Abstract
Metastasis-associated protein 1 (MTA1), a negative epigenetic modifier, plays a critical role in prostate cancer (PCa) progression. We hypothesized that MTA1 overexpression in primary tumor tissues can predict PCa aggressiveness and metastasis. Immunohistochemical staining of MTA1 was done on archival PCa specimens from University of Mississippi Medical Center and University of Iowa. We found that nuclear MTA1 overexpression was positively correlated with the severity of disease progression reaching its highest levels in metastatic PCa. Nuclear MTA1 overexpression was significantly associated with Gleason > 7 tumors in African Americans but not in Caucasians. It was also a predictor of recurrent disease. We concluded that MTA1 nuclear overexpression may be a prognostic indicator and a future therapeutic target for aggressive PCa in African American men. Our findings may be useful for categorizing African American patients with a higher probability of recurrent disease and metastasis from those who are likely to remain metastasis-free.
Similar content being viewed by others
Introduction
Prostate cancer (PCa) is a major public health problem in the United States. Major advances in the detection and diagnosis of localized PCa have resulted in significant improvement of the management of PCa by surgery and radiation. However, an important clinical question remains of how to distinguish aggressive PCa from indolent disease. Identifying the subset of patients with aggressive disease at the time of surgery (radical prostatectomy, RP) may allow for the use of more tailored therapeutic strategies. The probability of recurrent disease has been predicted on the basis of preoperative serum prostate-specific antigen (PSA) levels, sex steroids levels and other clinicopathological parameters such as tumor stage, biopsy Gleason score and surgical margins1,2,3,4,5,6,7,8,9,10. Integration of gene expression profiling and clinical variables has increased prediction accuracy for recurrent and aggressive disease11,12. However, the existing pathological and molecular prognostic indicators still do not accurately predict future recurrence and outcome, partially due to heterogeneity of the disease and racial disparity. As a result, despite the known clinical heterogeneity of PCa and racial differences in disease progression, all patients are screened similarly for prognosis and all patients with signs of biochemical recurrence are treated similarly. Improved, new and “tailored” prognostic biomarkers are needed to determine which patients are at a higher risk of developing recurrent disease and metastasis from those who are likely stay metastasis-free. Identifying these patients at the time of RP will allow for more appropriate clinical management of aggressive disease and avoid unnecessary over-treatment for patients who are cured with surgery.
In the United States, African Americans have 1.6 times the incidence of and 2.4 times the mortality from PCa compared to Caucasian Americans13. We and others have shown that African Americans have an earlier onset of PCa and worse outcomes than Caucasians14,15,16. Socioeconomic and environmental factors, such as diet, access to care and screening, have been cited as factors contributing to the disparity in PCa risk, incidence and more clinically aggressive PCa in African Americans compared to Caucasians. On the other hand, a recent study demonstrated that high socioeconomic status was correlated with reduced PCa risk, partially due to more screening frequency17. More recently, evidence is emerging that the disparity in PCa risk and advanced stage of disease may be explained by various biological factors such as higher levels of estrogen in African American men18, different NDRG1 (N-myc downstream-regulated gene 1) expression patterns19 or different levels of leptin in utero20.
In our previous studies we were the first to identify metastasis-associated protein 1 (MTA1) as a part of the PCa bone metastatic signature21 and further demonstrate that inhibition of MTA1 by RNAi technology or pharmacological agents decreases metastatic potential of PCa cells in vitro and in vivo21,22,23. Although the molecular mechanisms of MTA1 activity are poorly understood, it is evident that MTA1, as a part of the nucleosome remodeling and deacetylation (NuRD) co-repressor complex, plays a negative role in posttranslational modifications of certain tumor suppressors such as p5322. Overexpression of MTA1 in several types of human cancers correlates with clinicopathological parameters that characterize tumor progression and aggressiveness. Studies have demonstrated that MTA1 mRNA levels were significantly higher and associated with frequent lymph node metastasis, increased tumor grade and angiogenesis in patients with various carcinomas24,25,26,27. Relevant to our current study, MTA1 protein expression was higher in hormone-refractory metastatic PCa compared with clinically localized disease28. We, on the other hand, initially identified MTA1 as a part of the PCa bone metastatic signature using gene expression microarrays and subsequently verified overexpression of MTA1 in high grade tumors and bone metastases using tissue microarrays (TMAs) from commercial sources with limited clinicopathological information21. On the basis of our accumulated findings on the significant role of MTA1 in PCa, we hypothesized that nuclear MTA1 overexpression may provide meaningful information regarding prognosis, i.e. MTA1 may serve as a prognostic biomarker for aggressive PCa and a predictor of recurrent disease.
The objective of this study, therefore, was to assess the relationship between nuclear MTA1 overexpression and subsequent risk of recurrent disease and metastatic PCa and identify if molecular differences contribute to the racial disparity in PCa. Particularly, we asked the questions if MTA1 1) may differ in African Americans and Caucasian Americans; 2) be a factor contributing to the more clinically aggressive PCa in African American patients and 3) serve as a prognostic marker and potential therapeutic target for PCa. MTA1 expression and subcellular localization was analyzed by immunohistochemistry (IHC) on customized PCa TMAs and whole slides and correlated with clinicopathological parameters and disease recurrence.
