Abstract
Hypoxia-inducible factor 1 (HIF-1) has been associated with distant tumor metastasis; however, its function in multiple metastatic processes has not yet been fully elucidated. In the present study, we demonstrated that cancer cells transiently upregulated HIF-1 activity during their metastatic colonization after extravasation in the lungs in hypoxia-independent and reactive oxygen species (ROS)-dependent manners. Transient activation induced the expression of lactate dehydrogenase A and phosphorylation of the E1α subunit of pyruvate dehydrogenase, which indicated the reprogramming of glucose metabolic pathways from mitochondrial oxidative phosphorylation to anaerobic glycolysis and lactic acid fermentation. The administration of the HIF-1 inhibitor, YC-1, inhibited this reprogramming, increased intratumoral ROS levels and eventually suppressed the formation of metastatic lung tumors. These results indicate that HIF-1-mediated metabolic reprogramming is responsible for the survival of metastatic cancers during their colonization in lungs by reducing cytotoxic ROS levels; therefore, its blockade by HIF-1-inhibitors is a rational strategy to prevent tumor metastasis.
Similar content being viewed by others
Introduction
Distant tumor metastasis frequently occurs in cancer patients and is responsible for more than 90% of cancer-related deaths. Metastasis is sequentially regulated at multiple steps1. Cancer cells acquire an invasive phenotype in the first phase of the metastatic cascade through the so-called epithelial to mesenchymal transition (EMT)2,3, locally invade blood vessels by degrading the extracellular matrix (ECM)4, internalize into the microvasculature of the lymph and blood systems (known as intravasation)4 and then translocate to distant organs through the circulation5. In the second phase, cancer cells are recruited to the so-called premetastatic niche in foreign tissues6,7,8, extravasate from the bloodstream4, adapt to the microenvironments of distant tissues, actively proliferate and eventually form macroscopic secondary tumors (known as colonization)1. Accumulating evidence has revealed that cancer cells in the hypoxic regions of primary tumors acquire the ability to facilitate both the first phase of the metastatic cascade and formation of the premetastatic niche in distant tissues by activating hypoxia-inducible factor 1 (HIF-1)3,6,7,8.
HIF-1 is a heterodimeric transcription factor composed of an α-subunit (HIF-1α) and β-subunit (HIF-1β)9. The expression of HIF-1α is mainly regulated at the posttranslational level in an oxygen-dependent manner and is largely responsible for the regulation of HIF-1 activity10. A previous study showed that proline residues in the oxygen-dependent degradation domain of HIF-1α, P402 and P564, were hydroxylated under normoxic conditions in oxygen-, Fe2+- and α-ketoglutarate-dependent manners11. This hydroxylation was showed to trigger the ubiquitination and subsequent proteolysis of HIF-1α by E3 ubiquitin-protein ligases containing the von Hippel-Lindau tumor suppressor protein (pVHL) and 26S proteasome, respectively11. On the other hand, the rate at which proline residues are hydroxylated is known to decrease under hypoxic conditions, resulting in a reduced rate of ubiquitination and degradation11. In addition, ROS-mediated decreases in intracellular Fe2+ levels through its oxidization to Fe3+ have been also shown to increase the stability of HIF-1α, even under normoxic conditions. Stabilized HIF-1α interacts with the constitutively expressed HIF-1β protein, binds to its cognate enhancer sequence, hypoxia-response element (HRE)12,13 and induces the expression of more than 800 genes. Some of the HIF-1 downstream genes have been reported to play roles in improving oxygen availability (angiogenesis)14,15,16, shifting glucose metabolism from mitochondrial oxidative phosphorylation to anaerobic glycolysis and lactic acid fermentation (metabolic reprogramming)17 and tumor recurrence after radiation therapy18,19,20,21,22. Recent studies have also demonstrated that HIF-1 plays critical roles in the first phase of the metastatic cascade3,6,7,8. On the other hand, little is known about the involvement of HIF-1 in the second phase of the metastatic cascade, especially in the colonization of metastatic cancers in distant tissues.
In the present study, we demonstrated the importance of HIF-1-mediated metabolic reprogramming in the pulmonary colonization of metastatic cancers. HIF-1 activity was transiently upregulated in ROS-dependent and hypoxia-independent manners in metastatic cancer cells several days after their recruitment to the lungs. Active HIF-1 induced the reprogramming of glucose metabolism from oxidative phosphorylation to anaerobic glycolysis, leading to a decrease in cytotoxic ROS levels, which subsequently contributed to both the survival of metastatic cancer cells and eventual formation of metastatic tumors in the lungs.
