Abstract
We assessed whether increasing body mass index (BMI) affects health-related quality of life in a group of 38 overweight (BMI 25–30 kg/m2) middle-aged (45.9 ± 5.4 years) men, recruited in Auckland (New Zealand). Health-related quality of life was assessed with SF-36v2 at 0, 12 and 30 weeks. Increasing BMI was associated with a progressive reduction in physical component summary score (p = 0.008), as well as lower general health (p = 0.036), physical functioning (p = 0.024) and bodily pain (p = 0.030) scores. Stratified analyses confirmed these findings: participants who were more overweight (n = 19; BMI 27.5–30 kg/m2) had poorer physical component summary (p = 0.005), physical functioning (p = 0.040), bodily pain (p = 0.044) and general health (p = 0.073) scores than the less overweight (n = 19; BMI 25–27.5 kg/m2). Increasing BMI is associated with a progressive reduction in physical quality of life, even within a relatively narrow BMI range encompassing only overweight middle-aged men.
Similar content being viewed by others
Introduction
There is a global obesity pandemic and obesity rates in New Zealand continue to increase in both adults and children1. In 2011–2012, 28% of New Zealand's adult population were obese, compared to 19% in 19971. Importantly, a further 35% of the adult population were overweight but not obese1. While obesity rates are identical in both sexes, men are more likely to be overweight than women (41.3 vs 32.8%)2.
There is ever increasing awareness of the adverse effects of obesity on morbidity and mortality, particularly via cardiovascular diseases. There is also increasing evidence that obesity affects health-related quality of life (HRQL), especially physical functioning3. Numerous studies have examined the effects of body mass index (BMI) on HRQL, showing that higher degrees of obesity are associated with increased burden of disease3,4,5,6,7,8. These studies demonstrated that the more obese a person is, the poorer the physical health, reflected for example in impaired ability to perform daily physical tasks.
However, the data on overweight (BMI 25–30 kg/m2) as compared to obesity (≥30 kg/m2) have yielded inconsistent findings and some studies have not observed adverse effects on HRQL4,6,7,8. In light of the conflicting data in this particular group, we assessed whether increasing BMI affects health-related quality of life in a group of overweight middle-aged men.
Results
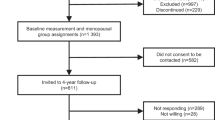
Study cohort
45 participants took part in the clinical trial9, but 7 were excluded due to incomplete HQRL data. Thus, 38 overweight men (BMI 27.3 ± 1.4 kg/m2), aged 45.9 ± 5.4 years (range 34.5–55.6) were studied. Most were of New Zealand European ethnicity (89%). Three participants were on antihypertensive medication, three were on lipid-lowering medications and two participants were on both. No participants had any other active physical or mental health co-morbidities. Note that the trial interventions had no effect on any HRQL scores.
Compared to New Zealand normative data, study participants displayed similar scores in the mental health domains, namely vitality (p = 0.36), social functioning (p = 0.29), role emotional (p = 0.31) and mental health (p = 0.10). However, study participants displayed better physical well-being than the normative data, with higher role physical (95.5 vs 85.7; p < 0.001), physical functioning (94.5 vs 85.9; p < 0.001), bodily pain (82.5 vs 75.3; p = 0.012) and general health (80.2 vs 74.5; p = 0.009) scores.
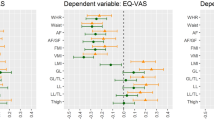
BMI vs HRQL
Univariate analyses showed that BMI was negatively correlated with physical component summary (r = −0.43; p = 0.007), physical functioning (ρ = −0.34; p = 0.035) and bodily pain (ρ = −0.34; p = 0.037) scores, also tending towards a similar association with general health (r = −0.30; p = 0.065) and vitality (r = −0.29; p = 0.081) scores. These results were corroborated by multivariate models, which showed that greater BMI was associated with poorer physical quality of life. Thus, increasing BMI was associated with a progressive reduction in physical component summary score (p = 0.008), as well as lower general health (p = 0.036), physical functioning (p = 0.024) and bodily pain (p = 0.030) scores.