Results
Nuclear MTA1 overexpression in human PCa tumors is correlated with aggressive disease and metastasis
To investigate the clinical significance of MTA1 expression in human PCa progression and metastasis, we analyzed protein expression by IHC in a total of 291 patients, including 143 African Americans and 148 Caucasian Americans with the median age of 61.3 years at the time of surgery. We examined 34 benign, 22 prostate intraepithelial neoplasia (PIN), 205 clinically localized PCa and 30 metastatic cases, from which 23 (76.7%) had bone metastasis. We stratified localized PCa (LPCa) by the Gleason score into three subgroups, Gleason score < 7, = 7 and > 7. Demographic and clinicopathological characteristics of the patients are summarized in Table 1.
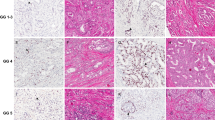
We evaluated MTA1 expression with the emphasis on subcellular localization and total staining score, which accounted for both intensity and frequency (see Materials and Methods). MTA1 was detected in both the cytoplasm and nucleus; however, it exhibited different expression patterns in terms of localization depending on pathological category of PCa and metastasis. In the benign and PIN samples, MTA1 protein expression appeared to be largely weak and cytoplasmic. In addition to cytoplasmic staining, localized PCa tissues, demonstrated increased nuclear staining associated with higher Gleason score, which reached its predominance in Gleason > 7 cases. In addition, all types of metastatic lesions [lymph node (LN), central nervous system (CNS) and bone] revealed predominant and intensive MTA1 nuclear staining (Fig. 1A). Interestingly, while cytoplasmic staining was comparable in each category, in metastatic tissues it was significantly reduced (p = 0.0001). Altogether, the nuclear to cytoplasmic (N/C) ratio of MTA1 expression increased from PIN to localized and to metastatic PCa (MPCa) (Table S1 online, Fig. 1B). In the localized PCa cases, there was a tendency towards increased N/C ratio in higher Gleason score tissues; however, the differences were not statistically significant (Table S1 online).
(A): Nuclear MTA1 overexpression is associated with PCa progression from PIN to localized PCa to metastasis. Representative images of MTA1 expression and subcellular distribution in PCa tissues and metastatic lesions analyzed by IHC and accompanied by H&E staining are shown. Benign tissues and PIN showed weak or moderate staining mostly in the cytoplasm; meanwhile, nuclear staining was stronger with a greater Gleason score: mostly cytoplasmic in Gleason < 7 tumors, moderate cytoplasmic and nuclear in Gleason = 7 tumors; and predominantly nuclear staining in Gleason > 7 cases. Metastatic tissues showed strong, almost exclusively, nuclear staining. (B): Distribution of nuclear (N) to cytoplasmic (C) ratio (N/C ratio) of MTA1 staining (TS) in different PCa pathologic categories. Geometric mean for N/C ratio for each category was calculated. Differences in N/C ratio were statistically significant between localized PCa and PIN. N/C ratio in metastatic PCa was the highest since cytoplasmic staining was statistically decreased compared to other categories. N/C ratio in Gleason subgroups showed a tendency to increase with Gleason score but differences were not statistically significant (not shown).
Racial differences in nuclear MTA1 overexpression between African Americans and Caucasian Americans
We hypothesized that MTA1 expression might reveal a biological (molecular) basis for the disparity of clinical progression and outcome among PCa patients of different races.
The state of Mississippi is one of the regions in the US with a substantial African American population. Importantly, incidence and mortality rates from PCa in Mississippi rank among the nation's highest. Subsequently, our institution, in addition to cases of Caucasian Americans, collected a uniquely large amount of African Americans cases (n = 147). Moreover, African Americans, who show more aggressive cases of the disease, accounted for 20 of the total 30 metastatic samples – 14 of which were bone metastasis. The median age at the time of surgery was 57.9 years (range 49–76 years) in African Americans and 62 years (range 42–87) in Caucasians.
In patients diagnosed with PIN and metastatic PCa, there were no significant differences in nuclear MTA1 expression levels between the two races (Table 2). Remarkably, the difference in nuclear MTA1 overexpression between patients with localized PCa was highly significant (p < 0.001), with Caucasian Americans having higher levels of MTA1. When stratified by Gleason scores, in patients with Gleason > 7 (high grade tumors), there was no significant difference between the two races. However, the nuclear MTA1 levels in Gleason < 7 (p = 0.02) and especially Gleason = 7 (p < 0.0001) were significantly higher in Caucasians compared with African Americans. As seen in the Fig. 2A, ANOVA analysis of MTA1 nuclear expression in whole cohort (WC) among three groups of prostate malignancy revealed statistically significant increase from PIN to LPCa and from clinically LPCa to MPCa (p < 0.0001). Differences among Gleason subgroups were not statistically significant. Panels B and C show the dynamics of changes in MTA1 nuclear expression analyzed by race. In African Americans the MTA1 increase was statistically significant from LPCa to MPCa while in Caucasians it was not, due to higher levels of MTA1 expression in localized disease. Most importantly, there was a dramatic and statistically significant increase in nuclear MTA1 staining in Gleason > 7 patient's tumors compared to Gleason ≤ 7 (p = 0.0002 vs Gleason = 7 and p = 0.006 vs Gleason < 7) in African Americans (Fig. 2B, right panel) while Caucasian Americans had higher and comparable levels of MTA1 expression in all three Gleason-subgroups. In the Caucasian American patients with high basic levels of nuclear MTA1 expression, neither the differences between Gleason score subcategories nor the differences between different pathologic categories were statistically significant, with the exception of differences between metastatic PCa and PIN (p = 0.014) (Fig. 2C).