Results
Transient upregulation of HIF-1 activity during the metastatic colonization of cancers in the lungs
We used a mouse model of pulmonary metastases, in which a suspension of cancer cells was intravenously injected into athymic nude mice, to analyze the function of HIF-1 in the metastatic colonization of cancers in the lungs (Supplementary Fig. S1,S2). We then developed a novel strategy to quantitatively analyze changes in HIF-1 activity during metastatic colonization, which enabled us to simultaneously monitor both the volume of and HIF-1 activity in metastatic tumors in the lungs without sacrificing mice.
We first established a stable transfectant of the murine mammary carcinoma cell line, EMT6 with a plasmid that constitutively expressed Cypridina luciferase (CLuc) from the cytomegalovirus (CMV) promoter (EMT6/CMVp-CLuc herein). Because the CLuc protein was previously reported to be secreted from mammalian cells after its translation, we expected that the metastatic tumor volume in the lungs could be quantified as CLuc activity in the serum. After seeding EMT6/CMVp-CLuc cells in vitro, we detected specific CLuc activity in the culture medium (Fig. 1a). CLuc activity was positively correlated with the number of EMT6/CMVp-CLuc cells seeded in each culture dish (Fig. 1b; R2 = 0.9421). After the subcutaneous transplantation of EMT6/CMVp-CLuc cells into the right hind legs of athymic nude mice, CLuc activity in the serum gradually increased over time as the xenografted tumor grew (Fig. 1c,d). CLuc activity was positively correlated with xenografted tumor volume, which was measured with calipers (Fig. 1e; R2 = 0.8072). CLuc activity in the serum was positively correlated with the number of metastatic colonies in the lungs after the i.v. transplantation of EMT6/CMVp-CLuc (Fig. 1f; R2 = 0.8431). Moreover, metastatic tumors were only detected in the lungs after the i.v. transplantation of EMT6 derivatives constitutively expressing firefly luciferase, which indicated that no tumors other than pulmonary metastases grew after the transplantation (Supplementary Fig. S3). These results indicated that EMT6/CMVp-CLuc cells can be used to quantitatively monitor increases in metastatic tumor volume as CLuc activity in the serum in the mouse model of pulmonary metastases.
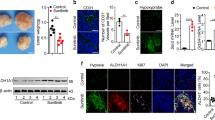
Transient upregulation of HIF-1 activity during the metastatic colonization of cancers in the lungs.
(a,b) Twenty-four hours after seeding EMT6 (a) and EMT6/CMVp-CLuc (a,b) cells (1 × 104 cells in 100 μL culture medium per one well of a 24-well plate), 10 μL culture medium was subjected to the CLuc assay. Means ± s.d. n = 3. **P < 0.01. (c,d) After the subcutaneous transplantation of EMT6/CMVp-CLuc cells, tumor growth and CLuc activity in the serum were monitored by measuring the tumor volume with calipers (c) and by performing the in vivo CLuc assay (d), respectively. Means ± s.d. n = 10. (e) Positive correlation between CLuc activity in the serum and the volume of subcutaneous tumor xenografts measured with calipers. (f) The relationship between CLuc activity in the serum and the number of metastatic colonies in the lungs was analyzed in 20 independent mice 10 days after the i.v. transplantation of EMT6/CMVp-CLuc cells. (g) EMT6/CMVp-CLuc/5HREp-FLuc cells (1 × 104 cells/well in 24-well plate) were cultured under normoxic (20% O2) or hypoxic (0.02% O2) conditions for 24 hours and harvested for the firefly luciferase assay. Means ± s.d. n = 3. **P < 0.01. (h) On the indicated days after the i.v. transplantation of EMT6/CMVp-CLuc/5HREp-FLuc cells (1 × 106/mouse), mice were subjected to optical in vivo imaging using the IVIS SPECTRUM system to externally monitor HIF-1 activity in metastatic lung tumors as FLuc bioluminescence (SeeSupplementary Fig. S4a). Ten μL of serum was simultaneously harvested from mice and subjected to the in vivo CLuc assay to monitor the volume of metastatic tumors (SeeSupplementary Fig. S4b). HIF-1 activity in lung metastases was divided by CLuc activity in the serum to calculate HIF-1 activity per unit of metastatic lung tumors. Means ± s.d. n = 10. *P < 0.05.
To simultaneously monitor changes in intratumoral HIF-1 activity in the animal model, EMT6/CMVp-CLuc cells were then subjected to additional stable transfection with the 5HREp-luc reporter gene, which expressed the firefly luciferase protein (FLuc) under the control of a HIF-1-dependent 5HRE promoter (5HREp). The resultant EMT6/CMVp-CLuc/5HREp-FLuc cells specifically expressed firefly luciferase bioluminescence under hypoxic conditions in vitro (Fig. 1g); therefore, these cells were useful in an optical in vivo imaging experiment for HIF-1 activity, as reported previously23.
