Key Points
-
Perfect imperfection – making dentures look like natural teeth and gums.
-
Being brave with tooth positioning and copying nature - selecting the right size and shape of artificial teeth using photometric calculation and assessment.
-
Patient led decision-making at rehearsal – the complete denture “try- in”.
-
Handling the delivery and review stages of complete denture provision.
Abstract
This final article in a series of three on producing complete dentures which the patient considers attractive, describes selecting the denture teeth, setting the front teeth at the chairside, the try-in visits, processing, fitting and reviewing the dentures. The role of the patient as captain of the ship, the dental nurse as the patient's support and liaison officer, and the clinician as the first technical officer is outlined. The use of immediate replay video technology in allowing a patient to see what the trial denture really looks like is described. It is vital that the patient is completely happy with its appearance in every detail before any denture is finished. Dealing with post-fitting aesthetic problems is considered.
Similar content being viewed by others
The materials of denture teeth
'Of course, dentures are essentially social appliances' Per-Olof Glantz.1
Porcelain teeth vs teeth of various resins
Though some practitioners prefer to use porcelain teeth, the majority of dentures are made with resin teeth. The principal reasons for this are: 1) that resin teeth are standard in most dental schools and colleges; and 2) that porcelain teeth have to be mechanically retained in denture base materials, and their retention features, pins in anteriors and holes in posteriors, must be maintained to allow retention. This latter requirement prevents substantial grinding of the neck and back of the tooth where space is limited by a large ridge or implant/overdenture attachments, or too little inter-ridge space. In these circumstances resin teeth are necessary because they bond chemically to the acrylic denture base material. Apart from that, porcelain's disadvantages as a denture tooth material – its noisiness when teeth occlude, their relative brittleness if a denture is dropped onto a hard surface and their abrasiveness when unglazed porcelain (ground or worn) opposes natural teeth – are thought in most cases to outweigh the advantages of extreme stain resistance and significantly greater wear resistance which porcelain teeth have. They are usually more expensive, too, since various stages of their manufacturing have not yet been automated and have to be done by hand. Any post-purchase surface characterisation, such as staining, crack lines, etc requires the use of a porcelain furnace. Few clinics have immediate access to such firing kilns, which makes the addition and removal of characterisations more difficult for the patient to control.
Initially, the poly-methyl methacrylate (PMMA) resins used to make denture teeth were relatively soft and subject to rapid attrition and abrasion. However, improvements in chemistry and manufacturing have been continuous and today's resin teeth are harder and more stain-resistant than before. Composite resins are used in some makes to improve wear resistance especially of posterior teeth, though these materials are more prone to staining and being chipped. Also, because of their filler particles, composite resins are also less translucent, which has a negative influence when pronounced incisal edge translucency is required in the outer enamel layer. Composite is therefore more useful in posterior teeth.
Choosing denture teeth for complete dentures
Anterior teeth
When a dentist extracts someone's front teeth and throws them in the hazardous waste bin, a usual procedure, precious evidence is being thoughtlessly disposed of. Those teeth would have become a great help in the selection of denture teeth for any future dentures. They are not useful for shade selection because teeth undergo marked colour changes as they dry out, but in every other respect – size, shape and surface detail – they cannot be improved on as records of the natural dentition; they were the natural dentition. We therefore advocate that dental practitioners wash extracted teeth, pack them discreetly in some suitable small container and offer them to the patient to keep for reference as new dentures are made in the years to come. No doubt some patients will find the idea distasteful and decline the offer, but many patients will see the good sense of not simply throwing away these valuable personal records. Some may even find that their possession helps the grieving process that a surprising number of people experience when deprived of natural teeth. But, as we have said, few patients are given that option. In the absence of natural teeth, how have clinicians gone about choosing front teeth for patients?
Aesthetic fallacies still used to select the moulds of anterior denture teeth
Over the years, associations between various facial measurements and the size or shape of front teeth have been proposed and still are found in up-to-date textbooks. To be fair, some of these ideas date from eras before 'smile photography' had arrived and there was probably no remaining image of the discarded natural teeth. Reviews of the history of denture tooth form selection may be found in Ibrahimagić et al.2 and Kumar, et al.3 A commonly cited 'concept' for choosing teeth is Leon Williams' suggestion4 that the shape of an upper central incisor would harmonise with the face if chosen to resemble the inverted outline of the individual's face (viewed from the eyebrows down). He distinguished square, tapering and ovoid teeth, groupings still used in the mould charts of today's manufacturers. Other proposals have referred front tooth size and shape to: personality, gender, age, the profile of the face viewed from the side, the width of the nose, the width of the face, the shape of the residual ridge, the outline form of the fingernail (!) and even the distance from the chin to the hair line (an unstable reference for many older men).