The stratified analyses confirmed the findings that increasing BMI among overweight men was associated with a progressive reduction in physical quality of life. Participants who were more overweight (n = 19; BMI 27.5–30 kg/m2) had poorer physical quality of life than those were less overweight (n = 19; BMI 25–27.5 kg/m2) (Table 1). This was illustrated by differences in the physical component summary score (p = 0.005), as well as physical functioning (p = 0.040), bodily pain (p = 0.044) and general health (p = 0.073) scores (Table 1). There were no differences between groups in mental health domains.
Discussion
This study shows that increasing BMI is associated with a progressive reduction in physical quality of life among middle-aged men. Importantly, this was observed to occur within a relatively narrow BMI range, encompassing only overweight men. Further, our findings were observed in an otherwise healthy group of individuals, with the possible confounding effects of physical activity levels and significant comorbidities accounted for.
The increased morbidity and mortality associated with obesity is widely recognized. However, recent studies have suggested that this is not the case for those who are overweight when compared to normal-weight individuals13,14,15,16. Similarly, the HRQL literature on the effects of overweight is conflicting and some studies found no effects of overweight on HRQL in comparison to those of normal weight6,7,8. However, irrespective of whether HRQL in a group of overweight males actually differs to that of normal-weight controls, our data do show that increasing BMI is associated with poorer outcomes in physical domains, even within a group consisting solely of overweight individuals.
We did not observe any effects of BMI on mental health domains assessed. These findings are consistent with a number of previous studies showing that physical quality of life is far more affected by increasing BMI than mental health domains6,17,18. However, the observed reduction in physical functioning in our overweight cohort may lead to decreased energy expenditure, resulting in increasing mismatch in energy balance and additional weight gain19. Thus, the observed impairments in physical health in overweight individuals may eventually lead to the onset of obesity. As a result, while we did not observe any effects of increasing BMI on mental health domains, progression to obesity would likely result in adverse effects on mental health20.
The main limitation of our study was our relatively small number of participants (n = 38). However, our findings are particularly robust as each participant underwent three assessments over a 30-week period. Thus, our study design minimized the potential effects of temporal variations in HRQL that might have been experienced by individual participants. Nonetheless, we studied a relatively narrow range of individuals (overweight males living in a large urban centre, mostly of New Zealand European ethnicity), which may limit wider applicability of our findings.
In summary, we found that physical quality of life is affected by increasing overweight levels, in the absence of overt obesity. There is considerable focus on public health interventions targeting those who are obese. Our study shows that overweight non-obese individuals also display impairments in physical quality of life. It is important therefore that such aspects are considered in the health management of overweight individuals, not only to improve quality of life, but also to prevent further reductions in physical activity levels and halt a consequent progression to obesity.
Methods
This study encompassed the post hoc analysis of data from a 30-week randomized, double-blinded, placebo-controlled, crossover trial examining the effects of olive leaf extract on insulin sensitivity9. All participants were overweight men (BMI 25–30 kg/m2) aged 35–55 years, who were recruited in February 2011 via advertisements in local newspapers that circulate freely in the central Auckland metropolitan area (New Zealand). Note that only males were recruited to the clinical trial so that the effects of the menstrual cycle on insulin sensitivity could be avoided. Exclusion criteria were: drug use (including tobacco), diabetes, or being on medications likely to affect insulin sensitivity. Subjects taking antihypertensive or lipid-lowering medications were recruited, but were required to have been on a stable dose for at least 6 months prior to start of the study. These subjects were also encouraged not to change dose throughout the trial and doses were checked at each assessment. All participants were asked not to make any substantial alterations to their lifestyle for the duration of the trial. Specifically, participants were instructed not to make changes to their diet and physical activity levels.