Athymic nude mice were intravenously injected with EMT6/CMVp-CLuc/5HREp-FLuc cells to analyze changes in HIF-1 activity per unit of tumor volume during the metastatic colonization of cancers in the lungs. Optical in vivo imaging revealed a gradual increase in HIF-1 activity in lung metastases after the transplantation (Supplementary Fig. S4a). On the other hand, an in vivo CLuc assay revealed the marked acceleration in the growth of pulmonary metastases from 6 to 7 days after the transplantation (Supplementary Fig. S4b). Collectively, HIF-1 activity per unit of metastatic tumor volume, which was calculated as the ratio of HIF-1 activity to CLuc activity in the serum, peaked approximately 6 days after the transplantation and subsequently decreased thereafter. (Fig. 1h).
ROS-mediated transient activation of HIF-1 during metastatic colonization of cancers in the lungs
We next investigated the mechanism underlying the transient upregulation of HIF-1 activity in the mouse model of pulmonary metastasis. HIF-1 activity is known to be mainly regulated through oxygen-dependent modifications in the HIF-1α subunit, such as PHDs-VHL-mediated proteolysis and the FIH-1-mediated inhibition of transactivating activity; therefore, we first examined the status of tumor hypoxia during pulmonary metastases after an intravenous injection of cancer cells. Lungs with metastatic tumors were surgically excised 90 minutes after an intraperitoneal injection of the hypoxia marker, pimonidazole, 5, 6 and 7 days after the i.v. transplantation of the tumor cell suspension. Immunohistochemical analyses with anti-pimonidazole and anti-CD31 antibodies demonstrated that there was no detectable hypoxic region and also that metastatic colonies were adequately oxygenated over time because of a well-organized vascular network (Fig. 2a).
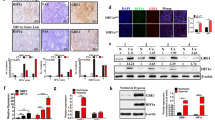
ROS-mediated transient activation of HIF-1 during the metastatic colonization of cancers in the lungs.
(a) Tumor hypoxia (pimonidazole; green) and CD31 (red) were detected on the indicated days after the i.v. transplantation of EMT6/CMVp-CLuc/5HREp-FLuc cells in the lungs with the resultant metastatic tumors (dotted line). Hoechst33342 = counter staining (blue). Bar = 50 μm. (b) On the indicated days after the i.v. transplantation of cancers, oxidative stress in methacarn-fixed paraffin-embedded sections (upper) and formalin-fixed paraffin-embedded sections (lower) of the lungs with the resultant metastatic tumors were detected by the Protein Carbonyls Immunohistochemical Staining Kit (upper) and anti-phospho-p38 antibody (lower), respectively. Bar = 500 μm (upper) and 20 μm (lower). (c–e) EMT6/CMVp-CLuc/5HREp-FLuc cells were cultured with (+) or without (−) N-acetylcysteine (NAC) under 3% oxygen conditions for 24 hours or under 3% oxygen conditions for 18 hours followed by 15% oxygen conditions for 6 hours and were then treated with the ROS marker, DCFH-DA, for flow cytometric analysis (c), subjected to Western blotting for protein carbonyls as the markers of oxidative stress (upper) and for β-actin (lower) (d) and subjected to the firefly luciferase assay for HIF-1 activity (e). A representative data set from 3 independent experiments is shown (c). Means ± s.d, n = 3, **P < 0.01 (e). (f–h) Athymic nude mice were i.v. transplanted with a suspension of EMT6/CMVp-CLuc/5HREp-FLuc cells (1 × 106/mouse) and treated with NAC (1,000 mg/kg) or saline (control) twice a day from 1 to 5 days after the transplantation. Six days after the transplantation, mice were subjected to the in vivo CLuc assay in the serum for tumor volume (f) and to the optical in vivo imaging experiment for HIF-1 activity (g). HIF-1 activity in lung metastases was divided by the CLuc activity in the serum to calculate HIF-1 activity per unit of metastatic lung tumors (h). Means ± s.d. n = 10. *P < 0.05. **P < 0.01. NS = not significant.
