Key Points
-
Discusses how difficult it can be to rehabilitate oral cancer patients.
-
Shows that most oral cancer patients may need referral to specialist rehabilitation.
-
Presents a novel way of rehabilitating oral cancer patients with a prosthesis which has the benefits of both a fixed and removable prosthesis.
-
Describes the complication rate associated with this prosthesis.
Abstract
Surgical resection of an oral tumour (and the associated free flap reconstruction) can significantly alter the oral anatomy. The lack of sulcus depth, alveolar ridge, presence of a mobile flap and limited tongue movement can make it impossible for patients to control a removable prosthesis. To help this cohort of patients, dental implants can be invaluable. The Oral Rehabilitation Team at Central Manchester University Dental Hospital have used dental implants to rehabilitate oral cancer patients for over thirty years. After their resective surgery, a number of patients were dentally rehabilitated with a laboratory-made, precious metal-alloy bar supported by at least four dental implants. A metal-alloy under-sleeve retained overdenture was then provided to fit over the milled bar. The majority of the 50 patients in this case series had tumours in the anterior floor of the mouth. It was noted that 76% of the patients received a rim resection and were reconstructed with a fasciocutaneous, soft tissue free flap. Six percent of patients received a segmental resection and were reconstructed with either a fibular or deep circumflex iliac artery free flap. The dental implants and sleeve overdentures had a survival rate of 100%. None of the dentures lost retention, implying that the frictional grip between the overcasting and the milled bar was sufficient to appease the retention demands of this cohort. However, 10% of patients encountered complications. This would suggest a success (or complication free) rate of 90% for this cohort of 50 oncology patients. This would still imply that milled bars/sleeve overdentures carry a relatively low maintenance burden and may be a useful treatment option for oral cancer patients.
Similar content being viewed by others
Introduction
The dental rehabilitation of oral cancer patients can be challenging for both the patient and clinician alike. Patients may have had a combination of non-surgical and surgical therapy to manage their malignancy which may result in both anatomical changes as well as trismus. Treatment modalities include radiotherapy (RT), chemotherapy (CT) and surgical resection (SR) with free flap reconstruction (FFR). The side effects of radiotherapy on the oral cavity are notoriously well known to the members of the oral rehabilitation team and include mucositis, dysphagia and xerostomia. Surgical resection of an oral tumour (and the associated free flap reconstruction) can significantly alter the oral anatomy. The lack of sulcus depth, alveolar ridge, presence of a mobile flap and in some cases, limited tongue movement, can make it impossible for patients to control a removable prosthesis. To help this cohort of patients, dental implants can sometimes prove to be invaluable.
The York Consensus1 has recommended that the minimum standard of care for the edentulous mandible should be an over denture retained by two implants. Regardless of the type of attachment system used (ball, bar or magnet), patients are significantly more satisfied with a two implant overdenture than with new conventional dentures.1 Edentulous patients find the implant overdentures significantly more stable, comfortable and more easy to speak and function with. They also have higher quality of life scores than patients wearing conventional dentures.1
Unfortunately, no such consensus statement exists for edentulous oncology patients, which is disappointing given the unique prosthodontic challenges which they may present with. Dental implants have been successfully used to support and retain overdentures in oral cancer patients for many years now. Linsen et al.2 analysed oral cancer patients with implant overdentures retained by balls and bars, and reported an implant survival rate of 87% at ten years. Other groups have reported survival rates of 98% at an average follow up of 62 months.3 Rogers et al.4 demonstrated that oral cancer patients with implant retained overdentures are more satisfied with their prostheses than those with just conventional dentures. Schoen et al.5 similarly suggested that implant retained overdentures can improve quality of life scores, oral function and denture satisfaction in head and neck cancer patients. These improvements in oral function and denture satisfaction are maintained for at least five years post denture delivery.6
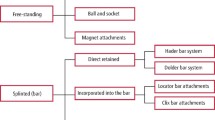
A number of attachment systems have been used to retain complete dentures in oral cancer patients. These include ball attachments,7 magnets8 and bars.9 The number of implants used to retain/support a complete denture varies from two to four in the literature.10 The number of fixtures prescribed depends on a number of factors including the anatomical form of the arch being restored, the opposing dental arch, the type of attachment used, tongue/swallowing function, patient expectations and whether the patient has had post-operative radiotherapy. Schoen et al.11 have suggested that for patients who have had radiotherapy, at least four implant fixtures are required in the mandibular arch to support a prosthesis. This number of implants was shown to relieve any undue pressure on the underlying soft tissues. In comparison to patients who have not had radiotherapy, two implant fixtures have been shown to be sufficient to retain a mandibular complete denture.
