC (i.e., the tumor size measured up to 5 cm, per the TNM classification17) and underwent an axillary SLN procedure with a radioisotope tracer between January 2007 and December 2012. SLN staging was performed using the classical H&E-based IHC technique from January 2007 until November 2009. The OSNA assay was employed to assess the SLN from December 2009 to December 2012. A few patients with pT3 were included because their tumor sizes were underestimated prior to surgery. Nineteen cases were excluded from the data analysis for the following reasons: lack of nodal migration, lack of CK19 protein expression in the histological study, neoadjuvant chemotherapy and lack of accurate or complete medical record.
The classical H&E-based IHC cohort consisted of 153 patients and the OSNA cohort consisted of 148 patients. The demographic characteristics of the 2 cohorts are presented in Table 1. The primary tumor size according to pathological analysis was classified according to the Seventh Edition of the AJCC Cancer Staging Manual. The cutoffs for estrogen receptor (ER) and progesterone receptor (PR) immunoreactivity were 10% positive cells, irrespective of intensity. Human growth factor receptor 2 (HER2) positivity was defined as either HER2 3+ (i.e., strongly positive in >10% of cancer cells by IHC) or HER2 2+ (moderately positive in >10% of cancer cells by IHC) and gene amplification ≥2 by fluorescence in situ hybridization.
SLN biopsy procedure
The localization of the sentinel node was identified using a Technetium-99m-labeled colloid (Nanocoll, Amersham Swan, Eindhoven, the Netherlands). One day before surgery, the tracer was injected into the intradermal and subdermal spaces in the vicinity of the tumor and into the retrotumoral space. In all cases, lymphoscintigraphy was performed 1 hour after the injection.
A systematic axillary lymph node dissection (ALND) was performed for all patients whose SLNs were positive for both micro- and macrometastases. ALND was not performed in five patients in the H&E-based IHC cohort because of special circumstances (e.g., elderly women with micrometastasis in the SLN and a high risk for surgical comorbidities). Since 2012, based on the recommendations of the 2011 St. Gallen Consensus Conference18, the presence of micrometastases in SLN biopsies has not been considered as an indication for further axillary surgery in our center.
Study of the SLN by IHC
The classical pathological study was based on a first-time intraoperative evaluation of excised nodes that were bisected across their long axis. Care was taken to obtain complete cross sections from the maximum diameter. For each lymph node half, a pair of imprints was made by gently touching the cut surface of the SLN to a glass slide. One imprint from each pair was air dried and stained with the Diff-Quick stain. The second imprint from each surface was immediately fixed for 3 minutes in 95% ethanol and then stained with H&E. If the SLN was >4 mm in width, the node was sliced into 4-mm slices; two imprints were made of each cut surface, one was air-dried and stained with Diff-Quick and the other was fixed in ethanol and stained with H&E. The imprints were then reviewed intraoperatively by either a board certified cytopathologist or a pathologist with informal training in cytology. Diagnostic categories included whether the node was positive or negative for tumor cells or whether atypical cells were present.
The surgical team was subsequently notified of the results. After an interpretation was rendered, the SLN was fixed in 10% formalin, processed in the usual manner and embedded in paraffin. A single H&E-stained section of the SLN was cut from the paraffin block and examined. If the initial review of the H&E-stained section was negative for tumor or atypical cells, a SLN protocol (consisting of an additional three H&E stained levels, cut at 50-μm intervals in conjunction with immunohistochemical stains for cytokeratin [AE1/AE3, Dako, Carpinteria, CA]) was performed on the first of the three levels. IHC studies were conducted using the avidin-biotin-peroxidase complex method, which has been described elsewhere19. Immunohistochemical stains for cytokeratin were considered to be positive if strong immunoreactivity in cell clusters or in individual cells was identified which demonstrated anatomic and cytologic features of metastatic tumor cells. After the histological analysis, the size of a metastasis was determined by its largest diameter and the metastasis was subsequently categorized as either isolated tumor cells (ITC, tumor deposits <0.2 mm), micrometastasis (>0.2 mm but <2.0 mm), or macrometastasis (tumor deposits ≥2.0 mm).
