Abstract
The aim of this study was to analyse high blood pressure detection, management, control and associated factors among residents accessing community health services (CHSs) in Beijing. We screened for HBP in 9524 individuals aged 50 years or older who accessed care in four Beijing CHSs. Among the 9397 residents with questionnaire responses that qualified them for inclusion in the study, 5029 patients with HBP were identified, 1510 (i.e., 30% of the HBP patient group) of whom were newly identified cases. The rate of hypertension detection was 53.5%. Among the 5029 HBP patients, the rates of awareness, treatment and control of hypertension were 70.0%, 62.1% and 29.6%, respectively. In general, the rate of hypertension control was higher when the rates of hypertension awareness and treatment were higher in subgroups stratified by different sociodemographic and risk factors, except for the overweight and obesity subgroups. In conclusion, suboptimal HBP awareness, treatment and control are still major problems confronting CHSs in Beijing. Control of hypertension in the population may be improved by increasing awareness and improving the treatment of hypertension in CHSs.
Similar content being viewed by others
Introduction
Hypertension is the most important modifiable risk factor for cardio-cerebrovascular diseases. In 2010, high blood pressure (HBP) accounted for 12.0% of disability-adjusted life-years and 24.6% of deaths in China and, after a composite of dietary risk factors, was the second most important risk factor for total disease burden1. Thus, achieving optimal blood pressure (BP) control in patients with HBP is an important objective for the early prevention and control of cardio-cerebrovascular diseases and for decreasing disease burden in China. Epidemiological surveys have shown that the prevalence of hypertension in China has increased from 13.6% in 1991 to 18.8% in 2002, whereas the rates of antihypertensive treatment and control are lower than those in developed countries2,3,4,5,6,7,8,9,10,11,12,13. As part of the healthcare reforms in China, there has been an increasing focus on hypertension prevention and control in community health services (CHSs). Following the release and implementation of Chinese guidelines for the management of hypertension, all CHS centres or stations in Beijing, covering both urban and rural communities, have been involved in the management of hypertension since 200814,15,16,17. These measures have improved the management and control of BP in patients with HBP in the community. However, it is unclear how the measures have affected current detection and management of hypertension in Beijing community residents. One of the main measures of the primary prevention of cardio-cerebrovascular diseases is increasing awareness and treatment of patients with hypertension, thereby achieving optimal BP control. However, there is little information on the factors associated with Hypertension detection, awareness, treatment and control in the Chinese CHS. Therefore, the aim of this study was to improve the prevention and control of HBP in the population by analysing HBP detection, management, control and associated factors in individuals utilising the CHS in Beijing. The study used baseline data from the “Trial on community-based screening and intervention technologies for individuals at high risk of stroke” in “Research on appropriate technologies for community-based stroke prevention and control” granted by the National Key Technology R&D Program during the eleventh “Five-year” plan.
Results
Characteristics of the participants
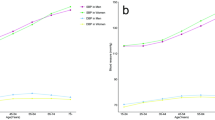
There were 9397 participants (mean age 60.2 ± 7.9 years, 34.8% men) whose questionnaires qualified them for inclusion in this study. The mean SBP and DBP were 129.9 ± 17.9 and 78.3 ± 10.1 mm Hg, respectively. The distributions of SBP and DBP according to age and gender are shown in Figure 1. Significant differences between men and women were found with respect to age, education, marriage, occupation, workload, BMI, smoking, drinking, diabetes, hyperlipidaemia and family history of hypertension, but not with respect to ethnicity or heart disease (table 1).
Hypertension detection, awareness, treatment and control
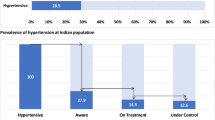
Of the 9397 residents whose questionnaires qualified them for inclusion in this study, 5029 HBP patients were identified, 1510 (30%) of which were new cases, i.e., were first identified in this investigation. The detection rate of hypertension in this community population was 53.5%. Among the 5029 HBP patients, the rates of awareness, treatment and control (SBP < 140 mm Hg and DBP < 90 mm Hg) were 70.0%, 62.1% and 29.6%, respectively. The mean age of the 5029 HBP patients was 61.7 ± 8.1 years and 38.1% were men. The detection rate of hypertension; the percentages of HBP patients who were aware, treated and controlled; and the percentage of treated hypertensive persons who were controlled were different across the different target individuals (table 2).