We examined the involvement of ROS in the activation of HIF-1 because ROS were previously shown to oxidize Fe2+ to Fe3+, decrease intracellular Fe2+ levels and induce HIF-1 activity, even under normoxic conditions, because Fe2+ is essential for the prolyl hydroxylation of HIF-1α by PHDs. We first analyzed changes in ROS levels in the mouse model of pulmonary metastases. Methacarn-fixed paraffin-embedded sections of lungs with metastatic tumors were subjected to immunohistochemical staining to detect protein carbonyls as the typical markers of oxidative stress24 because ROS have been shown to oxidize arbitrary proteins and generate protein carbonyls25,26. The staining experiment for protein carbonyls revealed high levels of ROS in metastatic colonies concomitant with the peak in HIF-1 activity per unit of tumor volume 6 days after the i.v. transplantation of cancer cells (compareFig. 2b upper to Fig. 1h). In addition, immunohistochemical analysis for phospho-p38 as a marker of the cellular response to oxidative stress27,28,29 also showed that intratumoral ROS levels peaked on day 6 and decreased the following day (Fig. 2b lower). Because previous studies have clearly demonstrated that reoxygenation causes ROS30,31,32, these results led to the following hypothesis; circulating cancer cells, which were under relatively low oxygen conditions in the peripheral blood, were exposed to a well-oxygenated environment after recruitment to the lungs and that such a change in the surrounding oxygen status increased ROS levels, resulting in the activation of HIF-1. This was supported by the results of in vitro experiments in which the reoxygenation of cells from 3%, which is equivalent to the partial oxygen pressure (pO2) of peripheral blood (pO2 = 20–30 mmHg), to 15%, equivalent to that of the lungs (pO2 = approximately 100 mmHg), caused the production of ROS (Fig. 2c,d) and induced HIF-1 activity (Fig. 2e) in a NAC-sensitive manner.
To determine the importance of ROS in the transient activation of HIF-1 in metastatic tumors in vivo, we treated mice with NAC and performed both the optical imaging experiment and in vivo CLuc assay 6 days after the i.v. transplantation of EMT6/CMVp-CLuc/5HREp-FLuc cells. Although the tumor-suppressing effect of NAC was not observed in the in vivo CLuc assay (Fig. 2f), its HIF-1-blocking activity was detected at this time point (Fig. 2g); collectively, these results demonstrated that the NAC treatment significantly suppressed the transient increase in HIF-1 activity per unit of tumor volume 6 days after the transplantation (Fig. 2h). Taken together, these results indicate that increased level of intracellular ROS in well-oxygenated conditions, but not hypoxia, was a causative factor of the transient upregulation of HIF-1 activity during the metastatic colonization of cancers in the lungs.
HIF-1-mediated metabolic reprogramming during metastatic colonization of cancers in the lungs
We investigated the function of the ROS-mediated activation of HIF-1 during the metastatic colonization of cancers. HIF-1 is known to induce metabolic reprogramming from oxidative phosphorylation to anaerobic glycolysis and lactic acid fermentation by inducing numerous genes, such as lactate dehydrogenase A (LDHA) and pyruvate dehydrogenase kinase 1 (PDK1). This reprogramming is reported to be important for cancer cells not only to earn more ATP, but also to reduce cytotoxic ROS levels by decreasing the activity and mass of mitochondria. Based on these findings, we hypothesized that the transient activation of HIF-1 may have induced metabolic reprogramming to decrease intracellular ROS levels for the survival of metastatic cancer cells. To examine this possibility, we first investigated whether transient upregulation induced metabolic reprogramming. We surgically excised lungs with metastatic tumors 5 and 6 days after the i.v. transplantation of tumor cells and performed immunohistochemical analyses against the markers of metabolic reprogramming, LDHA and the phosphorylated form of PDH-E1α. The staining experiments demonstrated that the expression of LDHA, which catalyzes lactic acid fermentation, was higher 6 days after than 5 days after the transplantation, which indicated the induction of the final step of anaerobic glycolysis (Fig. 3a). We also revealed that the phosphorylation of PDH-E1α was induced at the same time point (Fig. 3a). Because phosphorylated PDH-E1α is an inactive form that loses its ability to convert cytosolic pyruvate to acetyl-CoA, an increase in phosphorylation indicates a restriction in the supply of acetyl-CoA to the Krebs cycle. These results were consistent with our expectation that glucose metabolism shifted to anaerobic glycolysis and lactic acid fermentation at this time point. We then treated mice with the antioxidant, NAC and HIF-1 inhibitor, YC-1 to establish whether the ROS-mediated transient activation of HIF-1 was responsible for metabolic reprogramming. The NAC treatment, which significantly inhibited the ROS-mediated activation of HIF-1 in vivo (Fig. 2h), almost completely suppressed the induction of LDHA and phosphorylation of PDH-E1α, which indicated the critical role of ROS in metabolic reprogramming on day 6 (Fig. 3a). The YC-1 treatment, which exhibited no significant tumor-suppressing effect (Fig. 3b) but inhibited the induction of HIF-1 activity per unit of tumor volume on day 6 (Fig. 3c,d), also abrogated reprogramming (Fig. 3a). These results clearly demonstrated that the ROS-mediated activation of HIF-1 directly induced metabolic reprogramming from oxidative phosphorylation to both anaerobic glycolysis and lactic acid fermentation during the metastatic colonization of cancer in the lungs.
HIF-1-mediated metabolic reprogramming during the metastatic colonization of cancers in the lungs.