What all these methods have in common is: 1) that they are based on no evidence – on the contrary, when tested with dentate subjects in later studies, no such correlations have been found; and 2) that they are anyway biologically improbable.5 As an example, for Leon Williams' popular inverted face concept to be historically accurate for anyone, the shape of the upper central incisor and of that individual's face would need to be under the control of a single genetic unit, which seems absurd. Of course, Williams was only trying to be helpful for the selection of front teeth which he thought would look harmonious when the biological evidence (the tooth) had been thrown away.
Given that a) the patient's real teeth are no longer available, and b) the patient, properly informed of the aesthetic alternatives, has opted for the 'imperfect personal' option rather than the 'anonymous perfect' one, what other pre-extraction evidence is available? It is our contention that a better and often available starting point for tooth selection in edentulous is old photographs.
Evidence-based tooth selection: size and shape
Photographs
Photographs are the most commonly available visual records of natural tooth smiles. Early (nineteenth century) portrait photography required very long exposure times: several minutes were quite usual, much too long to hold a smile. But by the 1940s, with faster emulsions and better lenses, photographing smiles was no longer a technical problem, though in certain cultures it was and remains improper to show one's teeth in a photograph. A 'photometric' method was proposed as early as 1936 to estimate the width of front teeth from smiling photographs.6 A version of this method, using the distance between the subjects' pupils as a reference, was later validated,7 providing both the individual's eyes are also visible in the photo, the face is turned towards the camera and the subject is eight years old or more (Figs 1 and 2). By that age, the cranial base is fully formed and the eyes do not move any further apart.
The above patient (Fig. 1) with new complete dentures made using the photometric method for calculating the size of the upper central incisors, mimicking the tooth positions of the natural dentition. Note the attractive buccal corridors (FS and RG)
Photometric method for selecting front denture teeth
1 Measure the distance between the patient's pupils (PD) by lining up the zero edge of a metal ruler with the right edge of the patient's right iris and then reading off the right edge of the left iris in millimetres (although it is generally called the 'pupil distance', using the edge of the iris where there is a more obvious junction between the white sclera and the coloured iris is easier and more accurate than trying to guess the centre of each pupil). When lining up with the patient's right eye get him/her to look into your left and vice versa. This gets rid of the convergence of the patient's pupils when focusing on a close object. A PD of 65 ± 3 mm is typical.
2 The photograph can be scanned with a scanner or photographed using a digital camera or smartphone. The image is then enlarged on a large screen and a ruler or digital callipers are used to measure:
• The PD on the photograph
• The width of the two upper central incisors on the photograph.
If there is a central diastema or overlapping of these teeth it will be necessary to measure only one central incisor, though this increases the error slightly.
3 Calculate the real width of the original central incisors by subjecting their photographic width to the ratio of the real PD over the photographic PD. Thus: (11 + 21) true width = (11 + 21) photographic width × true PD photographic PD
A typical result would be 17.6 mm. Divide this by a factor of two to give the width of a single central incisor (for example, 8.8 mm). Incidentally, this is a reasonable average width to start with if you have no records at all of the patient's natural teeth.
• Use a mould chart ( Fig. 3 ) to locate central incisors of approximately the correct width (this is printed on the mould chart) and select from among these the one or two moulds most like the shapes, if visible, of the incisors in the photograph(s). With care, it may be possible to choose centrals of one mould, and laterals and canines of others, especially when the manufacturers can supply front teeth in pairs. The width is more important than the length of a front tooth because a) tooth wear and gingival recession may change the visible length, b) many people do not show the full length of their teeth even in photographs, and c) the width establishes the visual mass of the tooth.
When the preferred shades have been agreed with the patient, the teeth can be ordered, preferably to be in the clinic when the record rims are first tried in.
(NB If the lower front teeth seem to have been crowded, the typical arrangement in Caucasians, a wider mould for these may be required than shown on the mould guide as matching the uppers you have chosen.)
It is helpful to ask patients to bring to a first appointment several photographs of themselves showing natural teeth. These can be referred to when discussing the possibility of new dentures. Wedding photos are often the best, being printed larger and professionally in focus, but school photos and even holiday snaps can provide useful information. Asking for photographs at this early stage has several advantages: 1) it may take the patient some time to locate them, either at home or from other members of their family; 2) this may be the first time that the patient has looked for photographs specifically showing their teeth and the hunt, if successful, should raise their awareness of dental appearance issues generally; 3) any 'latent idealism' they may harbour about their own teeth has a chance of being re-educated by this historical evidence. Even with patients who disliked the alignment of their natural teeth and would not want that reproduced, suitable photographs will at least allow the clinician or technician to choose teeth of a size and shape similar to the originals. This personal touch should appeal to all but patients in pursuit of 'the ideal.'