Sociodemographic characteristics and factors associated with detection, awareness, treatment and control
Figure 2 shows the adjusted odds ratios and 95% confidence intervals for hypertension detection, awareness, treatment and control in different target groups.
Adjusted* odds ratios and 95% confidence intervals for hypertension detection, awareness, treatment and control in different target groups.
*adjusted other different factors including age, gender, ethnicity, education, marriage, occupation, workload, BMI, smoking, drinking, heart disease, diabetes, hyperlipidaemia.
Older age was associated with higher rates of hypertension detection, awareness, treatment and control.
Men had a higher rate of hypertension detection but lower rates of hypertension awareness, treatment and control than women.
No difference was found in the rates of hypertension detection, awareness, treatment and control between the Han and other ethnicities, between married and divorced/widowed/single patients or between employed and retired/housebound patients.
A higher level of education was associated with a lower rate of hypertension detection but a higher rate of hypertension control compared with lower level of education.
Light, mild and moderate workloads were associated with lower rates of hypertension detection than heavy workloads.
Overweight and obesity were associated with higher rates of hypertension detection, awareness and treatment but lower rates of hypertension control than low/normal weight.
Patients who had stopped smoking had higher rates of hypertension detection and treatment compared with regular smokers whereas patients who had never smoked only had a higher rate of hypertension detection.
Patients who were occasional drinkers or never drank had a lower rate of hypertension detection compared with patients who regularly drank. In contrast, patients who never drank had a higher rate of hypertension treatment than other drinkers and patients who had stopped drinking had a higher rate of hypertension control than the other categories of drinkers.
Patients with a family history of hypertension had higher rates of hypertension detection, awareness, treatment and control compared with patients with no or an unknown family history of hypertension. Similar associations were found in patients with heart diseases, diabetes and hyperlipidaemia.
Adherence to drug use and control
The rate of BP control was 45.8% in HBP patients with regular therapy,32.2% in HBP patients with irregular therapy and 3.2% in HBP patients without therapy. In a comparison of HBP patients with regular therapy using a multivariate model, the adjusted OR of BP control was 0.587 (95%CI: 0.476–0.725) in HBP patients with irregular therapy and 0.041 (95%CI: 0.031–0.054) in HBP patients without therapy.
Discussion
The present study indicates that suboptimal HBP awareness, treatment and control in the population are still major problems in the current CHS in Beijing. More than half of the subjects aged 50 years or older had hypertension (53.5%) and 30% of all the HBP patients were newly identified in this study. Of the 5029 HBP patients identified, the proportion who regularly used antihypertensive drugs was 55.4%, whereas the overall rate of hypertension control was 29.6%. When the 1510 new cases were excluded, the proportion of HBP patients who regularly used antihypertensive drugs was 79.3%, whereas the overall rate of optimal BP control was 44.4%. Because the rate of new cases of HBP patients identified decreased with increasing age in our study, if the current CHS program included younger residents in the community, it is likely that the rate of new HBP patients identified among younger residents would be higher than the 30% identified in the present study among elder residents aged 50 years or older. The rates of HBP awareness, treatment and control among HBP patients in our investigation were 70.0%, 62.1% and 29.6%, respectively. These rates were higher than the HBP awareness, treatment and control rates of 30.2%, 24.7% and 6.1%, respectively, found in the 2002 China national survey2 and those found in other studies in China3,4,5,6,7,8,9,20 and in other developing countries21,22, but they were lower than the respective rates of 80.6%, 71.6% and 48.4% in the 2007 to 2008 US National Health and Nutrition Examination Survey13. However, there was no similarity in age, sampling and representativeness between the studies.
In the present study, the non-modifiable sociodemographic and risk factors associated with hypertension detection, awareness, treatment and control included age, gender, education, workload and family history of hypertension but not ethnicity, marriage or occupation.
In the multivariate analysis, we found that old age was independently associated with higher hypertension awareness, treatment and control; this result is consistent with the results of other studies21,23,24.
In this study, men had a higher rate of hypertension detection than women, but they exhibited lower rates of awareness, treatment and control. It is commonly observed both in developed25,26 and developing23,24 countries, that the rates of hypertension awareness, treatment and control are higher in women than in men. In contrast, women aged 50 years or older had a higher prevalence of hypertension than men in Zhejiang, China, possibly due to menopause23. Compared with women, men visit physicians less often, have shorter consultations and tend to see their physicians later in the course of their illness. which may be the reason why women have higher hypertension awareness, treatment and control than men.