The Oral Rehabilitation Team at Central Manchester University Dental Hospital have used dental implants to rehabilitate oral cancerpatients for over thirty years now. A large proportion of these patients had been rendered partially dentate or completely edentulous after their ablative cancer therapy. Patients were dentally rehabilitated with multiple implants that were restored with a cast, laboratory made, precious metal-alloy bar. A metal-alloy under-sleeve retained overdenture was then provided to fit over the cast precious metal bar.
This case series will describe the use of these cast precious metal bars and sleeve overdentures in oral cancer patients. We will describe the design features and advantages of this prosthesis. We will also describe its survival and complication rate.
Aim
To describe the use of dental implants, cast precious metal bars and sleeve overdentures in this case series of oral cancer patients.
Objective
-
To describe the design features and advantages of prescribing cast bars/sleeve overdentures for oral cancer patients
-
To describe the survival and complication rates of this prosthesis at Central Manchester University Dental Hospital.
When should milled bar and sleeve overdentures be prescribed?
Patients who have had ablative surgery as part of their oral cancer treatment will present with a different anatomical appearance from a non-oral cancer patient. The extent of the resection, residual denture bearing anatomy, prognosis of remaining teeth and remaining tongue function will determine whether the patient can control a conventional denture. If the edentulous oral cancer patient still has the majority of their denture bearing area intact with alveolar ridges of good height/width and good tongue swallowing function, a conventional complete denture can be prescribed as a first line treatment (Fig. 1).
(a) An edentulous oral cancer patient who had all of his denture bearing area intact and good tongue control post cancer surgery (b) The patient previously had a squamous cell carcinoma (SCC) of his left buccal mucosa. The tumour was resected and reconstructed with a radial forearm free flap (RFFF). He was successfully rehabilitated with complete dentures
However, some patients may have had an extensive tumour resected and reconstructed with a large composite free flap. The altered anatomy, presence of a bulky flap, lack of sulcus depth, alveolar ridges and altered tongue function can make it impossible for patients to control a removable prosthesis, even one retained by dental implants. Furthermore if the patient has had radiotherapy, the presence of a mobile prosthesis on irradiated tissue may cause trauma and could promote osteoradionecrosis. Under these circumstances, the provision of a fixed, implant supported superstructure is advised.
An implant supported bridge restoration may in some cases be preferred by patients for a fixed natural feel. The lack of soft tissue contact makes it ideal to restore irradiated sites as it cannot traumatise the underlying mucosa. However, a fixed bridge cannot provide lip support. Clinicians will also require extra caution when examining the underlying ridge for recurrences, especially if there is substantial gingival acrylic attached to the fixed bridge for improved cosmetics. Superstructures must therefore be designed to ensure that they are cleansable and allow for surveillance of new tumours.
To combine the advantages of both a fixed and removable prosthesis, patients can be provided with multiple dental implants to support a cast metal bar. A corresponding sleeve overdenture was made to fit precisely over the bar but have minimal contact with the underlying soft tissues. This arrangement would allow a patient to be provided with lip support via the denture, yet still have a superstructure that was securely anchored by dental implants. The removable nature of the prosthesis also allows clinicians to check around the implants and ensure that the cancer has not reoccurred.
Design features of the cast precious metal bar/sleeve overdenture
Most patients described in this case series were rehabilitated with four dental implants in the native/reconstructed anterior mandible. The fixtures were restored with a cast gold-alloy bar. The bar was laboratory milled to have a zero degree taper. This taper was found to maximise retention of the sleeve overdenture through pure frictional grip. Some groups have used a four-degree taper for their metal bars.12 However, they also needed to incorporate additional attachments systems within the bar to help retain the sleeve. The use of a zero degree taper negates the need for additional retentive components.
All dental implants were placed in native residual anterior mandibular bone or the bone of the free flap and were allowed to osseointegrate for at least four months. The bone may or may not have received radiotherapy. If radiotherapy was provided the dose, fractionation, exact site, modality of radiotherapy as well as a CBCT scan to assess bony changes were all assessed to evaluate possible risks. All implants were placed according to a two-stage procedure and allowed to be buried at the time of placement. After four months, the implants were exposed. Any necessary soft tissue surgery (such as a vestibuloplasty or free gingival grafting) was performed at this stage whilst healing abutments were attached to the implants.