(a) Athymic nude mice were i.v. transplanted with a suspension of the stable transfectant, EMT6/CMVp-Cluc/5HREp-Luc (1 × 106/mouse). Tumor-bearing mice were treated with saline (-), NAC (1,000 mg/kg/administration, 2 injections/day from days 1 to 6), or YC-1 (30 mg/kg daily from days 3 to 6). On the indicated days after the i.v. transplantation, LDHA (green) and p-PDH-E1α (red) were detected in the lungs with the resultant metastatic tumors (dotted line). Hoechst33342 = counter staining (blue). Bar = 50 μm. (b–d) Athymic nude mice were i.v. transplanted with a suspension of EMT6/CMVp-CLuc/5HREp-FLuc cells and treated with or without the HIF-1 inhibitor, YC-1 (30 mg/kg daily) from 3 to 6 days after the transplantation of cancer cells. Six days after the transplantation, mice were subjected to the in vivo CLuc assay for tumor volume (b) and to the optical in vivo imaging experiment for HIF-1 activity (c). HIF-1 activity in lung metastases was divided by CLuc activity in the serum to calculate HIF-1 activity per unit of metastatic lung tumors (d). Means ± s.d. n = 10. *P < 0.05. **P < 0.01. NS = not significant.
HIF-1-mediated metabolic reprogramming reduced ROS levels and increased the survival of metastatic cancers
We next investigated whether HIF-1-mediated metabolic reprogramming led to a decrease in ROS levels during tumor metastasis to the lungs. Lungs with metastatic tumors were surgically excised 7 days after the i.v. transplantation of cancer cells, which was 1 day after the peak in HIF-1 activity and were subjected to immunohistochemical analyses for protein carbonyls and phospho-p38 as markers of ROS and oxidative stress. Although ROS levels was confirmed to be markedly decreased on day 7 (Fig. 2b,4a: DMSO), the YC-1 treatment cancelled this decrease (Fig. 4a: right). These results indicated that HIF-1-mediated metabolic reprogramming functioned to clear cytosolic ROS.
HIF-1-mediated metabolic reprogramming reduced ROS levels and increased the survival of metastatic cancers.
Athymic nude mice were i.v. transplanted with a suspension of the stable transfectant, EMT6/CMVp-CLuc/5HREp-FLuc cells (1 × 106/mouse) and treated with or without the HIF-1 inhibitor, YC-1 (30 mg/kg daily) from 3 to 6 days after the transplantation of cancer cells. (a) Lungs with the resultant metastatic tumors were surgically excised 7 days after the transplantation, which was 1 day after the peak in HIF-1 activity and ROS levels (SeeFig. 1h,2b) and ROS was detected in methacarn-fixed paraffin-embedded sections (upper) and formalin-fixed paraffin-embedded sections (lower) by the Protein Carbonyls Immunohistochemical Staining Kit and anti-phospho-p38 antibody, respectively. Bar = 500 μm (upper) and 20 μm (lower). (b) Ten days after the transplantation, mice were subjected to the in vivo CLuc assay in the serum for tumor volume. (c) Lungs with the resultant metastatic tumors were surgically excised 10 days after the transplantation, treated with Bouin's solution and the number of colonies was externally counted. Means ± s.d. n = 10. *P < 0.05. (d) Representative images of the lungs are shown.
To directly test the involvement of the HIF-1-mediated reduction of ROS levels in the survival of metastatic cancer cells in the lungs, the HIF-1 inhibitor, YC-1 was administered to the mouse model of pulmonary metastases. The in vivo CLuc assay confirmed that the YC-1 treatment from day 3 to day 6 did not suppress the progression of metastatic tumors in the lungs until 6 days after the i.v. transplantation of cancer cells, as demonstrated above (Fig. 3b). However, its HIF-1-blocking effect, which was detected on day 6 (Fig. 3c,d), eventually led to a significant reduction in both tumor volume (CLuc activity in the serum; Fig. 4b) and the number of metastatic colonies in the lungs (Fig. 4c,d) on day 10. Taken together, these results support a model in which cancer cells obtain high HIF-1 activity in response to oxidative stimuli, reduce ROS levels and survive severe microenvironments during metastatic colonization in the lungs.
Discussion
In the present study, we revealed that HIF-1, in response to elevated ROS levels, mediated the shift in oxidative phosphorylation to anaerobic glycolysis to decrease ROS levels and eventually increased the survival of cancer cells during the metastatic colonization of cancers in the lungs. Although both metabolic reprogramming and metastatic colonization are known to be under the control of HIF-1, their molecular mechanisms and functions have so far been discussed separately. Therefore, this is the first study to demonstrate the functional relationship between metabolic reprogramming and metastatic colonization.