Age and gender are not modifiable risk factors of HBP; however, due to their social roles in the community, women and the elderly are not neglected with respect to health education and health promotion for the prevention and control of HBP27.
A higher education level was associated with a lower rate of hypertension detection and an increase in optimal BP control in community HBP patients. Compared with people who have attained a high level of education, people with a lower education level usually have less knowledge about hypertension and consequently live an unhealthier lifestyle. In previous studies23,28,29, a lower education level was associated with poor BP control, which was consistent with the findings of the present study.
As one of the main factors analysed in this study, a family history of hypertension was positively associated with rates of hypertension detection, awareness, treatment and control in our investigation. A family history of hypertension was found to be associated with hypertension among the elderly in Costa Rican30. Optimal BP control was also most likely due to better awareness and treatment of hypertension in HBP patients with a family history of hypertension.
Few studies have documented associations between workload and HBP detection, awareness, treatment and control. In this study, participants with Light, mild and moderate workloads had lower rates of hypertension detection compared with participants with heavy workloads.
Ethnicity, marriage and occupation did not show significant effects on hypertension detection, awareness, treatment and control in the multivariate logistic regression analyses. However, the non-significance of the results does not necessarily mean that the relationship does not exist; it is possible that the sample sizes in some subgroups did not have sufficient power to detect some relationships. For example, with regard to ethnicity, although no significant differences in hypertension detection, awareness, treatment and control between Han and other Chinese ethnicities were found in our study, other studies have documented ethnic differences in the rates of treatment and control31,32,33. Cummings et al found that the probability of African Americans having a BP below the target value of 130/80 mm Hg was 39% lower than the corresponding probability for European Americans in multivariate-adjusted models (<130/80 mm Hg in African Americans vs. European Americans: 30 vs. 43%)31.
In the present study, we found that the modifiable risk factors associated with HBP included Smoking; drinking; overweight or obesity due to physical inactivity; and a history of heart diseases, diabetes or hyperlipidaemia. However, the associations of smoking and drinking with hypertension detection, awareness, treatment and control were unclear. In our investigation, there were no associations between cigarette smoking and hypertension awareness and control in HBP patients, whereas the rate of hypertension detection in participants who had never smoked or had stopped smoking was higher than that in participants who regularly smoked and the rate of treatment of hypertension in HBP patients who had stopped smoking was higher than that in HBP patients who regularly smoked. Indeed, HBP patients who had stopped smoking were more likely to receive hypertension treatment. In Muntner's study, controlled hypertension was more common among individuals who underwent lifestyle modification34. Interestingly, on the contrary, non-smoking women were more likely to have uncontrolled high blood pressure than their smoking counterparts in the Oslo Health Study 2000–200135. In our study, we found that the rate of hypertension detection in participants who never or only occasionally drank was lower than that in participants who regularly drank; furthermore, participants who never drank were more likely to receive hypertension treatment and HBP patients who had stopped drinking were more likely to have their hypertension under control. Previous studies confirmed our findings that patients who regularly drank had a higher rate of HBP detection compared with those patients who never drank whereas there were no differences between these patients groups with respect to the rates of awareness, treatment and control23,24.
Generally, the rate of hypertension control was higher when the rates of hypertension awareness and treatment were higher. However, our findings showed that overweight and obese people were more likely to be aware of and treated for, hypertension but had poorer BP control compared with people with normal/low body weight. Other studies have also shown that overweight or obesity was significantly associated with hypertension and better BP awareness but poorer BP control among hypertensive patients23,36. It has been suggested that overweight and obesity positively influence BP monitoring and the prescription of medication for treatment; thus resulting in higher rates of awareness and treatment. In contrast, overweight or obese patients were less likely to have their BP adequately controlled compared with low/normal weight patients despite their higher awareness and treatment rates. In Czernichow's opinion, poorer BP control in obese HBP patients may have been a consequence of obesity and its complex pathophysiology rather than a consequence of inadequate therapeutic decisions made by clinicians36.