Other records (in the absence of suitable dentate photographs)
Patients may have dentures whose appearance they really liked and wish to have repeated. These teeth can be copied, either via a standard duplication technique or at least by reference to dental stone casts of those dentures. Alternatively, there may be a relative (son, daughter, sister, brother, etc) who the patient thinks has similar teeth (Figs 4 and 5). Casts of those may be made, if impressions are possible and permitted. Or photographs of the relative's teeth may be available if they are unable to attend the clinic. Dental radiographs taken before the front teeth were extracted may give an indication of size and shape. A simple proactive service, which the thoughtful clinician can offer, is to provide the dentate patient with a set of study casts to keep safely as records for the future. This is especially important for wind instrument players, whose embouchure may be critically dependent on the exact re-creation of original tooth positions should the front teeth ever be lost or damaged. But it would benefit anyone needing to replace missing teeth.
In the absence of any evidence whatsoever, upper central incisors with a width around 8.8 mm might be a good starting point, since this is a mean value across several surveys measuring dental casts. A Swiss study of direct measurements of extracted front teeth (14–24), including 44 upper central incisors, reports a mean width of central incisors of 9.1 mm.8 Most manufacturers make the mean width of their upper central incisor moulds considerably less than that. While women's teeth are on average 2 per cent smaller than men's, the variation of tooth size between individuals of either sex is so great that no gender stereotypes will do. Furthermore, it isn't possible to tell whether an unlabelled dental cast is that of a man's or a woman's teeth.9 This fact challenges the 'Dentogenic' concepts of Fisher and Frush (tooth selection by age, sex and personality).10
Choosing the colours (shades) of complete denture teeth
Shade selection is generally claimed by clinicians to be a problem area, with older edentulous patients opting for shades inappropriately light for their age. And it is quite possible that, with the current popularity of natural tooth whitening procedures, there are actually new dental norms shifting towards lighter shades of front teeth, including the natural teeth of older people. These trends are being accommodated by some manufacturers, who offer 'bleach shades' of denture teeth to capitalise on fashions in the United States and other youth-seeking cultures. However, the fact remains that very light teeth displayed in an older face are usually difficult to reconcile as natural. It is the responsibility of the clinician to mention this possibility to any older patients who, with the untrained eye, tend to choose the lightest shades. However, the point should be made as a matter of information, not of obligation. It should always be the right of the patient, having understood that possibility, to over-ride the opinions of the rest of the dental team. The matter might be put in the following way: 'It is absolutely your right to have the very light teeth you have opted for, providing you realise that many people, meeting you for the first time, may well suspect that they are not your own natural teeth. As long as you are still happy with that, that is how we shall go ahead. Can we arrange for a friend or member of your family to come to vet the appearance of the teeth at their final 'dress rehearsal' (try-in), while it is still possible to change the teeth to a different shade, if that is what you decide?'
The supposed preference of older denture wearers for bright teeth may be more myth than fact. In one interesting study entitled 'Tooth shade preferences in older patients,' four sets of complete dentures were made for a 77-year-old woman.11 The same moulds were used in all the dentures, but the shades were varied from very light to fairly dark (Dentsply New Hue 62 to New Hue 81). Colour photographic prints were made of each of the dentures in the mouth, one set showing the whole face and one set showing a close-up view of the lips and teeth. A total of 150 patients at the New York University Dental College were asked to rank the photographs in each set, in order of preference – 50 of the subjects being aged 25–45, 50 being aged 46–65 and 50 being aged 66 or over. It had apparently been expected that the oldest group would show a preference for the lightest teeth. When it was found that in fact they preferred the darkest, the test was repeated with another group of over-65s and another interviewer. This again produced a clear preference for the darkest teeth.
Setting up the teeth
The advantages of chairside setting of anterior denture teeth
Conventionally, after completing the jaw relation records, the clinician hands over the setting up of teeth to the laboratory technician. It should be possible with the following information for a skilled technician to make a very good job of it:
-
1
Prior selection of shades and moulds of denture teeth by patient, dental nurse and clinician working together, plus
-
2
Record rims properly trimmed for face height, lip support and speech, and
-
3
Marked with a centreline, plus
-
4
Dentate photographs when available (or any other pre-extraction records).
However even this approach does not give the patient full opportunity for involvement in the aesthetic management, which, as we have argued, needs to be the patient's prime responsibility. Unless the clinician has the advantage of a technician in the next room or is able to attend the clinic, a better way, we have found, is for the clinician to set up the upper eight front teeth at the chairside with the patient, mirror-in-hand, giving opinions. This is not popular with many clinicians who may consider it a waste of their valuable time and a waste of the patient's money. Or they may feel that their expertise in setting teeth does not begin to compete with the technician's.