Although we demonstrated the importance of the HIF-1-mediated clearance of ROS in the survival of cancer cells during metastatic colonization, we cannot exclude the possibility that another HIF-1-dependent mechanism may also have supported survival. For example, cancer cells may be able to produce more ATP through metabolic reprogramming and survive severe conditions during metastatic colonization. This should be examined in future studies.
In addition to previous studies reporting the involvement of HIF-1 in the first phase of distant tumor metastasis, we demonstrated the critical function of HIF-1 in the second phase. This study further justified targeting HIF-1 to inhibit distant tumor metastasis.
Methods
Cell culture
The mouse mammary carcinoma cell line (EMT6) was purchased from the American Type Culture Collection and maintained in 10% FBS-Dulbecco's modified Eagle's medium. Cells were incubated in a well-humidified incubator with 5% CO2 and 95% air at 37°C for normoxic incubation. Cells were incubated in the Bactron Anaerobic Chamber, BACLITE-2 (Sheldon Manufacturing, Cornelius, OR, USA) for <0.02% O2 hypoxic conditions or in the multi-gas CO2 incubator (Panasonic, Japan) for 3% O2 hypoxic conditions.
Plasmids
To construct pcDNA4A/CLuc, which constitutively expresses the CLuc protein, the CLuc coding sequence was prepared from pCL-sv (Atto corp. Tokyo, Japan) and inserted into a unique EcoRI site of pcDNA4/myc-his A (Invitrogen). The plasmid p5HRE-Luc, which expresses firefly luciferase under the control of the HIF-1-dependent 5HRE promoter, was constructed as described previously23.
Stable transfectants
EMT6 cells were transfected with pcDNA4A/CLuc (for EMT6/CMVp-CLuc cells) or both pcDNA4A/CLuc and p5HRE-Luc (for EMT6/CMVp-CLuc/5HREp-FLuc). Cells were then cultured for 10–14 days in culture medium containing the corresponding antibiotic to select antibiotic-resistant stable transfectants. The resultant colonies were isolated and established as clones. Representative clones showing the expected and reasonable activities were used in the present study.
Firefly Luc assay and CLuc assay in vitro
Regarding the firefly luciferase assay, a cell suspension was harvested with the Passive Lysis Buffer (Promoga) and subjected to the luciferase assay kit (Promoga) according to the manufacturer's instructions. Regarding the Cluc assay in vitro, 10 μL culture medium was harvested and directly subjected to the CLuc assay kit (Atto Corp, Tokyo, Japan) according to the manufacturer's instructions. The absolute firefly luciferase activity and CLuc activity were normalized to the number of cells counted just after harvesting.
Western blot analysis
To detect protein carbonyl in culture cells as the typical markers of oxidative stress24, cell lysates harvested in Cell Lytic Buffer (Sigma Aldrich) were treated with 2,4-dinitrophenylhydrazine and subjected to Western blotting using the anti-dinitrophenol rabbit polyclonal antibody (Cosmo Bio, Co. Ltd, Tokyo, Japan) and anti-β-actin antibody (BioVision Research Products) according to the manufacturer's instructions.
Ethics of animal experiments
All animal experiments were approved by the Animal Research Committee of Kyoto University and performed according to guidelines governing animal care in Japan.
In vivo experiments
Cancer cell suspensions (1 × 106 cells/mouse) were subcutaneously transplanted into the right hind leg of athymic nude mice for the subcutaneous tumor xenograft. The tumor volume was calculated as 0.5 × length × width2. Cancer cell suspensions (1 × 106 cells/mouse) were intravenously transplanted into athymic nude mice for a mouse model of pulmonary metastases. To monitor HIF-1 activity in pulmonary metastasis, the model mice of pulmonary metastasis were subjected to the IVIS Spectrum in vivo imaging system (Caliper) as described previously19,20,21,23,33,34. Regarding the in vivo CLuc assay, 10 μL serum was harvested from the model mice of pulmonary metastasis and subjected to the CLuc assay kit according to the manufacturer's instructions (Atto Corp). HIF-1 activity in lung metastases was divided by CLuc activity in the serum to calculate HIF-1 activity per unit of metastatic lung tumors. Tumor-bearing mice were treated with saline (-), NAC (1,000 mg/kg/administration, 2 injections/day from 1 to 6 days after the i.v. transplantation of cancer cell), or YC-1 (30 mg/kg daily from 3 to 6 days after the i.v. transplantation of cancer cells).