Participants were assessed at baseline and after 12 and 30 weeks. Clinical assessments were carried out at the Maurice & Agnes Paykel Clinical Research Unit (Liggins Institute, University of Auckland). HRQL was assessed using the SF-36v2 Health Survey (New Zealand/Australia adaptation), based on subjective measures of well-being. The SF-36v2 is a validated tool that measures perception of health on eight multi-item dimensions covering functional status, wellbeing and overall evaluation of health10. The SF-36v2 assesses 8 domains, including 4 physical (general health, physical functioning, bodily pain and role limitations related to physical problems) and 4 mental (mental health, vitality, social functioning and role limitations related to emotional problems)10. Parameters summarizing both physical and mental domains were also obtained. There are a number of items that make up each individual domain. These have been presented and discussed by Ward10 and are summarized in Figure 1.
Itemized description of health-related quality of life (HRQL) measures as per the SF-36 survey.
* indicates significant correlation with other summary measure. Reproduced with permission from Ware JE, Jr. SF-36® Health Survey Update; http://www.sf-36.org/tools/sf36.shtml.
Auxological assessment included height measurement using a Harpenden stadiometer. Weight was measured using whole-body dual-energy X-ray absorptiometry (DXA, Lunar Prodigy 2000, General Electric, Madison, USA). Physical activity levels were assessed using the International Physical Activity Questionnaire (IPAQ)11, covering four domains of physical activity: work-related, transportation, housework/gardening and leisure time.
Univariate analyses were initially performed using simple correlations or Spearman's rank correlations. SF-36v2 data for the study cohort were compared to normative data for New Zealand men aged 45–64 years12 using two-sample t-tests. Random effect mixed models with repeated measures were used to evaluate the association of BMI with SF-36v2 outcomes. Randomization sequences, time period and on-going use of medication (for cholesterol or hypertension) were accounted for, with IPAQ score also included as a co-variate. Stratified analyses were also carried out dividing the study cohort in half, separating participants according to BMI. Univariate analyses were carried out in Minitab v.16 (Pennsylvania State University, State College, PA, USA), while multivariate analyses were performed in SAS v.9.3 (SAS Institute Inc. Cary, NC, USA). Demographic data are presented as means ± standard deviation, while outcome data are presented as model-adjusted means (estimated marginal means adjusted for the confounding factors in the models), with associated 95% confidence intervals. All statistical tests were two-sided and a 5% significance level maintained throughout the analyses.
Ethics approval for this study was provided by the Northern Y Regional Ethics Committee (New Zealand Ministry of Health) and written informed consent was obtained from all participants. This study was registered with the Australian New Zealand Clinical Trials Registry (#336317).
References
Ministry of Health. . Annual Report for the year ended 30 June 2013 including the Director-General of Health's Annual Report on the State of Public Health. (Ministry of Health, Wellington, 2013).
University of Otago & Ministry of Health. A Focus on Nutrition: Key findings of the 2008/09 New Zealand Adult Nutrition Survey. (Ministry of Health, Wellington, 2011).
Fontaine, K. R. & Barofsky, I. Obesity and health-related quality of life. Obes. Rev. 2, 173–182 (2001).
Ul-Haq, Z., Mackay, D. F., Fenwick, E. & Pell, J. P. Meta-analysis of the association between body mass index and health-related quality of life among adults, assessed by the SF-36. Obesity (Silver Spring, Md.) 21, E322–327 (2013).
Ul-Haq, Z., Mackay, D. F., Fenwick, E. & Pell, J. P. Impact of metabolic comorbidity on the association between body mass index and health-related quality of life: a Scotland-wide cross-sectional study of 5,608 participants. BMC Public Health 12, 143 (2012).
Hopman, W. M. et al. The association between body mass index and health-related quality of life: data from CaMos, a stratified population study. Qual. Life Res. 16, 1595–1603 (2007).
Vasiljevic, N. et al. The assessment of health-related quality of life in relation to the body mass index value in the urban population of Belgrade. Health Qual. Life Outcomes 6, 106 (2008).