Racial differences in nuclear MTA1 expression between African Americans and Caucasian Americans.
(A): Comparison of MTA1 nuclear staining in PIN, localized PCa and metastasis (left) and in Gleason subgroups (right) in whole cohort (WC). MTA1 nuclear overexpression is significantly higher in metastatic (MPCa) versus localized PCa (LPCa) and PIN. No statistically significant differences were found amongst Gleason subgroups. (B): Nuclear MTA1 overexpression in African American (AA) men is associated with disease progression and higher Gleason score. Differences in MTA1 nuclear expression were statistically significant between different pathologic categories (left) and between Gleason > 7 and Gleason < 7/Gleason = 7 (right). (C): Comparison of MTA1 nuclear staining in different pathologic categories (left) and in Gleason subgroups (right) in Caucasian Americans (CA). No statistically significant changes were found between MPCa and LPCa groups and between Gleason subgroups. Box plots represent each category/score, error bars show SEM and horizontal lines represent median. TNS, total nuclear score.
Next, we analyzed for Gleason score and preoperative PSA simultaneously. We first stratified localized PCa by two subgroups on the basis of Gleason score, which were defined as group A (Gleason ≤ 7) and group B (Gleason > 7). We further stratified each group by three subcategories on the basis of pre-operative PSA levels: < 10 ng/ml as low risk; 10–20 ng/ml as intermediate risk and > 20 ng/ml as high risk. The analysis revealed that in the low risk subcategory (PSA < 10 ng/ml) higher MTA1 nuclear staining was associated with Gleason > 7 group, whereas lower MTA1 scores were associated with Gleason ≤ 7 group. Although the limited number of samples did not show a statistically significant difference between groups A and B, differences in the whole cohort were 3-fold (0.14 ± 0.1 vs 0.42 ± 0.22, p = 0.21) reaching 8.4-fold in African Americans (0.07 ± 0.03 vs 0.59 ± 0.34, p = 0.20) whereas there were no changes in Caucasian Americans (0.22 ± 0.20 vs 0.15 ± 0.13, p = 0.82). No association between MTA1 expression and intermediate and high PSA levels was found in African Americans whereas there was a trend towards association between high PSA levels and increased nuclear MTA1 expression in group A of Caucasians Americans (data not shown).
Nuclear MTA1 overexpression is correlated with disease recurrence
The next question we asked was whether nuclear MTA1 overexpression may predict PCa recurrence. Recurrent PCa was defined by a serum PSA level greater than 0.4 ng/ml after RP and/or receipt of salvage therapy after RP and/or clinical or radiological evidence of metastatic disease. Non-recurrent PCa was defined as no biochemical (< 0.4 mg/ml) or clinical evidence of recurrence. We analyzed changes in MTA1 nuclear expression in non-recurrent and recurrent groups and the association between MTA1 nuclear overexpression and clinicopathological parameters in a subset of the patients from the whole cohort with known recurrent history (Table 3). We found that MTA1 expression levels were significantly (p = 0.03) higher in the recurrent cohort compared to the non-recurrent cohort. When stratified by Gleason score, there was a tendency for higher MTA1 staining in the recurrent compared to non-recurrent group, but the differences did not reach statistical significance. Further, analysis of changes in MTA1 expression in the non-recurrent and recurrent groups by racial differences revealed a more vivid increase in the group of African American patients with recurrent disease (0.59 ± 0.18 vs 0.28 ± 0.09, 2.1-fold increase) compared to Caucasian Americans (0.8 ± 0.13 vs 0.54 ± 0.08, 1.5-fold increase) (Fig. 3). However, nuclear MTA1 expression in the recurrent group of African Americans with Gleason > 7 was marginally more significant (p = 0.09) compared to the same subgroup in the non-recurrent cohort (see Supplementary Table S2, online). In Caucasians, the differences in Gleason = 7 subgroups between non-recurrent and recurrent groups reached statistical significance (p = 0.04) (see Supplementary Table S3, online). We also examined a correlation between MTA1 nuclear expression and other parameters in the study cohort in racial groups. No significant correlation between MTA1 nuclear expression and positive surgical margin status, capsule invasion, initial or follow-up PSA levels or age was found (Table 3, Tables S2 and S3).