Immunohistochemical analyses
To simultaneously detect pimonidazole and CD31, the hypoxia marker, pimonidazole was injected i.p. (60 mg/kg body weight) 90 min before mice were sacrificed. Lungs with metastatic tumors were surgically excised and their frozen sections were stained with the FITC-conjugated anti-pimonidazole antibody (Hypoxyprobe, Inc.) for hypoxia (green), with a combination of the anti-mouse CD31 rat monoclonal antibody (BD Bioscience) and Alexa Fluor 594 goat anti-rat IgG (Invitrogen) for CD31 (red) and with Hoechst33342 for counter staining (blue), as described previously19,20,33,35,36. To detect oxidative stress as protein carbonyls, methacarn-fixed paraffin-embedded sections were stained with a combination of the Protein Carbonyls Immunohistochemical Staining Kit (Cosmo Bio Co., LTD.) and Alexa Fluor 488 goat anti-rabbit IgG (Invitrogen) to detect ROS according to the manufacturer's instructions. To detect phospho-p38 as a marker of the cellular response to oxidative stress, formalin-fixed paraffin-embedded sections were stained with the anti-mouse phospho-p38MAPK antibody (Cell Signaling Technology, Tokyo, Japan) according to the manufacturer's instructions. To simultaneously detect LDHA and p-PDH-E1α, frozen sections of lungs with metastatic tumors were stained with a combination of the anti-mouse LDHA goat polyclonal antibody (Santa Cruz Biotechnology, Inc.) and Alexa Fluor 488 donkey anti-goat IgG (Invitrogen), with a combination of the anti-phosphorylated form of the PDH-E1α (p-PDH-E1α) rabbit polyclonal antibody (Novus) and Alexa Fluor 594 goat anti-rabbit IgG (Invitrogen).
References
Chaffer, C. L. & Weinberg, R. A. A perspective on cancer cell metastasis. Science 331, 1559–1564 (2011).
De Craene, B. & Berx, G. Regulatory networks defining EMT during cancer initiation and progression. Nat Rev Cancer 13, 97–110 (2013).
Polyak, K. & Weinberg, R. A. Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer 9, 265–273 (2009).
Egeblad, M. & Werb, Z. New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer 2, 161–174 (2002).
Pantel, K., Brakenhoff, R. H. & Brandt, B. Detection, clinical relevance and specific biological properties of disseminating tumour cells. Nat Rev Cancer 8, 329–340 (2008).
Erler, J. T. et al. Hypoxia-induced lysyl oxidase is a critical mediator of bone marrow cell recruitment to form the premetastatic niche. Cancer Cell 15, 35–44 (2009).
Erler, J. T. et al. Lysyl oxidase is essential for hypoxia-induced metastasis. Nature 440, 1222–1226 (2006).
Psaila, B. & Lyden, D. The metastatic niche: adapting the foreign soil. Nat Rev Cancer 9, 285–293 (2009).
Wang, G. L., Jiang, B. H., Rue, E. A. & Semenza, G. L. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci U S A 92, 5510–5514 (1995).
Kallio, P. J., Pongratz, I., Gradin, K., McGuire, J. & Poellinger, L. Activation of hypoxia-inducible factor 1alpha: posttranscriptional regulation and conformational change by recruitment of the Arnt transcription factor. Proc Natl Acad Sci U S A 94, 5667–5672 (1997).
Jaakkola, P. et al. Targeting of HIF-alpha to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science 292, 468–472 (2001).
Forsythe, J. A. et al. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol Cell Biol 16, 4604–4613 (1996).
Norris, M. L. & Millhorn, D. E. Hypoxia-induced protein binding to O2-responsive sequences on the tyrosine hydroxylase gene. J Biol Chem 270, 23774–23779 (1995).
Semenza, G. L. Targeting HIF-1 for cancer therapy. Nat Rev Cancer 3, 721–732 (2003).
Semenza, G. L. Defining the role of hypoxia-inducible factor 1 in cancer biology and therapeutics. Oncogene 29, 625–634 (2010).
Semenza, G. L. Hypoxia-inducible factors: mediators of cancer progression and targets for cancer therapy. Trends Pharmacol Sci 33, 207–214 (2012).
Semenza, G. L. Regulation of cancer cell metabolism by hypoxia-inducible factor 1. Semin Cancer Biol 19, 12–16 (2009).
Harada, H. & Hiraoka, M. Hypoxia-inducible factor 1 in tumor radioresistance. Curr Signal Transd Ther 5, 188–196 (2010).
Harada, H. et al. Cancer cells that survive radiation therapy acquire HIF-1 activity and translocate towards tumour blood vessels. Nat Commun 3, 783 (2012).
Harada, H. et al. Treatment regimen determines whether an HIF-1 inhibitor enhances or inhibits the effect of radiation therapy. Br J Cancer 100, 747–757 (2009).
Harada, H. et al. Significance of HIF-1-active cells in angiogenesis and radioresistance. Oncogene 26, 7508–7516 (2007).