But in taking that view, they are depriving themselves and the patient of one of the most exciting and useful periods in complete denture construction, one in which the patient can assume the role of team leader, assisted by the dental nurse if present. In fact, with all but the most assertive patients, the nurse is best cast as the patient's ally and advocate in aesthetic matters, rather than supporting the clinician. To have taken a decisive role in creating the appearance of their dentures is for many patients a revelation. This involvement inevitably brings with it a feeling of connection with the rest of the dental team and a sense of responsibility. This stage is not to be rushed – a two-hour appointment is often needed – and sometimes that is not sufficient. However, two hours seems to be the maximum period people can concentrate on setting up eight upper anterior teeth. After that, one's judgement goes and it is better to book another appointment to continue. Often then what needs to be done is immediately obvious.
It would be a mistake to think that taking time to perfect an appearance-conscious patient's dental appearance will be seen as extravagant. More likely it will be appreciated as taking great care. 'If these people are going to so much trouble just for me, that must mean I am important.'
The front eight teeth
If a remote technician is asked to set up the teeth, it will be better, in our view, to get the patient's opinion first about the set-up of only the upper front eight teeth (Figs 6 and 7). This is because, if front teeth in the initial set-up need to be moved back, many clinicians are inhibited from making the necessary chairside adjustments to a full arch of denture teeth – it takes too much work and time. Moving eight teeth is less intimidating. The first premolars need to be part of this initial arrangement because otherwise the smile looks too 'gappy' at the sides, which many patients find disconcerting. The lower front teeth may also be set up for the first try-in visit, when the patient's principal concern is appearance. The idea is to give the patient sufficient time for considering how the dentures will look, and at least two opportunities on different occasions for this. For many wearers, this is the prime requirement of dentures. Aesthetic failure is as upsetting as aesthetic success is uplifting.
The set-up
The following description refers to both clinic and laboratory locations for set up. The principal disadvantage of the latter is that the technician, even if provided with the necessary information (accurate jaw relation records, correctly carved rims, centre line, dentate photographs, patient approved tooth moulds and shades, etc), does not have the patient's lips or opinions there to assist with setting up the front teeth.
Once the upper rim has been trimmed or added to, to provide proper lip support, and the jaw relationship and vertical dimension of the face has been approved by the patient in front and side views, it is now a three-dimensional template for setting up the teeth. Starting from the scribed midline, a block of wax slightly wider than one of the upper central incisors is cut out with a scalpel blade (thinner and more accurate than a wax knife) using judgement to make the horizontal cut at a level and an angle suitable for receiving the ridge lap of the denture tooth. Using the adjacent rim each side to guide the placement of the tooth, it is sealed in place only at the neck with a hot wax instrument. An electrically-heated waxing instrument maintaining a constant temperature can save a lot of time with set-ups. This procedure – wax block removal and placement of a tooth, one-by-one, is repeated for each tooth round to include the first premolars (Figs 6 and 7). The photographs of the natural teeth are repeatedly referred to in placing each tooth. It is advisable to stop at this point as already explained. If the anterior eight tooth set-up is carried out in the lab, the clinician will be less inhibited in making changes to that small number of teeth. If it is carried out in the clinic, with the patient's approval, the technician will have a much easier job in setting the posterior teeth.
To avoid disputes between clinic and laboratory about tooth position when the teeth are to be set up in the lab, many technicians prefer not to use the record rims which have come from the clinic; they want to keep the unaltered rims as evidence. In this case, it will be necessary to make a new base on which to set the teeth. The dimensions of the original rim may be registered using a silicone putty index attached to the outside of the opposing rim or cast. The teeth can be set up to this reciprocal record (Fig. 8). An alternative to this, which uses the original rim for setting up (Fig. 7) but keeps the evidence, is for the laboratory technician to make photographic records of the articulated rim(s) before and during the tooth set-up, to prove, if necessary, that the information provided by the rims – centre-line, overjet, arch shape, etc – has been respected.
The spatial relationships between front and back teeth in complete dentures
This is the moment for us to make two controversial assertions. First, the positions of the front and back teeth have nothing to do with each other and should be regarded as entirely separate entities.
The front teeth should be put wherever they look good and permit clear speech. The back teeth should be placed so as to 1) give the tongue enough room to function normally, 2) occlude evenly at a good vertical dimension and, if at all possible, 3) permit lateral balanced occlusion over a short distance (say no more than 2 mm each side). This is not to allow normal unilateral chewing ('enter bolus, exit balance') but to assist rapid reseating of a displaced denture in the absence of food.