Study of the SLN by OSNA
A whole SLN was homogenized with LYNORHAG lysis buffer (Sysmex Corp., Hyogo, Japan). CK19 mRNA in each lysate was amplified using a LYNOAMP BC gene amplification reagent (Sysmex Corp.) and then a 2-μl sample of each lysate was subjected to an RT-LAMP reaction. The CK19 mRNA copy number was detected by measuring the rise time based on a standard curve using a RD-100i (Sysmex Corp.). The SLN was assessed as OSNA-negative (−) when fewer than 250 copies per μl were present and as OSNA-positive (+) when there were more than 250 copies per μl. Although the OSNA assay is unsuitable for measurements, a semiquantitative display of metastatic volume-related data approximately matches the arbitrary categories of micrometastasis and macrometastasis. If CK19 mRNA copy numbers were fewer than 100 copies per μl of lysate, the result was designated as negative (pN0), whereas copy numbers between 100 and 250 copies per μl of lysate were designated as ITC. Copy numbers between 250 and 5,000 copies per μl of lysate were designated as micrometastases and more than 5,000 copies per μl of lysate were designated as macrometastases, per the manufacturer's recommendations. In terms of equivalence to the results obtained by IHC, an OSNA- negative result is consistent with negative histology or with the presence of ITC, which were scored as pN0 and N0(i+), respectively. For comparative analyses, all patients were classified based on their axillary stagings, according to the TNM classification17.
Statistical analysis
All statistical data analyses were performed using IBM SPSS version 21.0 (IBM Corp. 2012) and R software environment (http://www.r-project.org/). To compare the characteristics between the H&E-based IHC and OSNA assays of the patients with tumors and who underwent SLN biopsy, we performed the chi-squared test or Fisher's exact test for categorical variables. An independent samples Student's t-test was used for the continuous variables. Breslow-Day and Tarone's tests were used to test for homogeneity of metastasis detection between the H&E-based IHC and OSNA cohorts. p < 0.05 was considered to be statistically significant.
References
Giuliano, A. E. et al. Improved axillary staging of breast cancer with sentinel lymphadenectomy. Ann. Surg. 222, 394–401 (1995).
Wilson, L. L. & Giuliano, A. E. Sentinel lymph node mapping for primary breast cancer. Curr. Oncol. Rep. 7, 12–17 (2005).
Fleissig, A. et al. Post-operative arm morbidity and quality of life. Results of the ALMANAC randomised trial comparing sentinel node biopsy with standard axillary treatment in the management of patients with early breast cancer. Breast Cancer Res. Treat. 95, 279–293 (2006).
Cserni, G. Intraoperative analysis of sentinel lymph nodes in breast cancer by one-step nucleic acid amplification. J. Clin. Pathol. 65, 193–199 (2012).
Tew, K., Irwig, L., Matthews, A., Crowe, P. & Macaskill, P. Meta-analysis of sentinel node imprint cytology in breast cancer. Br. J. Surg. 92, 1068–1080 (2005).
Layfield, D. M., Agrawal, A., Roche, H. & Cutress, R. I. Intraoperative assessment of sentinel lymph nodes in breast cancer. Br. J. Surg. 98, 4–17 (2011).
Mesker, W. E. et al. Supervised automated microscopy increases sensitivity and efficiency of detection of sentinel node micrometastases in patients with breast cancer. J. Clin. Pathol. 57, 960–964 (2004).
Weaver, D. L. et al. Detection of occult sentinel lymph node micrometastases by immunohistochemistry in breast cancer. An NSABP protocol B-32 quality assurance study. Cancer 107, 661–667 (2006).
Cserni, G. et al. The value of cytokeratin immunohistochemistry in the evaluation of axillary sentinel lymph nodes in patients with lobular breast carcinoma. J. Clin. Pathol. 59, 518–522 (2006).
Weigelt, B. et al. Detection of metastases in sentinel lymph nodes of breast cancer patients by multiple mRNA markers. Br. J. Cancer 90, 1531–1537 (2004).
Gillander, W. E. et al. Molecular detection of micrometastatic breast cancer in histopathology-negative axillary lymph nodes correlates with traditional predictors of prognosis: an interim analysis of a prospective multi-institutional cohort study. Ann. Surg. 239, 828–837 (2004).
Abdul-Rasool, S. et al. An evaluation of molecular markers for improved detection of breast cancer metastases in sentinel nodes. J. Clin. Pathol. 59, 289–297 (2006).
Visser, M. et al. Intra-operative rapid diagnostic method based on CK19 mRNA expression for the detection of lymph node metastases in breast cancer. Int. J. Cancer 122, 2562–2567 (2008).
Tamaki, Y. et al. Molecular detection of lymph node metastases in breast cancer patients: results of a multicenter trial using the one-step nucleic acid amplification assay. Clin. Cancer Res. 15, 2879–2884 (2009).
Tsujimoto, M. et al. One-step nucleic acid amplification for intraoperative detection of lymph node metastasis in breast cancer patients. Clin. Cancer Res. 13, 4807–4816 (2007).
Smith, P. A., Harlow, S. P., Krag, D. N. & Weaver, D. L. Submission of lymph node tissue for ancillary studies decreases the accuracy of conventional breast cancer axillary node staging. Mod. Pathol. 12, 781–785 (1999).