Expression and subcellular distribution of MTA1 in PCa cell lines
Using cell fractionation, followed by detection with Western blot, a panel of cell lines representing different stages of PCa progression was investigated for MTA1 expression and subcellular distribution. MTA1 only appeared in the nuclear fraction and at different levels reflecting “aggressiveness” of cell lines: almost undetectable levels in “normal” prostate epithelial RWPE-1 cells, higher levels in LNCaP androgen-responsive cells, more expression in Du145 androgen-resistant cells and the highest levels in extremely metastatic PC3M cells (Fig. 4A). As expected, in MDA PCa 2b cells, derived from bone metastatic site of African American man, MTA1 nuclear expression was comparable with levels in highly aggressive PC3M cells (Fig. 4B). Thus, established PCa cell lines in vitro closely represent the distribution of MTA1 in different pathologic categories in vivo.
(A): Subcellular localization and differential expression of MTA1 in cells representing different stages of PCa progression: RWPE1, “normal” immortalized prostate epithelial cells; LNCaP, androgen-responsive cells; Du145, androgen-resistant cells; PC3M, aggressive metastatic cells. (B): MTA1 nuclear expression in MDA PCa 2b cells derived from bone metastatic site of AA man is comparable with high levels of MTA1 in PC3M aggressive cell line. Nuclear and cytoplasmic fractions were obtained for western blot analysis. Erk and lamin A were used as loading controls for cytoplasmic and nuclear fractions, respectively. Full-length blots can be found in the Supplementary Information.
Discussion
The goal of this study was to investigate MTA1 expression and subcellular localization in a wide series of PCa samples and metastatic lesions to determine its role as a prognostic biomarker for recurrent/aggressive disease and metastasis and its value as a potential therapeutic target. We evaluated MTA1 expression and localization in a well-characterized cohort of African American and Caucasian American PCa patients. In general, the main observation in the whole cohort was a strong trend of increasing nuclear MTA1 expression associated with worse pathologic parameters: localized PCa and metastatic lesions had significantly higher nuclear MTA1 levels compared with PIN. Importantly, we found different patterns of MTA1 expression in African Americans compared with Caucasians between the Gleason score subgroups. Our data revealed a “jump- increase” in MTA1 nuclear expression in Gleason > 7 localized PCa compared with Gleason score 7 and below in African Americans, whereas Caucasian American patients presented similar scores to each other but a higher baseline MTA1 expression pattern in all localized tumors. The reason for these elevated levels of MTA1 in Caucasians is not clear. The obtained data suggest that nuclear MTA1 overexpression was able to differentiate more aggressive tumors in the African American cohort but not in Caucasians. This observation indicates the role of MTA1 in disease progression in this cohort and might have clinical relevance in discriminating the subset of less aggressive (Gleason ≤ 7) tumors in African American patients with low MTA1 expression who will remain disease-free from the same subset that have high MTA1 levels indicating a potential of more aggressive disease. In addition, in the “low risk” subpopulation of African Americans (PSA levels < 10 ng/ml) high MTA1 was associated with more aggressive Gleason > 7 tumors suggesting prognostic value for MTA1 in this subgroup of patients.
Both races demonstrated the same, significantly high profile of MTA1 nuclear staining in metastasis. Interestingly, MTA1 cytoplasmic staining, which was very similar in all samples, showed statistically significant decreased levels in metastatic tissues. Given our initial finding of MTA1 as a part of the bone metastatic signature21, the bone metastatic tissues were of primary interest (23/30, 77% cases). Although we confirmed our previous finding of intensive nuclear MTA1 bone-metastatic staining in all 23 cases in the current study, our initial hypothesis on MTA1 as a bone metastatic site-specific marker did not prove to be true. The data demonstrated that rigorous exclusive nuclear MTA1 staining was characteristic for all metastatic tissues examined, including lymph nodes and central nervous system. The majority of metastatic cases were from African Americans (20/30, 67%), however, no conclusion can be made from this fact regarding MTA1 race-dependent prevalence of metastatic PCa. Unfortunately, the lack of matched primary and metastatic prostate tumors and sufficient clinical information preclude us from drawing firm conclusions regarding the clinical relevance of nuclear MTA1 overexpression in metastatic lesions.
To evaluate if MTA1 can serve as a tissue biomarker of recurrent PCa, we assessed the association between MTA1 nuclear expression and disease recurrence. The analysis revealed a statistically significant correlation (p = 0.02) between high MTA1 nuclear expression and recurrent disease. When stratified by Gleason subgroups, there was a trend towards correlation of high MTA1 and recurrence. Nevertheless, no significant association was detected between MTA1 nuclear overexpression and other clinical parameters (preoperative PSA, follow-up PSA, capsule invasion, positive margins and age).