Second, protrusive balance is not required with complete dentures, provided a horizontal gap of at least than 2 mm is created between the upper and lower front teeth, so that they do not clash during small lateral contact movements of the back teeth. The requirement of this gap clearly does not apply to Class III intercuspal occlusions, with lower incisors edge-to-edge, or even more protruded; but it is important in Class I incisor relations and especially in Class II/div. 2 cases.
Balance in protrusion confers no advantages to the complete denture wearer, with the possible exception of the patient who has totally lost her occlusal bearings and has no 'home position' to return to when reseating the dentures. Balance in protrusion may help reseating in such circumstances. But in all others the insistence on protrusive balance is likely to impose significant aesthetic penalties with no advantages. An obvious instance would be preventing an anterior set-up with a deep incisor overbite, thus leaving the face with an inadequate display of front teeth, upper and lower (Figs 9, 10, 11, 12 show a satisfactory overbite case). Insistence on balance in protrusion must be partly responsible for the unnatural appearance of so many complete dentures.
Similar dentition recreated to restore original dental identity from the photograph of the natural dentition (Fig. 9) (JB and TB)
It is not necessary to wait until the casts have been mounted on the articulator before setting up the eight front upper teeth. This can be done freehand before the records are completed (interocclusal and facebow records, in that order so that the upper cast can remain on the facebow fork until after mounting the upper cast). Gunnar Carlsson has pointed out that a facebow registration is unnecessary for complete dentures.12 We would argue that, providing the clinician has the facebow equipment to hand, it takes so little time to do – say, five minutes at most – and it saves the technician having to choose an arbitrary position for the upper cast, that it is not worth not doing. An additional advantage of using a facebow is that having the articulator condylar hinge axis in approximately the right anatomical position means that minor changes in the vertical dimension can be made on the articulator without much disturbing the occlusion.
Setting the two upper central incisors usually takes the longest time because they need to be correct in so many vectors:
-
Location of the tooth necks with respect to the ridge
-
Amount of tooth on show with the upper lip relaxed
-
Angulation of each tooth long axis in three dimensions
-
Rotation of individual teeth around their long axes
-
Relationship to each other, for example, overlapping or separated (diastema).
Caution needs to be exercised in recruiting the patient's opinion at this early two tooth stage, because any person with only the two front teeth on an occlusal rim tends to look like a cartoon rat. Once the centrals are in positions resembling the dentate photographs, setting up the remaining six teeth becomes much easier.
It is difficult to explain the difference between a well-positioned denture tooth and a poorly positioned one. Suffice it to say that a well-placed tooth looks as if it had erupted there and a badly positioned one looks as if it had been put there. Even the layman can often spot the difference.
Another advantage of including the first premolars in the initial set-up is that it gives the technician, who may be setting the remaining teeth for a full try-in, an idea of the trajectory of the posterior teeth and the buccal corridors. Buccal corridors are not the aesthetic defect that some dental 'makeover' salesmen claim them to be. They can make an important aesthetic contribution to a beautiful smile (Fig. 13), thus avoiding the 'wall-to-wall', 'over-toothed' look.
Once the initial front tooth set-up, including its effect on speech, has been approved by the clinical dental team, patient leading, the case can be transferred to the laboratory, for setting the remaining teeth.
The final 'dress rehearsal', the full try-in of denture teeth and gums, should take place with the attendance – prosthodontic privacy permitting – of the patient's 'nearest and dearest', on the understanding that the dentures will not be finished until there is unanimous consent about the appearance of the face and mouth and smile and speech. It is much easier to achieve what the patient will continue to be happy with when the teeth are still in wax and can be moved, than to have to remake the denture.
Trial denture try-in appointment
The wax try-in stage should be carefully choreographed. Initially the clinician assesses the trial dentures for acceptable fit and occlusion. The patient can then be photographed extra-orally with the trial set up in place. In addition to 'stills', the use of video is helpful: it allows patients to visualise their appearance during social interactions and demonstrates much more than still photographs alone. The photographs and the video of the try-in can be combined with the more familiar use of one or even two hand-mirrors which the patient holds. The dental nurse and the patient's family or close friend (if the patient permits) are recruited to give their opinion (Fig. 21). The patient is invited to be really fussy about the try-in on the grounds that 'it is easy to make changes at this stage but really difficult once the dentures are finished.' The dentate photos are also available for scrutiny. It may help for the clinician to leave the patient alone with the dental nurse for a few minutes; patients are often more forthcoming about their appearance in the absence of the clinician who has supervised it. The teeth are adjusted at this visit or a new try-in appointment is made. The patient can take the try-in home to assess it if they wish, with the necessary instructions about its care. It is important that there is no pressure to accept the denture aesthetically. The denture will be finished only when he or she is completely happy and can think of no further visual improvement.