After the peri-implant soft tissues had matured around the healing abutments, transmucosal abutments were placed at the appropriate height. Pick up impression copings were subsequently used to take an abutment level impression in a special tray with polyether impression material. Once the accuracy of the master casts had been confirmed with a verification jig, wax rims were used to record the patient's occlusal scheme. These were used to mount the master casts and a tooth set-up was produced. The set-up and mounted models could then be analysed to ensure that there was sufficient inter-occlusal clearance to accommodate the bar and overdenture. The tooth trial was then tried in clinically to verify the proposed tooth position.
The technical team would then capture an index of the tooth set-up before waxing up the bar. The bar was milled to have a zero-degree taper and then cast in precious metal gold alloy. The milled bar was then tried in clinically to check fit and passivity. It was then returned to the technical team to wax-up the corresponding sleeve. The sleeve was designed to fit precisely over the milled bar without relief. This means that the overdenture feels as nearly as retentive as a fixed, implant supported bridge. The sleeve was then cast in precious metal alloy before having the acrylic flanges and teeth added using the lost wax technique.
The milled bar was then fitted and the sleeve overdenture was delivered (Fig. 2). The patient was then routinely followed up one to two weeks later. Patients were subsequently followed up at a head and neck multidisciplinary team (MDT) clinic on a six month to annual basis. Any complications with the prosthesis were noted. The maxillofacial surgeons and restorative dentists asked patients to remove the overdenture at these appointments so that the soft tissues could be surveyed for tumour re-occurrence (Fig. 3).
The patient received four mandibular implants and a precious metal bar. (b) The corresponding sleeve overdenture for the patient shown in Figure 2 (a). (c) The definitive maxillary complete denture and mandibular sleeve overdenture
(b) The cast bar in the mandible was supported by four implants. (c) Once the mandibular sleeve overdenture was removed, a squamous cell carcinoma was found to have re-occurred underneath the two implants on the left hand side. (d) The inferior surface of the sleeve overdenture after removal. This was an earlier sleeve overdenture with additional (but unnecessary) retentive attachments incorporated into the metal sleeve
All metal frameworks used to support the superstructures were laboratory cast in precious metal alloy. An alternative to this are computer aided designed (CAD), milled, titanium frameworks (Fig. 4). They are light weight and do not suffer from problems with casting shrinkage or porosity. CAD designed bars are relatively quick to mill and allow a digital copy of the framework to remain should the metalwork need remaking. Although the CAD designed titanium metal bars and sleeves were found to be equally effective as the precious metal counterpart, the cost was found to be prohibitive. The cost of a cast, precious metal alloy bar and sleeve was £600. The cost of a CAD, milled, titanium bar and sleeve was £1600. Given the excellent support provided by the in-house technical team, and the desire to preserve NHS funding where possible, the authors currently prescribe cast, laboratory made metal bars. They are, however, looking to develop an efficient and cost-effective digital service.
Data collection
All cast bars/sleeve overdentures were constructed at Manchester University Dental Hospital by the in-house laboratory. Any item constructed is logged on a computer database by the administrators in the laboratory. The authors used the database search engine to locate all milled bars constructed at Manchester Dental Hospital.
The authors then obtained the patient notes of all patients who had a cast, precious metal, milled bar/sleeve overdenture constructed. Any patient who had the prosthesis constructed as part of their oral cancer rehabilitation was included in this case series. These included patients receiving ablative resective surgery for an oral cancer, free flap reconstruction and radiotherapy. All head and neck patients are routinely followed up on at least an annual basis by the head and neck MDT. Any details highlighted in the patient notes (such as complications/lack of complications) could verbally be corroborated by one of the authors when the patients were reviewed.
All of the patients' details were anonymised and the following details were collected for each patient: location of oral cancer/details of treatment received/number of dental implants placed/whether fixtures were placed at primary cancer resection surgery/year the implants were placed/last date the overdenture was reviewed by a consultant in restorative dentistry/any complications observed with the implants, peri-implant soft tissues, bar or acrylic superstructure. Examples of complications include loss of retention of the sleeve overdenture, peri-implantitis, early/late implant failure necessitating explantation of the fixture, soft tissue overgrowth around the fixtures, screw loosening, screw fracture and fracture of the acrylic overdenture. The collected data is shown in Table 1.