Limited reports exist on the prognostic value of MTA1 in human cancers. Although an association of MTA1 expression and PCa progression was established, puzzling results were reported on an association between higher MTA1 expressions with lower rates of disease recurrence for localized PCa28. To the best of our knowledge, the whole cohort of the abovementioned study consisted of Caucasians. Interestingly, we also found high levels of MTA1 in localized PCa in Caucasian Americans and no prognostic value of MTA1 in this cohort. In our study, the prognostic value of MTA1 in PCa was only evident in the African American population. On the other hand, a recent report indicated significantly worse disease-free and overall survival in the MTA1-positive colon cancer patients, indicating a potential prognostic value of MTA1 expression for colon cancer29.
The importance of MTA1 overexpression and its nuclear localization in PCa is multi-factorial. First, MTA1 is a critical transcription factor and epigenetic modifier which is a part of the nucleosome remodeling and deacetylation (NuRD) co-repressor complex involved in histone deacetylation and gene-specific transcriptional regulation30,31,32. Therefore, nuclear localization of MTA1 explains genomic and epigenomic functions of MTA1, which acts as a global transcriptional suppressor and translational modifier. For example, we have shown that MTA1 participates in the deacetylation of p53 since MTA1 silencing through RNAi increases p53 acetylation and significantly sensitized PCa cells to resveratrol-dependent p53 acetylation and apoptosis22. On the other hand, MTA1 localization in the cytoplasm suggests possible nongenomic functions for MTA1 in PCa33. Second, in the current paper we demonstrated that MTA1 expression was restricted to the nucleus in all PCa cell lines tested and that nuclear overexpression was associated with metastatic potential of cells: the highest level was detected in the most aggressive PC3M cells, high levels were detected in androgen-resistant Du145, decreased levels were in androgen-sensitive LNCaP and virtually no expression was detected in RWPE-1 cells. Third, using these cell lines we have recently shown that inhibition of MTA1 by RNAi technology or pharmacological agents decreases metastatic potential of cells in vitro and in vivo21,22,23. MTA1 knockdown PCa orthotopic xenografts developed significantly smaller tumors and less metastasis compared to xenografts with MTA1-expressing tumors23.
The clinical significance of our findings is also three-fold: prognostic, therapeutic and chemopreventive. Prognostic: We found that MTA1 is a tissue biomarker for PCa aggressive disease and metastasis in African American patients. Identifying a biomarker for aggressive disease, specifically for African Americans, can be of great importance since the established clinicopathological parameters and molecular markers are still insufficient for accurate prognosis of cancer progression. We suggest biopsy MTA1 screening of Gleason ≤ 7 tumors and low PSA (< 10 ng/ml) subset of African American patients at risk of high MTA1 nuclear levels and more aggressive disease. Interestingly, a recent study identified MTA1 by serological screening of PCa cDNA libraries: MTA1 antigen reacted with PCa sera tested, but not with normal sera34. This finding suggests that MTA1 may be released into the secretions and/or blood after shedding from the PCa cells, therefore there is a strong possibility that a MTA1 serum immunoassay can be developed as an indicator of disease relapse. In the future, we will develop an immunoassay for MTA1 detection in the serum or urine of PCa patients since there is no commercially available MTA1 ELISA. Therapeutics: Silencing MTA1 by MTA1 knockdown (shRNA) in PCa cells significantly decreased their metastatic potential in vitro and tumor development in subcutaneous and orthotopic xenografts mostly due to inhibition of angiogenesis and induction of apoptosis21,22,23. These data suggest that future MTA1-targeting therapy for metastatic PCa may belong to so-called “tumor depriving” agents that belong to the next generation of anti-angiogenic drugs with less toxicity than chemotherapeutic agents. In addition, histone deacetylase (HDAC) inhibitors and PI3K inhibitors showed promising results on MTA1 inhibition in PCa cells (unpublished data) and a possible use of these clinically approved agents in MTA1-overexpressing PCa can be considered but needs to be evaluated. Chemoprevention: We and others, have previously shown that African Americans develop PCa at younger age with greater volumes and higher Gleason score15. Diet is associated with cancer and may play role in the racial disparities. We recently reported that dietary stilbenes, resveratrol and its potent analogue pterostilbene, by down-regulating MTA1 demonstrate potent anticancer and antimetastatic properties in PCa cells in vitro and in orthotopic xenografts22,23. Given that the PCa risk is 66% greater in African Americans than among Caucasians, our findings of MTA1 as a target of dietary stilbenes is very promising and may have both therapeutic and chemopreventive public health significance. Therefore, putting together results of the current study and our previous finding that MTA1 can be downregulated by dietary stilbenes found in berries and red wine, we emphasize new perspectives for PCa chemoprevention. We believe that it is important to inform African American men in our communities about the chemopreventive qualities of dietary products and encourage them to modify their diet and drinking habits.
In summary, this study demonstrated that MTA1 nuclear overexpression correlates with higher risk for Gleason > 7 tumors and recurrent disease, particularly in African Americans. The subset of African American patients with Gleason ≤ 7 and PSA < 10 ng/ml which is considered as low risk population may benefit from evaluation of MTA1 levels as high levels of MTA1 will indicate an otherwise overlooked aggressive progression of the disease. African American men at an increased risk of PCa incidence and/or recurrence may benefit from resveratrol/analogues dietary intervention for maintaining low levels of MTA1. In the future, resveratrol and its analogues may be used as dietary supplements for MTA1 inhibition in chemopreventive settings, while HDAC inhibitors and PI3K inhibitors alone and in combination with stilbenes may be considered as therapeutic agents. Additional studies addressing the importance of high baseline nuclear expression of MTA1 in Caucasian Americans may be helpful in furthering our understanding of the role of MTA1 in pathogenesis and progression of PCa.