The patient can then be asked to sign the dental records indicating that they are completely satisfied with the appearance of the denture try-in and that the dentures are ready to be finished. Large aesthetic alterations to the dentures once they have been processed will not be possible and, if requested, will require further visits and consequent professional fees. This possibility may help to focus the patient's mind, making sure they are aware of their responsibility and have fully scrutinised the try-in.
Gum and tooth characterisation
'Not quite perfect is perfect',
Japanese saying.
Variegated pink gumwork
Patients show varying amounts of gingiva during speech, smiling and normal social interactions. Natural gums are not monochrome. For people who show a lot of gum when smiling, the monochrome pink of standard denture gums is noticeably artificial. To escape the attention this could arouse, and maintain prosthodontic privacy, it is necessary to provide gumwork with a natural variegated appearance (Fig. 14). It is useful to have built up a library of photographs of natural dentitions with different gum contours, colouring and recession (Figs 15, 16, 17). These are invaluable in helping fabricate dentures which mimic the architecture of the teeth and supporting gums. A beautiful book of such photographs is also available.13 Most of the dentures shown in this article have variegated gum work produced using Schottlander Enigma Colour Tones, a set of eight heat-curing acrylics based on methyl methacrylate (now replaced by Enigma Gingival Composite).14
The process starts with waxing up, paying particular attention to the anatomical details that will be highlighted in the final denture by the variegated gum colours: root eminencies, gingival recession, papillary recession and areas of greater vascularity are clearly defined at this stage (Figs 18, 19, 20). Stippling is subtly added by softening the wax surface with a pin flame, applying a piece of soft packing foam to it while soft, then lightly re-flaming the surface. As if by magic, natural-looking 'orange peel' gingival stippling appears. Note: a hand-held gas flame can be used with care, but it tends to be too hot; better is the flame from a spirit burner blown sideways to a pin flame, for example, a Hanau alcohol torch (still in production), or a flameless butane pen torch with a narrow nozzle, available from tool and model shops.
Note 1) the stippling and the knife edge margins at the junction between the flanges laterally and the alveolar mucosa; 2) the anterior land of the cast has been cut back to allow easier access of instruments to the wax gumwork. This requires split mounting of the cast so that it can be separated from the articulator mounting plaster during waxing-up (JB)
Denture processing with variegated gum colouring
Internal colouring – the in-flask technique
The waxed-up dentures are flasked with the labial-buccal surfaces using a white stone so that the colours of the gingival acrylics can be clearly seen when applied. The wax is removed by boiling out and, once the cast has cooled, isolating solution is applied to the gingival areas and the different coloured gingival acrylics are sifted in layers, building from the epithelial outside inwards, in order to produce the variegated colouring of natural gums (Fig. 22). Red veining fibres can be added to imitate the nonattached gingivae (Fig. 23).
Photographs of the patients' gums are used to match the gingival acrylic colour range. A small amount of methyl methacrylate monomer delivered by a paintbrush is allowed to seep down the wall of the flask and is absorbed by the powder until no dry powder remains. After application of the gingival acrylics, the denture base material is mixed, packed and processed as normal. If an injection processing system is used, it is important to ensure that the gingival acrylics have been left to bench harden sufficiently prior to processing, so that they will not be displaced by the inflowing base material. Figures 24, 25, 26, 27, 28, 29 show examples of how lifelike coloured gingival acrylics can be.
The partial denture in Fig 27 seated. (FS and RG)
Darker gingival acrylics can be used equally effectively to mimic racial variations in gingival pigmentation (Fig. 29).
External colouring – addition technique for gum characterisation
Typically, this involves light-cured composites coloured specifically to imitate natural gums.15,16,17 Space is made on the labial surface of the denture base either by cutting back the wax before processing the base or by trimming back the processed acrylic. The composite is built up in layers using various gingival colours of composite resin. With skilful application, this can also achieve impressive results (Figs 30 and 31), though the techniques for external application are much more time-consuming than the traditional in-flask acrylic layering method described above (currently reported as between five and ten times as long, e.g. ten minutes per denture with acrylic vs. one to two hours with composite).
The advent of digitally designed dentures, with bases milled out of monochrome pink plastic will accelerate the need for surface-addition skills such as this to achieve artificial gums with anything like realistic appearances. Computer-aided design (CAD) and computer-aided manufacture (CAM) dentures promise improved retention, support and stability owing to improved accuracy of fit of the denture bases.18,19,20This technology in its present form produces CAD CAM (milled or 3D printed) poly methyl-methacrylate denture bases into which the artificial denture teeth are cemented. Alternatively, the teeth may be an integral part of the puck which is milled. The CAD CAM denture bases are prepared from scans of articulated working casts following impression making and jaw registration. At present these methods do not match the aesthetics of hand-made dentures using the techniques described in these articles; the positioning of the denture teeth is not as flexible and the process does not allow internal gum staining. Creating realistic gingival appearance is likely still to require skilful manual additive composite technique such as that shown in Figures 30 and 31.