Optimal BP control in HBP patients with co-morbidities is more difficult than that in HBP patients without co-morbidities; however, optimal BP control rates in HBP patients with co-morbidities were seemingly higher than those in HBP patients without co-morbidities in the CHS. Similarly, awareness of known heart diseases, diabetes and hyperlipidaemia was associated with a higher probability of awareness, treatment and control of HBP. The rates of unknown histories of hyperlipidaemia, heart diseases and diabetes among the 5029 HBP patients investigated were 19.2%, 7.3% and 5.2%, respectively; the rates of optimal BP control in these groups of HBP patients were lower than those in the group of HBP patients with clear (yes or no) histories of diseases, implying that awareness of co-morbidities is important for facilitating optimal BP control in community HBP patients. Similar findings were observed in the Oslo Health Study 2000–2001 and the presence of cardiovascular disease or diabetes and the prescription of cholesterol-lowering statins were independently associated with better control of BP35.
The potential reasons for inadequate BP control are numerous and include not only insufficient patient knowledge but also biological resistance, patient lifestyle/behavioural choices, comorbid conditions and treatments, non-adherence to medication, inadequate access to health care, discrimination by race and gender, failure to adopt BP guidelines and lack of treatment intensification31,37. Asides from these sociodemographic and risk factors, drug adherence is also an important factor for optimal BP control. Joshi et al observed that drug non-compliance may help explain poor BP control in patients undergoing treatment for hypertension38. Bosworth et al. found that African Americans in the Veterans Administration system were 81% more likely than European Americans to be nonadherent to medications for BP control38. Safford et al found that African American hypertensive subjects were more likely to have a more intense antihypertensive regimen than European Americans across all age and income groups but were still more likely to have elevated blood pressure values, suggesting the presence of medication nonadherence and/or treatment resistance39. We also observed that BP control in patients who regularly use their antihypertensive drugs was better than that in patients who Intermittently/occasionally use antihypertensive drugs. In addition, only approximately 60% of HBP patients who were investigated regularly took their antihypertensive medicine, implying that gaps in drug compliance could also be improved.
Unlike previous observational studies, this was a community-based study that screened individuals at high risk for stroke and included hypertension detection. The present study has limitations, including its cross-sectional design; the use of self-reported disease and medication adherence measures; limited study factors for exploring associations with HBP detection, awareness, treatment and optimal control; and the use of an identical BP control target for HBP patients with co-morbidities and elderly HBP patients. We were unable to collect information on the type of and compliance with antihypertensive therapy and to identify secondary and/or resistant hypertension in HBP patients. In addition, as only a quarter of the individuals in the communities participated in our investigation and there were different responses between subgroups (e.g., gender), our results could be overestimated or underestimated. However, our findings suggest that the detection, treatment/management and control of hypertension can be further improved.
In conclusion, suboptimal HBP awareness, treatment and control are still major problems associated with the current CHS in Beijing. The associations of HBP awareness, treatment and control with most sociodemographic and risk factors indicate that the control of hypertension in populations can be improved by increased awareness and treatment of hypertension in the course of CHS care. However, the mechanisms of some sociodemographic and risk factors associated with the inconsistency between hypertension awareness, treatment and control in different subgroups of patients should be further expected in future studies.
Methods
Subjects
Using a quasi-experimental community trial design, 4 communities with a total population of approximately 100,000 people, who received care at 4 Beijing CHS Centres (or Stations), were defined. These centres were the Yongwai CHS Centre and the Tiyuguanlu CHS Centre in the Dongcheng (previously Chongwen) District, as well as the Pingguoyuan CHS Centre and the Xihuangcun CHS Station affiliated with the Capital Steel Hospital in the Shijingshan District. A total of 37626 individuals aged 50 years or older were identified and accounted for 41.14% of the 91453 residents in the defined communities. Patients with stroke or residents who refused to participate were excluded from the study. A total of 9524 individuals aged 50 years or older participated in the study for identifying individuals at high risk of stroke, accounting for 25.3% of the 37626 targeted residents. A total of 9397 individuals had questionnaire responses that qualified them for inclusion in the analysis.
Ethics statement
This study was approved by the Ethics Committee of the Beijing Tiantan Hospital affiliated with the Capital Medical University, shared by the Beijing Neurosurgical Institute and written informed consent was obtained from all participants. The study was performed in accordance with approved guidelines.