Methods
Specimens and clinical information
We used specimens and clinicopathological data from the Pathology File of UMMC, Jackson, MS and from the case files from the Pathology Department of University of Iowa Hospitals and Clinics, Iowa City, IA. From the total 302 cases, the majority of the samples were from Mississippi (254), while the remaining 48 were from Iowa. Pathology reports for each surgical specimen were independently reviewed by pathologists from Mississippi and Iowa. Several cases from the Mississippi cohort which turned out to be either multiple entries of the same tumor from a single patient or with conflicting information were excluded from the study. Finally, there were 291 samples: 147 African Americans and 144 Caucasian Americans. This included 30 metastatic PCa from the Mississippi database (20 African Americans and 10 Caucasian Americans). Of the patients from the Mississippi cohort, 28 pairs of recurrent and non-recurrent localized PCa samples were selected and matched by race and age, 19 African Americans and 9 Caucasian Americans. The cases from Iowa were all from Caucasian Americans with the exception of one Hispanic, which was excluded from the study. These samples consisted of 24 non-matched pairs of recurrent and non-recurrent groups. Clinicopathological characteristics included age, race, different pathologic categories, Gleason score, capsule invasion and surgical margins. Availability of pre-operative PSA levels was limited to 96 cases and follow-up PSA levels were limited to 48 cases. Clinically localized PCa cases were grouped as low Gleason score (< 7), intermediate ( = 7) and high Gleason score (>7). In some analyses, low and intermediate Gleason scores were considered together. Cases were also grouped and analyzed as non-recurrent (NR) and recurrent (R) and by race: African Americans (AA) and Caucasian Americans (CA). This collaborative study was approved by the Institutional Review Boards of both institutions.
Tissue microarrays
Of the 254 samples from UMMC, representative tissue blocks of formalin-fixed, paraffin-embedded (FFPE) primary and metastatic tumors were selected for Tissue MicroArrays (TMAs) construction. The selection was done on the basis of verified histological features, which then were topographically correlated with the corresponding paraffin blocks. A 2 mm cylindrical core from each selected site of the primary FFPE block was transferred to the composite paraffin blocks to construct TMA blocks by using a Beecher MTA1 Manual Tissue Arrayer (Beecher Instruments, Sun Prairie, WI). The resulting TMA blocks were then sectioned at 5 μm in thickness for IHC analysis. Data was analyzed by patient and not sample numbers.
Immunohistochemistry
Immunohistochemical analysis was conducted on TMAs (UMMC) and FFPE whole sections (University of Iowa) following standard protocol. Two antibodies against MTA1, A-11 and C-17 were purchased from Santa Cruz Biotechnology, CA and compared for specificity and reproducibility in a pilot setting. MTA1(A-11) is a mouse monoclonal antibody raised against amino acids 513–678 of human MTA1 and MTA1(C-17) is a goat polyclonal antibody raised against a peptide mapping at the C-terminus of human MTA1. In agreement with our previous report21, the specificity and reproducibility of MTA1 (A-11) proved to be superior and it was subsequently used on all cases in this study. Detection of MTA1 was conducted using the VECTASTAIN Elite ABC kit (Vector laboratories, CA). 3,3′-diaminobenzidine was used as chromogen and slides were counterstained with hematoxylin. Briefly, sections were deparaffinized, rehydrated with xylene and descending grades of water and alcohol. Antigen retrieval was performed by boiling the slides in Antigen Unmasking Solution (Vector Laboratories, CA) for 30 min in a steamer. After quenching endogenous peroxidase activity and blocking, the slides were incubated overnight with MTA1 A-11 (1:200) antibody. Detection was achieved by using the ImmPACT DAB kit (Vector Laboratories, CA). Negative controls were performed by omitting the primary antibody. Images were viewed and recorded on Nikon Eclipse E400 and Olympus BX41 plus DP70 camera microscopes.
Analysis of immunohistochemical staining
Evaluation of stained slides was done independently by two board certified pathologists (MI and MG) by scoring intensity and frequency of staining21. The MTA1 expression was recorded as subcellular localization (nuclear (N), cytoplasmic (C) or both) as well as intensity and frequency of the signal. Total Score (TS) was defined as intensity × frequency (% or fraction). The staining intensity was scored as following: −, no staining (0), +, weak (1); ++, moderate staining (2); +++, strong staining (3). The frequency of MTA1 expression was scored as% of positively stained cells. For example, if staining for the tumor was with intensity ++, moderate staining (2) and the frequency was 17%, then TS was calculated as 2 × 0.17 = 0.34.