Yeom, C. J., Goto, Y., Zhu, Y., Hiraoka, M. & Harada, H. Microenvironments and cellular characteristics in the micro tumor cords of malignant solid tumors. Int J Mol Sci 13, 13949–13965 (2012).
Harada, H., Kizaka-Kondoh, S. & Hiraoka, M. Optical imaging of tumor hypoxia and evaluation of efficacy of a hypoxia-targeting drug in living animals. Mol Imaging 4, 182–193 (2005).
Sato, T. et al. Senescence marker protein-30 protects mice lungs from oxidative stress, aging and smoking. Am J Respir Crit Care Med 174, 530–537 (2006).
Nakamura, A. & Goto, S. Analysis of protein carbonyls with 2,4-dinitrophenyl hydrazine and its antibodies by immunoblot in two-dimensional gel electrophoresis. J Biochem 119, 768–774 (1996).
Robinson, C. E. et al. Determination of protein carbonyl groups by immunoblotting. Anal Biochem 266, 48–57 (1999).
Ishimoto, T. et al. CD44 variant regulates redox status in cancer cells by stabilizing the xCT subunit of system xc(-) and thereby promotes tumor growth. Cancer Cell 19, 387–400 (2011).
Muller, M. Cellular senescence: molecular mechanisms, in vivo significance and redox considerations. Antioxid Redox Signal 11, 59–98 (2009).
Murphy, M. P. et al. Unraveling the biological roles of reactive oxygen species. Cell Metab 13, 361–366 (2011).
Li, C. & Jackson, R. M. Reactive species mechanisms of cellular hypoxia-reoxygenation injury. Am J Physiol Cell Physiol 282, C227–241 (2002).
Wang, W. et al. Superoxide flashes in single mitochondria. Cell 134, 279–290 (2008).
Zhou, T. B., Qin, Y. H., Lei, F. Y., Huang, W. F. & Drummen, G. P. Prohibitin is associated with antioxidative protection in hypoxia/reoxygenation-induced renal tubular epithelial cell injury. Sci Rep 3, 3123 (2013).
Harada, H. et al. The Akt/mTOR pathway assures the synthesis of HIF-1alpha protein in a glucose- and reoxygenation-dependent manner in irradiated tumors. J Biol Chem 284, 5332–5342 (2009).
Harada, H. et al. The combination of hypoxia-response enhancers and an oxygen-dependent proteolytic motif enables real-time imaging of absolute HIF-1 activity in tumor xenografts. Biochem Biophys Res Commun 360, 791–796 (2007).
Zeng, L. et al. TS-1 enhances the effect of radiotherapy by suppressing radiation-induced hypoxia-inducible factor-1 activation and inducing endothelial cell apoptosis. Cancer Sci 99, 2327–2335 (2008).
Zhu, Y. et al. Involvement of decreased hypoxia-inducible factor 1 activity and resultant G1-S cell cycle transition in radioresistance of perinecrotic tumor cells. Oncogene 32, 2058–2068 (2013).
Acknowledgements
This study was supported by the Funding Program for NEXT Generation World-Leading Researchers (NEXT Program) from the Japan Society for the Promotion of Science (JSPS), Japan to H.H. (No. LS071), by the Program for Promotion of Fundamental Studies in Health Science from the National Institute of Biomedical Innovation (NIBIO), Japan to H.H. (No. 09-25), by Grants-in-Aid for Young Scientists (B) from the Ministry of Education, Culture, Sports, Science and Technology (MEXT), Japan to M.K. (No. 25861088), M.Y. (No. 24791293) and S.I. (No. 24659563), by the Sagawa Foundation for the Promotion of Cancer Research to H.H., by the Kobayashi Foundation for Cancer Research to H.H., by the Takeda Science Foundation to H.H. and by the Mochida Memorial Foundation for Medical and Pharmaceutical Research to H.H.
Author information
Authors and Affiliations
Contributions
H.H. designed and supervised the study and wrote the manuscript. T.Z., Y.Z., A.M., M.K. and K.S. performed experiments and analyzed the data. S.I., M.Y., G.G. and M.H. contributed to the data analysis and discussion.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary Figure S1-S4
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Zhao, T., Zhu, Y., Morinibu, A. et al. HIF-1-mediated metabolic reprogramming reduces ROS levels and facilitates the metastatic colonization of cancers in lungs. Sci Rep 4, 3793 (2014). https://doi.org/10.1038/srep03793
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep03793
This article is cited by
-
Survival mechanisms of circulating tumor cells and their implications for cancer treatment
Cancer and Metastasis Reviews (2024)
-
Perfluorodecalin-based oxygenated emulsion as a topical treatment for chemical burn to the eye
Nature Communications (2022)
-
Effect of hypoxia factors gene silencing on ROS production and metabolic status of A375 malignant melanoma cells
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.