Lopez-Garcia, E. et al. Relation between body weight and health-related quality of life among the elderly in Spain. Int. J. Obes. Relat. Metab. Disord. 27, 701–709 (2003).
de Bock, M. et al. Olive (Olea europaea L.) leaf polyphenols improve insulin sensitivity in middle-aged overweight men: a randomized, placebo-controlled, crossover trial. PLoS ONE 8, e57622 (2013).
Ware, J. E., Jr SF-36 health survey update. Spine 25, 3130–3139 (2000).
Hagstromer, M., Oja, P. & Sjostrom, M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 9, 755–762 (2006).
Scott, K. M., Tobias, M. I., Sarfati, D. & Haslett, S. J. SF-36 health survey reliability, validity and norms for New Zealand. Aust. N. Z. J. Public Health 23, 401–406 (1999).
Lenz, M., Richter, T. & Muhlhauser, I. The morbidity and mortality associated with overweight and obesity in adulthood: a systematic review. Dtsch. Arztebl. Int. 106, 641–648 (2009).
Janssen, I. Morbidity and mortality risk associated with an overweight BMI in older men and women. Obesity (Silver Spring, Md.) 15, 1827–1840 (2007).
McGee, D. L. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann. Epidemiol. 15, 87–97 (2005).
Janssen, I. & Mark, A. E. Elevated body mass index and mortality risk in the elderly. Obes. Rev. 8, 41–59 (2007).
Huang, I. C., Frangakis, C. & Wu, A. W. The relationship of excess body weight and health-related quality of life: evidence from a population study in Taiwan. Int. J. Obes. 30, 1250–1259 (2006).
Doll, H. A., Petersen, S. E. & Stewart-Brown, S. L. Obesity and physical and emotional well-being: associations between body mass index, chronic illness and the physical and mental components of the SF-36 questionnaire. Obes. Res. 8, 160–170 (2000).
Schwimmer, J. B., Burwinkle, T. M. & Varni, J. W. Health-related quality of life of severely obese children and adolescents. JAMA 289, 1813–1819 (2003).
Kolotkin, R. L., Meter, K. & Williams, G. R. Quality of life and obesity. Obes. Rev. 2, 219–229 (2001).
Acknowledgements
This study was supported by a TECHNZ grant (University of Auckland - UniS 30475.001) through the New Zealand Ministry of Science and Innovation. MdB was funded by the Joan Mary Reynolds Trust. We also thank the Paykel Trust for long-term funding of the Maurice & Agnes Paykel Clinical Research Unit at the Liggins Institute (University of Auckland) and Dr Yannan Jiang (Department of Statistics, University of Auckland) for valuable statistical input.
Author information
Authors and Affiliations
Contributions
M.d.B., W.S.C., P.L.H. and J.G.B.D. conceived and designed the experiment. M.d.B. performed the experiment. J.G.B.D. analysed the data. J.G.B.D. and M.d.B. wrote the manuscript with input from W.S.C. and P.L.H.
Ethics declarations
Competing interests
The authors have no financial or non-financial conflicts of interest to disclose that may be relevant to this work. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Rights and permissions
This work is licensed under a Creative Commons Attribution 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by/3.0/
About this article
Cite this article
Derraik, J., de Bock, M., Hofman, P. et al. Increasing BMI is associated with a progressive reduction in physical quality of life among overweight middle-aged men. Sci Rep 4, 3677 (2014). https://doi.org/10.1038/srep03677
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep03677
This article is cited by
-
Longitudinal Study of Body Composition and Energy Expenditure in Overweight or Obese Young Adults
Scientific Reports (2020)
-
Effect of high body mass index on knee muscle strength and function after anterior cruciate ligament reconstruction using hamstring tendon autografts
BMC Musculoskeletal Disorders (2018)
-
Abdominal obesity is strongly associated with Cardiovascular Disease and its Risk Factors in Elderly and very Elderly Community-dwelling Chinese
Scientific Reports (2016)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.