Cell culture
DU145 and LNCaP cells were obtained from the American Type Culture Collection and maintained in RPMI 1640 medium containing 10% FBS as previously described21,22. RWPE1, (courtesy of Dr. Thumbikat, Northwestern University, Chicago), normal prostate epithelial cells, were maintained in EpiLife medium supplemented with human keratocyte growth factor (HKGS; Cascade Biologics). MDA PCa 2b cells were a gift from Dr. C Lee and PC3M cells were a gift from Dr. R. Bergan (Northwestern University, Chicago).
Western blot analysis
Western blot analysis was done as described previously21,22,23. Briefly, the cells were fractionated using NE PER Nuclear and Cytoplasmic extraction reagents (Thermo Scientific, Pierce Biotechnology, IL) according to the manufacturer's instructions. The protein concentration was measured using the Bio-Rad protein assay reagent (Bio-Rad Laboratories, Hercules, CA). Equal amounts of protein (70 μg) were resolved in 10% Tris-TGX Ready gels and transferred to a PVDF membrane by Mini Trans-Blot Electrophoresis Transfer System (Bio-Rad Laboratories, Hercules, CA). The membranes were then blocked with TBS-Tween and 5% dry milk for 2 hours at room temperature and probed with MTA1 (A-11) (Santa Cruz Biotechnology, Santa Cruz, CA) antibodies. The blots were probed with Erk (Cell Signaling Technology, Inc., Danvers, MA) and lamin A (Santa Cruz Biotechnology, Santa Cruz, CA) as loading controls. Signals were visualized using enhanced chemiluminescence.
Statistical analysis
Descriptive data are presented as percentages or means and SD/SE, as appropriate. Because the distributions of total cytoplasmic score (TCS) and total nuclear score (TNS) were skewed, values were transformed to natural logs. TNS:TCS ratios were calculated where TCS > 0. Statistical hypothesis testing of differences between groups was carried out using t tests or ANOVA (with Bonferroni correction for post-hoc tests), as appropriate. Logistic regression was used to estimate the independent association of TNS, PSA level, margin involvement and capsule involvement with tumor recurrence. The differences were considered significant at p ≤ 0.05. All statistical analyses were done using SAS 9.1.3 (SAS Institute Inc., Cary, NC).
References
Tollefson, M. K., Karnes, R. J., Rangel, L. J., Bergstralh, E. J. & Boorjian, S. A. The impact of clinical stage on prostate cancer survival following radical prostatectomy. J. Urol. 189, 707–712 (2013).
Bryniarski, P., Paradysz, A. & Fryczkowski, M. PSA mass as a marker of prostate cancer progression after radical prostatectomy. Medical science monitor: Int. Med. J. Exp. Clin. Res. 17, CR104–109 (2011).
Stephenson, A. J. et al. Prostate cancer-specific mortality after radical prostatectomy for patients treated in the prostate-specific antigen era. J. Clin. Oncol. 27, 4300–4305 (2009).
Salonia, A. et al. Preoperative sex steroids are significant predictors of early biochemical recurrence after radical prostatectomy. World J. Urol. 31, 275–280 (2013).
Pierorazio, P. M. et al. Preoperative characteristics of high-Gleason disease predictive of favorable pathological and clinical outcomes at radical prostatectomy. BJU Int. 110, 1122–1128 (2012).
Masieri, L. et al. The role of free to total PSA ratio in prediction of extracapsular tumor extension and biochemical recurrence after radical prostatectomy in patients with PSA between 4 and 10 ng/ml. Int. Urol. Nephrol. 44, 1031–1038 (2012).
Han, M. et al. Biochemical (prostate specific antigen) recurrence probability following radical prostatectomy for clinically localized prostate cancer. J. Urol. 169, 517–523 (2003).
Pound, C. R. et al. Natural history of progression after PSA elevation following radical prostatectomy. JAMA 281, 1591–1597 (1999).
Stephenson, A. J. et al. Postoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J. Clin. Oncol. 23, 7005–7012 (2005).
Loeb, S. & Catalona, W. J. Prostate-specific antigen screening: pro. Curr. Opin. Urol. 20, 185–188 (2010).
Stephenson, A. J. et al. Integration of gene expression profiling and clinical variables to predict prostate carcinoma recurrence after radical prostatectomy. Cancer 104, 290–298 (2005).
Bismar, T. A. et al. Defining aggressive prostate cancer using a 12-gene model. Neoplasia 8, 59–68 (2006).
Jemal, A. et al. Cancer Statistics, 2010. CA Cancer J. Clin. 60, 277–300 (2010).
Hsing, A. W. & Chokkalingam, A. P. Prostate cancer epidemiology. Front. Biosci. 11, 1388–1413 (2006).
Zhou, X., Bigler, S. & Pound, C. Age disparities in diagnosis of prostate cancer between African Americans and Caucasians. Ageing International 37, 186–194 (2012).
Bigler, S. A., Pound, C. R. & Zhou, X. A retrospective study on pathologic features and racial disparities in prostate cancer. Prostate Cancer 2011, ID 239460 (2011).