Other contouring possibilities
It is possible to incorporate rugae and an incisive papilla in the palate of complete dentures (Fig. 32). The presence of an incisive papilla often helps with phonetics, particularly with developing normal 's' and 'sh' sounds. It can modify the jet of air emitted by the median sulcus of the tongue and prevent the whistling 's' anomaly, which can be embarrassing. Better still, the addition of an incisive papilla to a denture which doesn't have one can cure a whistling or over-sharp 's' as if by magic. First this option is rehearsed by adding and modifying a drop of wax to the denture immediately behind the upper central incisors. If phonetically successful, the wax papilla is replaced at the chairside by a small amount of self-curing acrylic.
Bulking of the tongue-palate contact zone and the area of the incisive papilla can sometimes assist proper pronunciation and reduce speech adaptation time,21 though crowding the tongue, through setting teeth too far lingually or having too thick a denture palate, causes more speech problems. The best time to start testing speech is at the record rim stage, providing all superfluous lingual wax has been removed after the lip and cheek support has been finalised and the vertical dimension established. It is much easier to move warmed wax rims (on a rigid base) than to move denture teeth already set in place.
Incorporation of rugae into the palate of complete dentures has been shown to help some people speak clearly.22 These features can be added at the waxing up stage of the denture using the shape and positions of the patients' own incisive papilla and rugae. The simplest way to do this is to mark the crests of the rugae on the cast with a lead pencil, which marks can be seen through the wax sheet covering the palate. Molten wax is added from a waxing instrument along these lines and on the papilla. If the patient doesn't like the feeling, they can be removed before processing, or from the finished denture, at any time later. Ready-made rugae-forming sheets can be incorporated into the dentures, but these are less individual and more trouble to attach. It is important to discuss the provision of these anatomical features before adding them. Elderly long-term denture wearers often prefer the smooth palates and featureless gums they are used to.
Anatomical gums and denture hygiene
Incorporating gingival recession and other anatomical features into gumwork on dentures may make them more difficult to clean, but this is largely a problem caused by incorrect contouring. Where the gingival margins are too thick, the junction between tooth and gum forms a right-angle crevice in which sticky foods lodge and are not easily displaced by tongue, cheeks or lips. This is especially a problem with marked papillary recession in the embrasure areas. With more delicate carving and shallower recesses (Fig. 25), food tends not to stick and to be washed away by saliva. For really lifelike gums it should be possible to floss between the front teeth in the mouth, a pleasant possibility for the self-conscious denture wearer sharing a bedroom or bathroom. But it is fair to say that anatomically contoured gumwork will require more attention to cleaning than standard flat pink gums. This can easily be taught in the clinic after the insertion (delivery) visit with the aid of disclosing solutions (food dyes) applied in a cup at a sink and suitable brushes for cleaning. The 'piece of spinach' stuck to the front tooth will still have to be pointed out as it would with natural teeth. Elderly people sometimes feel that the aesthetic gain of anatomical contouring is not worth the extra trouble in denture hygiene. But they should have the choice.
It may also be objected that it is not worth going to the trouble of making the gums look real when they are shown so little. However, first when the gums contours are refined at the try-in stage most patients say the teeth look better even if they don't know why. And second, it is not just the appearance of the denture in the mouth which is important to the patient. Many patients will examine their new dentures quite carefully in the hand when they get home. The obvious care and quality of the work required to produce good gingival appearance will usually impress such patients. Apart from the increased confidence which they will have in the dental team responsible (a helpful spin-off), the knowledge that what they have in their mouths looks really good, even if part of it doesn't show much, can improve confidence and self-esteem in patients for whom the fact of having dentures does the opposite. A patient summed it up thus: 'I know they're not real but it makes me feel they are that bit more real.' One dress designer provided his fashion show catwalk models with French silk underwear individually monogrammed with their initials. The underwear was not on show but he said it made them walk better.
Occasionally, and in our experience typically with an older long-term denture wearer, there may be a complaint that he or she, having initially liked the look of it, can't get used to the feel of the anatomical gingival contouring, having become used for years to a smooth characterless denture surface. Fortunately, there is a relatively simple solution to this problem. A runny mix of clear self-curing acrylic is flowed over all the surface irregularities, filling up all the depressions, embrasure spaces and gingival crevices. This is processed in warm water in a pressure pot and polished when set. The clear acrylic is virtually invisible, leaving the anatomy and variegated colouring evident as planned, but the denture surface feeling perfectly smooth.