Survey method and content
Face-to-face interviews and physical examinations were performed on subjects according to the questionnaire used in the selected CHS centres between May and December in 2008; the questionnaire was designed by medical and research staff from the Beijing Neurosurgical Institute. The survey content included questions regarding age; gender; race; education; marriage; occupation; workload; smoking; drinking; family history of hypertension; histories of hypertension, heart disease, diabetes mellitus and dyslipidemia; and BP, height and weight measurements and Cerebral Vascular Hemodynamic Index (CVHI) derived from physical examination18.
Workload was classified into light, mild, moderate and severe levels according to the daily work activities as follows: light covering sedentary work (e.g., reading, writing, performing office work and assembling and repairing watches and radios) that does not require strenuous muscle activity; mild covering standing work that can include walking, or sedentary work requiring no intense muscle activity (e.g., teaching, conducting laboratory work, typing, operating a computer and performing sales assistant duties); moderate covering work that requires more intense muscle activity (e.g., performing the daily activities of students, driving a vehicle, or performing electrical installation, metal cutting or woodworking); and severe covering occupations such as steelmaking, lathe operation, dancing and sports. Smoking was categorised as regular smoking (i.e. more than one cigarette per day for more than 6 months), occasional smoking, quit smoking (had not smoked for more than 6 months) and never smoked. Similarly, drinking was divided into regular drinking (≥once a week), occasional drinking, quit drinking (had not had an alcoholic drink for more than 6 months) and never drank.
Hypertension was defined as having a history of hypertension, or taking antihypertensive medication in the recent 2 weeks, having a systolic blood pressure (SBP) ≥ 140 mm Hg or having a diastolic blood pressure (DBP) ≥ 90 mm Hg. The use of antihypertensive drugs in the past year (i.e., adherence to medication) was divided into regular use (more than 9 months during the past year), intermittent use (more than 6 months in the past year), occasional use (less than 6 months in the past year) and never used. The heart diseases inquiries included coronary heart disease, hypertensive heart disease, rheumatic heart disease and atrial fibrillation. Histories of heart disease, diabetes and hyperlipidaemia were categorised as yes, no or unknown according to the patients' self-reports.
BP was measured twice in the right arm in the seated position with a mercury sphygmomanometer after the participant had been seated for 5 minutes. The average of the two readings was used in the analysis. Weight was measured to the nearest 0.1 Kg using weight scales with participants wearing light clothing without shoes. Height was measured to the nearest 0.1 cm using a stadiometer with shoes removed. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Overweight and obesity were defined as 24 ≤ BMI<28 and BMI ≥ 28, respectively, according to the recommended standard Chinese thresholds for overweight and obesity19. Data on CVHI evaluation were not used in this study and were therefore omitted from the analysis.
Statistical analysis
The detection rate of hypertension in the community population was the rate of the detected community patients with hypertension among the community residents who were actually screened. New cases were defined as HBP patients who were first identified in this study. The rates of hypertension awareness, treatment and control were the percentages of HBP patients who were aware, treated and controlled (i.e., SBP < 140 mm Hg and DBP < 90 mm Hg), respectively, among all HBP patients detected in the community. The control rate of treated hypertensive patients was the rate of HBP patients with SBP < 140 mm Hg and DBP < 90 mm Hg among all HBP patients in the community who had been treated in the past two weeks.
The characteristics of male vs. female subjects were compared by using the chi square test. The rates of hypertension detection, awareness, treatment and control in the subgroups of different factors were calculated and compared by non-conditional binary logistic regression after adjusting for different factors including age group, gender, ethnicity, education, marriage, occupation, workload, BMI, smoking, drinking, family history of hypertension, heart disease, diabetes and hyperlipidaemia in a multivariate model. Given the relationship between HBP control and drug adherence, the association between antihypertensive treatment in the past year and control was further analysed by introducing the antihypertensive treatment into the multivariate model. All statistical calculations were performed using SPSS 13.0 software (SPSS Inc. Chicago, IL, USA). P < 0.05 was considered statistically significant.
References
Yang, G. et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 381, 1987–2015 (2013).
Wu, Y. et al. Prevalence, Awareness, Treatment and Control of Hypertension in China. Data from the China National Nutrition and Health Survey 2002. Circulation 118, 2679–2686 (2008).
Gu, D. et al. Prevalence, Awareness, Treatment and Control of Hypertension in China. Hypertension 40, 920–927 (2002).