Results
The majority of patients rehabilitated with milled bars and sleeve overdentures had tumours in the anterior floor of the mouth (Fig. 5). Furthermore all of the patients in this case series had ablative surgery to remove their tumours (Fig. 6). It was noted that 76% of the patients received a rim resection and were reconstructed with a fasciocutaneous, soft tissue free flap. The majority of these flaps (36 patients) were radial forearm free flaps whilst only two patients received an anterolateral thigh flap. Six percent of patients received a segmental resection and were reconstructed with either a fibular or deep circumflex iliac artery (DCIA) free flap (Fig. 6). Eleven out of the 50 patients in this case series also received post-operative radiotherapy as part of their oral cancer management (Table 1).
Ninety percent of the patients in this case series received four implants to support their bar and sleeve overdenture (Fig. 7). One patient received six implants. This was one of the earliest cases treated and probably reflected the operator planning for failure in case any fixtures were lost in the future. One of the more recent cases received five implants. This patient had a lateral floor of mouth tumour, and received a large rim resection. In order to replace the missing dental units and avoid a long cantilever on the bar, five implants were placed at the time of surgery.
Ninety-four percent of the patients had implants placed in their native mandibular bone. The majority of these patients had received a rim resection and reconstruction with a free soft tissue flap. The remaining 6% had their implants placed into a composite fibular or DCIA free flap bone (Table 1).
Thirty-seven of the patients had implants placed as a second stage procedure after receiving any necessary resection, free flap reconstruction or radiotherapy to manage their oral cancer (Table 1). The majority of the 13 who received fixtures at the time of primary surgery received a rim resection. These patients had the fixtures placed into residual native bone before being reconstructed with a fasciocutaneous radial forearm or anterolateral free flap (Table 1).
None of the implant fixtures required explantation and none of the acrylic superstructures required remaking. This would suggest an implant and prosthetic survival rate of 100% in this case series. Ninety percent of patients had no complications with their fixtures/peri-implant tissues or the prosthetic superstructure (Fig. 8). However, 10% of the patients in this case series experienced complications with this mode of treatment. One patient developed peri-implantitis around one of his fixtures. Another patient fractured one of his bridge screws connecting the milled bar to the abutment. The final three patients with complications all reported problems with soft tissue overgrowth around their fixtures. All three patients had radial forearm free flap tissue surrounding their implants.
Discussion
Ten percent of patients in this series encountered complications (Fig. 8). This would imply that milled bars/sleeve overdentures carry a relatively low maintenance burden. From both a patient and clinician point of view, this is important. Although oral cancer patients are followed up by members of the head and neck team post treatment, some units may discharge patients back to their general dentist after any implant based rehabilitation is complete. This may be due to capacity or NHS funding agreements. However, practitioners may not be familiar with attachment systems and are understandably reluctant to maintain implant based superstructures.13 Patients who have been treated with implants and simple locator retained overdentures have problems such as loss of retention and abutment loosening.14 If some practitioners are reluctant to manage such maintenance issues, patients could be put at significant inconvenience when problems occur. It is therefore encouraging that the complication rate (and maintenance burden) was relatively low in this case series (Fig. 8). However, longer follow up periods are needed to check whether or not this is indeed the case.
Of the five patients in this series who did encounter complications, one developed peri-implantitis. He had no obvious risk factors as he did not smoke and had no apparent history of periodontal disease. His superstructure was cleansable and the patient was maintaining good plaque control. The surgical notes implied that the implants were within the boney envelope and had excellent primary stability. Even so, the fixture started to demonstrate pathological levels of bone loss. This was arrested with non-surgical periodontal therapy, antimicrobials and open flap debridement.
Three patients in this case series had problems with soft tissue overgrowth of the surrounding free flap around the fixtures. One patient needed to have his free flap debulked. The other two also needed to have autogenous, free gingival grafts placed around the fixtures to normalise the peri-implant tissue and increase the surrounding band of keratinised tissue.15 These three patients subsequently reported no problems with cleaning around the implants or problems with soft tissue overgrowth of the peri-implant tissues. For future cases, if the free flap overlying the fixtures is particularly bulky the authors would strongly recommend: debulking; normalising the surrounding implant tissues with free gingival grafts; and performing a vestibuloplasty. This will make it easier for patients to clean their implants and to prevent similar problems from occurring.