Singletary, S. E. & Connolly, J. L. Staging Manual Breast Cancer Staging: Working With the Sixth Edition of the AJCC. CA Cancer J. Clin. 56, 37–47 (2006).
Goldhirsch, A. et al. Strategies for subtypes-dealing with the diversity of breast cancer: highlights of the St. Gallen International expert consensus on the primary therapy of early breast cancer 2011. Ann. Oncol. 22, 1736–1747 (2011).
Hsu, S. M., Raine, L. & Fanger, H. Use of avidin-biotin-peroxidase complex (ABC) in immunoperoxidase techniques: a comparison between ABC and unlabelled (PAP) procedures. J. Histochem. Cytochem. 29, 577–580 (1981).
Osako, T. et al. Intraoperative Molecular Assay for Sentinel Lymph Node Metastases in Early Stage Breast Cancer A Comparative Analysis Between One-Step Nucleic Acid Amplification Whole Node Assay and Routine Frozen Section Histology. Cancer 117, 4365–4374 (2011).
Tamaki, Y. et al. Routine clinical use of the one-step nucleic acid amplification assay for detection of sentinel lymph node metastases in breast cancer patients: results of a multicenter study in Japan. Cancer 118, 3477–3483 (2012).
Santaballa, A. et al. Advantages of one step nucleic acid amplification (OSNA) whole node assay in sentinel lymph node (SLN) analysis in breast cancer. Springerplus 2, 542 (2013).
Vegué, L. B. et al. Comparison of Molecular Analysis and Histopathology for Axillary Lymph Node Staging in Primary Breast Cancer: Results of the B-CLOSER-I Study. Diagn. Mol. Pathol. 21, 69–76 (2012).
Godey, F. et al. Sentinel lymph node analysis in breast cancer: contribution of one-step nucleic acid amplification (OSNA). Breast Cancer Res. Treat. 131, 509–516 (2012).
Klingler, S. et al. Using one-step nucleic acid amplification (OSNA) for intraoperative detection of lymph node metastasis in breast cancer patients avoids second surgery and accelerates initiation of adjuvant therapy. Ann. Oncol. 24, 2305–2309 (2013).
Lannin, D. How many breast cancer cells in a sentinel lymph node are OK? Ann. Surg. Oncol. 11, 553–534 (2004).
Lyman, G. H. et al. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early stage breast cancer. J. Clin. Oncol. 23, 7703–7720 (2005).
Giuliano, A. E. et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305, 569–575 (2011).
Tiernan, J. P. et al. Systematic review and meta-analysis of cytokeratin 19-based one-step nucleic acid amplification versus histopathology for sentinel lymph node assessment in breast cancer. Br. J. Surg. 101, 298–306 (2014).
Bernet, L. et al. Consensus on sentinel lymph node biopsy in breast cancer. Review of the Spanish Society of Senology and Breast Pathology 2013. Rev. Senol. Patol. Mamar. 27, 43–53 (2014).
Peg, V. et al. Intraoperative molecular analysis of total tumor load in sentinel lymph node: A new predictor of axillary status in early breast cancer patients. Breast Cancer Res. Treat. 139, 87–93 (2013).
Espinosa-Bravo, M. et al. Prediction of non-sentinel lymph node metastasis in early breast cancer by assessing total tumoral load in the sentinel lymph node by molecular assay. Eur. J. Surg. Oncol. 39, 766–773 (2013).
Guillén-Paredes, M. P. et al. [One-step nucleic acid amplification (OSNA) assay for sentinel lymph node metastases as an alternative to conventional postoperative histology in breast cancer: A cost-benefit analysis.]. Cir. Esp. 89, 456–462 (2011).
Francissen, C. M. et al. Evaluation of the Benefit of Routine Intraoperative Frozen Section Analysis of Sentinel Lymph Nodes in Breast Cancer. ISRN Oncol. 2013, 843793 (2013).
Acknowledgements
This work was financially supported by the Ministerio de Ciencia e Innovación (SAF2012-38914), Plan Nacional de I + D + I, MICINN, Spain. The authors also gratefully acknowledge the crucial assistance of the Dr. Josep Trueta registration staff for their help during data collection.
Author information
Authors and Affiliations
Contributions
M.A.R., E.L.-B., M.B. and J.A.M. contributed to study design. M.A.R., E.L.-B., F.T.-R., E.V.-C., E.A. and B.M.-C. contributed to data collection. M.A.R., E.L.B., M.B. and J.A.M. contributed to data analysis. M.B. was responsible for performing statistical analysis. M.A.R and J.A.M. wrote the paper.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Ruano, M., Lopez-Bonet, E., Buxó, M. et al. An improved axillary staging system using the OSNA assay does not modify the therapeutic management of breast cancer patients. Sci Rep 4, 5743 (2014). https://doi.org/10.1038/srep05743
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep05743
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.