Zhao, Y. et al. Trends in Population Blood Pressure and Prevalence, Awareness, Treatment and Control of Hypertension among Middle-Aged and Older Adults in a Rural Area of Northwest China from 1982 to 2010. PLoS ONE 8, e61779. 10.1371/journal.pone.0061779 (2013).
Zhao, Y. et al. Trends in Hypertension Prevalence, Awareness, Treatment and Control Rates in Shandong Province of China. J. Clin. Hypertens. 14, 637–643 (2012).
Li, H. et al. Prevalence, awareness, treatment and control of hypertension in rural China: results from Shandong Province. J. Hypertens. 28, 432–438 (2010).
Yang, J. et al. Prevalence of prehypertension and hypertension in a Chinese rural area from 1991 to 2007. Hypertens. Res. 33, 331–337 (2010).
Xi, B. et al. Trends in prevalence, awareness, treatment and control of hypertension among Chinese adults 1991–2009. Int. J. Cardiol. 158, 326–329 (2012).
Meng, X. J. et al. Prevalence, awareness, treatment, control and risk factors associated with hypertension in urban adults from 33 communities of China: the CHPSNE study. J. Hypertens. 29, 1303–1310 (2011).
Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Arch. Intern. Med. 157, 2413–2446 (1997).
Meissner, I. et al. Detection and Control of High Blood Pressure in the Community Do We Need a Wake-Up Call? Hypertension 34, 466–471 (1999).
Egan, B. M., Zhao, Y. & Axon, R. N. US Trends in Prevalence, Awareness, Treatment and Control of Hypertension, 1988–2008. JAMA 303, 2043–2050 (2010).
Yoon, S. S., Ostchega, Y. & Louis, T. Recent Trends in the Prevalence of High Blood Pressure and its Treatment and Control, 1999–2008. NCHS Data Brief 48, 1–8 (2010).
Liu, L. S. & Gong, L. S. Writing Group of Chinese Guidelines for the Management of Hypertension. 1999 Chinese guidelines for the management of hypertension. Chin. J Hypertens. 8, 94–104 (2000).
Liu, L. S. National Revision Committee for the Guidelines on Prevention and Control of Hypertension in China. Prevention and treatment of hypertension in community. The Guidelines On Prevention And Control Of Hypertension In China. Liu, L. S. (ed.) Beijing: People's Medical Publishing House. 49–51p (2006).
Liu, L. S. Writing Group of 2010 Chinese Guidelines for the Management of Hypertension. 2010 Chinese guidelines for the management of hypertension. Chin. J. Cardiovasc. Dis. 39, 579–615 (2011).
Jiang, B. et al. Investigation of prevention and treatment capabilities of stroke recurrence in general practitioners and nurses in Beijing Communities. Chin. Gen. Pract. 12, 1134–7 (2009).
Huang, J. et al. Evaluation of the relative risk of stroke in patients with hypertension using cerebrovascular hemodynamic accumulative scores. Chin. J. Cerebrovasc. Dis. 3, 537–541 (2006).
Cooperative Meta-analysis Group of China Obesity Task Force. Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population. Chin. J. Epidemiol. 23, 5–10 (2002).
Ahn, S., Smith, M. L., Cho, J., Bailey, J. E. & Ory, M. G. Hypertension Awareness and Associated Factors among Older Chinese Adults. Front. Public Health 1: 67. 10.3389/fpubh.2013.00067.eCollection 2013 (2013). (Date of access:19/02/2014).
Duboz, P., Boëtsch, G., Gueye, L. & Macia, E. Hypertension prevalence, awareness, treatment and control in Dakar (Senegal). J. Hum. Hypertens. 10.1038/jhh.2013.142 (2014). (Date of access:19/02/2014).
Kiau, B. B. et al. Prevalence, awareness, treatment and control of Hypertension among the elderly: the 2006 National Health and Morbidity Survey III in Malaysia. Med. J. Malaysia 68, 332–7 (2013).
Wang, H. et al. Factors Associated with Prevalence, Awareness, Treatment and Control of Hypertension among Adults in Southern China: A Community-Based, Cross-Sectional Survey. PLoS ONE 8, e62469. 10.1371/journal.pone.0062469 (2013).
Agyemang, C., Bruijnzeels, M. A. & Owusu-Dabo, E. Factors associated with hypertension awareness, treatment and control in Ghana, West Africa. J. Hum. Hypertens. 20, 67–71 (2006).