Cordaro et al.16 have already reported that patients may find it difficult to clean around milled bars compared to other attachment systems like locator abutments. They noted that fixtures restored with locator attachments had lower bleeding on probing scores and pocket depths than fixtures supporting a milled bar. Krennmair et al.17 similarly noted that plaque and calculus scores were higher around fixtures supporting milled bars compared to those supporting telescopic crowns. Clinicians should therefore perform any necessary mucogingival surgery to ensure that patients can clean around their fixtures. Furthermore bars should be designed to ensure that there is sufficient space between the inferior surface of the bar and the underlying soft tissues to accommodate interdental brushes. The inferior surface should be slightly convex so as not to accumulate plaque. This is paramount to avoid problems with peri-implant mucosal disease.
The final patient who had complications fractured a bridge screw in one of the abutments. This patient was a parafunctionalist and was warned that this problem could be encountered. The abutment (and fractured screw) was removed with the appropriate removal tool. The patient was then provided with a new abutment and bridge screw to unite the milled bar to the underlying abutments. The patient has had no problems since.
The findings of this paper compare well to other groups17,18,19 who rehabilitate edentulous, non-oncology patients with milled bars and sleeve overdentures. They have suggested that milled bars/sleeve overdentures are associated with a high implant success rate and a low maintenance burden. Krennmair et al.12 have also compared milled bars/sleeve overdentures to implant overdentures retained by clips on round bars. The number of maintenance visits was significantly higher for the clip retained overdentures, compared to the milled bar supported prostheses. These findings have been corroborated by Weinlander et al.,20 which is not surprising. The frictional fit between the milled bar and sleeve would reduce any rotational movements of the prosthesis under occlusal load. However, a round bar with clips would allow rotational movements of the prosthesis towards the denture bearing area. With time, this may cause the clips to lose their retention.
In this paper we have described the cohort of oral cancer patients rehabilitated with cast bars and sleeve overdentures. The vast majority of patients had anterior floor of mouth tumours, received rim resections, reconstruction with soft-tissue free flaps and placement of four implants into their residual native mandible (Table 1). The complication rate appeared to be low with this treatment modality (Fig. 8). This finding must be treated with care as the follow up for some patients in this case series was only one year (Table 1). Clearly longer follow up periods are necessary to ascertain the true maintenance burden in this cohort.
Conclusion
As far as the authors know, this is the largest cohort of oral cancer patients that have been provided with cast bars and sleeve overdentures. As a standard protocol, the authors tend to normally recommend the placement of four implants to support the milled bar. If more dental units need to be replaced or unfavourable cantilevers are to be avoided, clinicians may have to provide more fixtures. The majority of implants were placed into native, residual mandibular bone after a rim resection was performed. Ideally, this should be a carried out at the time of ablative surgery to speed up the patient's oral rehabilitation and reduce the number of surgical visits. Implants placed at the time of ablative surgery are normally buried. At the time of exposure, clinicians then have an ideal opportunity to carry out any necessary flap debulking and mucogingival surgery to optimise the peri-implant tissues and facilitate plaque control. The milled precious metal bar can then be constructed. The prosthesis seems to combine the prosthetic advantages of both a fixed appliance (in terms of being retentive and having no soft tissue contact) as well as a removable appliance (in providing lip support and being easily removed to check for tumour recurrence). Although the cost of fabricating the precious metal bar, sleeve and overdenture may be high, this initial cost may be offset by the fact that the prosthesis appears to have a relatively low maintenance burden. However, longer follow up periods and well-designed prospective cohort trials are now needed to confirm whether this is also true for oral cancer patients.
References
Thomason J M, Feine J, Exle C et al., Mandibular two implant-supported overdentures as the first choice standard of care for edentulous patients – the York Consensus Statement. Br Dent J 2009; 207: 185–186.
Linsen SS, Martini M, Stark H . Long-term results of endosteal implants following radical oral cancer surgery with and without adjuvant radiation therapy. Clin Implant Dent Relat Res 2012; 14: 250–258.
Chiapasco M, Gatti C . Implant-retained mandibular overdentures with immediate loading: a 3-to 8-year prospective study on 328 implants. Clin Implant Dent Relat Res 2003; 5: 29–38.