Rundle, A. et al. A prospective study of socioeconomic status, prostate cancer screening and incidence among men at high risk for prostate cancer. Cancer Causes Control 24, 297–303 (2013).
Rohrmann, S. et al. Serum estrogen, but not testosterone, levels differ between black and white men in a nationally representative sample of Americans. J Clin. Endocrinol. Metab. 92, 2519–2525 (2007).
Caruso, R. P. et al. Altered N-myc downstream-regulated gene 1 protein expression in African-American compared with Caucasian prostate cancer patients. Clin. Cancer Res. 10, 222–227 (2004).
Lai, G. Y. et al. Racial variation in umbilical cord blood leptin concentration in male babies. Cancer Epidemiol. Biomarkers Prev. 20, 665–671 (2011).
Kai, L. et al. Targeting prostate cancer angiogenesis through metastasis-associated protein 1 (MTA1). Prostate 71, 268–280 (2011).
Kai, L., Samuel, S. K. & Levenson, A. S. Resveratrol enhances p53 acetylation and apoptosis in prostate cancer by inhibiting MTA1/NuRD complex. Int. J. Cancer 126, 1538–1548 (2010).
Li, K. et al. Pterostilbene acts through metastasis-associated protein 1 to inhibit tumor progression and metastasis in prostate cancer. PLoS ONE 8, e57542 (2013).
Toh, Y. et al. Overexpression of metastasis-associated MTA1 mRNA in invasive oesophageal carcinomas. Br. J. Cancer 79, 1723–1726 (1999).
Sasaki, H. et al. Expression of the MTA1 mRNA in advanced lung cancer. Lung Cancer 35, 149–154 (2002).
Jang, K. S. et al. MTA1 overexpression correlates significantly with tumor grade and angiogenesis in human breast cancers. Cancer Sci. 97, 374–379 (2006).
Iguchi, H. et al. Expression of MTA1, a metastasis-associated gene with histone deacetylase activity in pancreatic cancer. Int. J. Oncol. 16, 1211–1214 (2000).
Hofer, M. D. et al. The role of metastasis-associated protein 1 in prostate cancer progression. Cancer Res. 64, 825–829 (2004).
Higashijima, J. et al. Expression of histone deacetylase 1 and metastasis-associated protein 1 as prognostic factors in colon cancer. Oncol. Rep. 26, 343–348 (2011).
Toh, Y., Pencil, S. D. & Nicolson, G. L. A novel candidate metastasis-associated gene, mta1, differentially expressed in highly metastatic mammary adenocarcinoma cell lines. cDNA cloning, expression and protein analyses. J. Biol. Chem. 269, 22958–22963 (1994).
Xue, Y. et al. NURD, a novel complex with both ATP-dependent chromatin-remodeling and histone deacetylase activities. Mol. Cell 2, 851–861 (1998).
Molli, P. R., Singh, R. R., Lee, S. W. & Kumar, R. MTA1-mediated transcriptional repression of BRCA1 tumor suppressor gene. Oncogene 27, 1971–1980 (2008).
Kumar, R. et al. A naturally occurring MTA1 variant sequesters oestrogen receptor-alpha in the cytoplasm. Nature 418, 654–657 (2002).
Geng, L. et al. Identification of Metastasis Associated Antigen 1 (MTA1) by Serological Screening of Prostate Cancer cDNA Libraries. Open Biochem. J. 2, 100–107 (2008).
Acknowledgements
We are grateful to Dr. Steven Bigler (Pathology Department, UMMC) for his contribution to the study. We are also grateful to Dr. Lucio Miele (Cancer Institute, UMMC) for valuable discussions.
Author information
Authors and Affiliations
Contributions
Both S.J.D. and X.Z. contributed equally to the carrying out the experiments and analysis of the data. Z.H., S.D. and L.Z. carried out IHC and western blot analysis, M.I. and M.P.G. evaluated and analyzed IHC data, A.D.P. and S.V. contributed to the analysis and interpretation of data. A.S.L. contributed to the conception, design, analysis and interpretation of data. A.S.L. supervised the study and wrote the manuscript with assistance from S.J.D., X.Z. and A.D.P.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary Tables and Full-lenght blots
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Dias, S., Zhou, X., Ivanovic, M. et al. Nuclear MTA1 overexpression is associated with aggressive prostate cancer, recurrence and metastasis in African Americans. Sci Rep 3, 2331 (2013). https://doi.org/10.1038/srep02331
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep02331
This article is cited by
-
Clinical implications of MTA proteins in human cancer
Cancer and Metastasis Reviews (2014)
-
Expression of MTA1 in nasopharyngeal carcinoma and its correlation with prognosis
Medical Oncology (2014)
-
MTA family of proteins in prostate cancer: biology, significance, and therapeutic opportunities
Cancer and Metastasis Reviews (2014)
-
Properties and clinical relevance of MTA1 protein in human cancer
Cancer and Metastasis Reviews (2014)
-
Subcellular localization of MTA proteins in normal and cancer cells
Cancer and Metastasis Reviews (2014)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.