Wyatt, S. B. et al. Prevalence, awareness, treatment and control of hypertension in the Jackson Heart Study. Hypertension 51, 650–656 (2008).
Meisinger, C. et al. Regional disparities of hypertension prevalence and management within Germany. J. Hypertens. 24, 293–299 (2006).
Jiang, B. et al. Evaluation of Health Education on Prevention of Cerebrovascular Diseases in the Community Population. Chin. J. Clin. Rehabil. 8, 171–173 (2004).
Veghari, G. et al. Impact of literacy on the prevalence, awareness, treatment and control of hypertension in adults in Golestan Province (northern Iran). Caspian J. Intern. Med. 4, 580–4 (2013).
Wu, Y. et al. Risk factors associated with hypertension awareness, treatment and control in a multi-ethnic Asian population. J. Hypertens. 27, 190–197 (2009).
Méndez-Chacón, E., Santamaría-Ulloa, C. & Rosero-Bixby, L. Factors associated with hypertension prevalence, unawareness and treatment among Costa Rican elderly. BMC Public Health 8, 275. 10.1186/1471-2458-8-275 (2008).
Cummings, D. M. et al. Blood Pressure Control in Diabetes. Temporal progress yet persistent racial disparities: national results from the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Diabetes Care 33, 798–803 (2010).
Lane, D. A. & Lip, G. Y. H. Ethnic differences in hypertension and blood pressure control in the UK. Q. J. Med. 94, 391–396 (2001).
Shelley, D. et al. Predictors of blood pressure control among hypertensives in community health centers. Am. J. Hypertens. 24, 1318–23 (2011).
Muntner, P. et al. Factors associated with hypertension awareness, treatment and control in a representative sample of the Chinese population. Hypertension 43, 578–585 (2004).
Tonstad, S., Furu, K., Rosvold, E. O. & Skurtveit, S. Determinants of control of high blood pressure. The Oslo Health Study 2000–2001. Blood Pressure 13, 343–349 (2004).
Czernichow, S. et al. Determinants of blood pressure treatment and control in obese people: evidence from the general population. J. Hypertens. 30, 2338–44 (2012).
Bosworth, H. B. et al. Racial differences in blood pressure control: potential explanatory factors. J. Gen. Intern. Med. 23, 692–8 (2008).
Joshi, P. P., Salkar, R. G. & Heller, R. F. Determinants of poor blood pressure control in urban hypertensives of central India. J. Hum. Hypertens. 10, 299–303 (1996).
Safford, M. M. et al. Understanding racial disparities in hypertension control: intensity of hypertension medication treatment in the REGARDS study. Ethnic Dis. 17, 421–6 (2007).
Acknowledgements
We thank all of the physicians and medical workers in the Yongwai CHS Centre and the Tiyuguanlu CHS Centre in the Dongcheng (previously Chongwen) District, the Pingguoyuan CHS Centre and the Xihuangcun CHS Station affiliated with the Capital Steel Hospital in the Shijingshan District. Who were involved in this study. We also wish to thank Director Changxia Duan, Ms Xiaoli Liu and Mr Feng Liu of the local health authority for CHS organisation and community mobilisation. This study was funded by the Ministry of Science and Technology and the Ministry of Health of the People's Republic of China under grant nos. 2007BAI24B03 and 2011BAI08B01 of the National Key Technology R&D Program.
Author information
Authors and Affiliations
Contributions
B.J., H.L., X.R. and H.Z. carried out the field works, data collection and analysis. B.J., S.W. and W.W. designed the study and directed its implementation. B.J. performed the statistical analysis and manuscript writing. All contributors discussed the findings and approved the final version for publication.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. The images in this article are included in the article's Creative Commons license, unless indicated otherwise in the image credit; if the image is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the image. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
JIANG, B., LIU, H., RU, X. et al. Hypertension Detection, Management, Control and Associated Factors Among Residents Accessing Community Health Services In Beijing. Sci Rep 4, 4845 (2014). https://doi.org/10.1038/srep04845
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep04845
This article is cited by
-
Prevalence, Awareness, Treatment, and Control of Hypertension among Kazakhs with high Salt Intake in Xinjiang, China: A Community-based Cross-sectional Study
Scientific Reports (2017)
-
SLCO1B1 Variants and Angiotensin Converting Enzyme Inhibitor (Enalapril) -Induced Cough: a Pharmacogenetic Study
Scientific Reports (2015)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.