Rogers S N, McNally D, Mahmoud M, Chan M F, Humphris G M . Psychologic response of the edentulous patient after primary surgery for oral cancer: A cross-sectional study. J Prosthet Dent 1999; 82: 317–321.
Schoen P J, Reintsema H, Bouma J, Roodenburg J L, Vissink A, Raghoebar G M . Quality of life related to oral function in edentulous head and neck cancer patients posttreatment. Int J Prosthodont 2007; 20: 469–477.
Korfage A, Schoen P J, Raghoebar G M, Roodenburg J L, Vissink A, Reintsema H . Benefits of dental implants installed during ablative tumour surgery in oral cancer patients: a prospective 5-year clinical trial. Clin Oral Implants Res 2010; 21: 971–979.
Linsen S S, Martini M, Stark H . Long-term results of endosteal implants following radical oral cancer surgery with and without adjuvant radiation therapy. Clin Implant Dent Relat Res 2012; 14: 250–258.
Ishii J, Yoshida T, Yokoo S, Komori T . Use of magnetic abutments for short endosseous implants following a fibula bone graft in an oral cancer patient: a case report. J Oral Implantol 2003; 29: 289–292.
Vecchiatini R, Mobilio N, Barbin D, Catapano S, Calura G . Milled bar-supported implant overdenture after mandibular resection: a case report. J Oral Implantol 2009; 35: 216–220.
Korfage A, Raghoebar G M, Slater J J et al. Overdentures on primary mandibular implants in patients with oral cancer: a follow-up study over 14 years. Br J Oral Maxillofac Surg 2014; 52: 798–805.
Schoen P J, Reintsema H, Raghoebar G M, Vissink A, Roodenburg J L . The use of implant retained mandibular prostheses in the oral rehabilitation of head and neck cancer patients. A review and rationale for treatment planning. Oral Oncol 2004; 40: 862–871.
Krennmair G, Krainhöfner M, Piehslinger E . The influence of bar design (round versus milled bar) on prosthodontic maintenance of mandibular overdentures supported by 4 implants: a 5-year prospective study. Int J Prosthodont 2008; 21: 514–520.
Vere J W, Eliyas S, Wragg P F . Attitudes of general dental practitioners to the maintenance of Locator retained implant overdentures. Br Dent J 2014; 216: E5.
Vere J, Hall D, Patel R, Wragg P . Prosthodontic maintenance requirements of implant-retained overdentures using the locator attachment system. Int J Prosthodont 2012; 25: 392–394.
Kwasnicki A, Butterworth C . 360 degrees peri-implant, keratinised, soft-tissue grafting with stereolithographic-aided dressing plate. Int J Oral Maxillofac Surg 2009; 38: 87–90.
Cordaro L, di Torresanto V M, Petricevic N, Jornet P R, Torsello F . Single unit attachments improve peri-implant soft tissue conditions in mandibular overdentures supported by four implants. Clin Oral Implants Res 2013; 24: 536–542.
Krennmair G, Sütö D, Seemann R, Piehslinger E . Removable four implant-supported mandibular overdentures rigidly retained with telescopic crowns or milled bars: a 3-year prospective study. Clin Oral Implants Res 2012; 23: 481–488.
Krennmair G, Krainhöfner M, Piehslinger E . Implant-supported mandibular overdentures retained with a milled bar: a retrospective study. Int J Oral Maxillofac Implants 2007; 22: 987–994.
Krennmair G, Sütö D, Seemann R, Piehslinger E . Removable four implant-supported mandibular overdentures rigidly retained with telescopic crowns or milled bars: a 3-year prospective study. Clin Oral Implants Res 2012; 23: 481–488.
Weinländer M, Piehslinger E, Krennmair G . Removable implant-prosthodontic rehabilitation of the edentulous mandible: five-year results of different prosthetic anchorage concepts. Int J Oral Maxillofac Implants 2010; 25: 589–597.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ali, R., Al-Khayatt, A. & Barclay, C. The use of dental implants, cast bars and sleeve overdentures in oral cancer patients. Br Dent J 224, 605–613 (2018). https://doi.org/10.1038/sj.bdj.2018.309
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2018.309
This article is cited by
-
Conventional and implant-based mandibular oral rehabilitation for patients with head and neck cancer
British Dental Journal (2022)
-
Restorative aspects of oral cancer reconstruction
British Dental Journal (2018)