Tooth characterisation
When sighted human beings meet, they automatically scan each other's face, usually first the eyes, followed by the mouth (in denture sufferers it may be the other way around). This scanning mostly takes place subconsciously until something abnormal is detected, at which point consciousness may switch on. Abnormally white, perfectly aligned teeth would be an example of this (except, perhaps in Hollywood).23 A missing natural front tooth would also be eye-catching, and as such would be regarded by most people as a social emergency. The objective, for patients who prefer to keep their wearing of a denture confidential, is to incorporate minor imperfections which switch off the observer's attention. 'Nothing unusual there', the scanning subconscious concludes, before going back on stand-by.
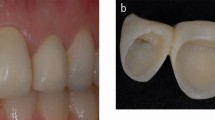
Even with the most lifelike denture teeth available on the market today, such as Schottlander Enigmalife+ teeth, characterisation using composite resin can make a dramatic difference in giving a truly lifelike appearance. Making the denture teeth age-appropriate with fillings, wear, cracks and other naturally occurring flaws can help switch off the observer's attention. One of the most telling deceptions is to leave a small extraction gap in a discrete position, say an upper second premolar, which only shows when the patient smiles. Everybody knows that dentures don't have missing teeth, 'so it can't be a denture, can it?' The patient must guide the rest of the dental team in the matter of how many imperfections will be desired/tolerated. Fortunately, many of the added imperfections can be reversed if the patient does not like them, provided they are carried out before processing the denture. Only the provision of amalgam fillings in posterior teeth is best done on the processed denture. Even then, if the patient changes her mind, they can be made to vanish with composite resin fillings instead.
Front teeth
Wear
If there is one simple thing, taking only a few minutes, which any clinician can do to make front denture teeth look more real, it is to grind their incisal edges. Manufacturers always produce incisors with rounded corners looking as if freshly erupted. Yet the only adults whose natural incisors look like this are people with anterior open bite and those with huge incisor overjets, whose upper and lower incisors can't meet. Everyone else has incisors which show some degree of incisal wear. It is amazing how the removal of even fractions of a millimetre from its incisal edge can often transform a denture tooth from Disneyesque to realistic.
Medium grit sandpaper disks are ideal for this and it is best done incrementally with the set-up in the patient's mouth, under the direction of the patient, holding a hand mirror. It is better to wait until the patient is satisfied with the appearance of the upper teeth before dealing with wear of the lowers, bringing them into edge-to-edge contact during protrusive movements of the lower jaw. This last adjustment is most easily carried out on the articulator, then refined in the mouth.
Denture teeth, once ground down, cannot easily be rebuilt. To avoid this problem, it is possible to fake incisal edge reduction using a black waterproof marking pen (Figs 33, 34, 35, 36, 37, 38, 39).
This was due to saliva leaking past an imperfect lip seal caused by inadequate upper lip support. The front teeth on the existing denture had been set on the ridge instead of in a Class II/div 1 position with a significant 11 mm overjet (see Fig. 5)
Daughter of the patient in Fig. 38. In the absence of good photographic records of her mother's natural dentition, the daughter's face and natural teeth were used as a model for the size and position of her mother's artificial teeth. Their facial resemblance is striking
Cracks
Scoring the resin tooth surface with a scalpel blade produces realistic, natural-looking crack lines in teeth. To produce an unstained crack, a white opaque resin can be rubbed into the crack (Fig. 39). To produce a brown crack, brown composite can be rubbed in (Fig. 38). Incorporating wear into the incisal edge where the crack line terminates mimics natural teeth (Figs 40 and 41). Diastemas and fillings can be incorporated to make the dentures more life-like (Figs 43, 44, 45, 46, 47, 48, 49, 50).
Irregular lower incisors look even more authentic with wear incorporated in the edges. Enamel is removed from the incisal edge in the middle section, a small slot about 2 mm deep is cut with a thin bur (a twist drill from a dentine pin set is ideal) and filled with a light brown stained composite or acrylic resin (Fig. 44).
Back teeth
Surface stains in the tooth fissures/grooves, amalgam fillings, gold inlays or crowns can be incorporated into the dentures to give a lifelike appearance (Figs 45, 46, 47, 48, 49, 50, 51, 52). Amalgam fillings can be placed into occlusal cavities cut into the teeth (Figs 43, 44, 45, 46, 47, 48, 49, 50). Composite is available in dark colours too and can be used instead (Fig. 45). A missing tooth can be incorporated with tipping of adjacent teeth (Fig. 46).
Denture fitting (delivery)
Treatment doesn't finish with fitting the dentures. It is important that the patient is reviewed within one week of fitting them. This rule applies to all patients, including those who feel completely comfortable with the new dentures. They may still require adjustment. We have occasionally seen, under a new denture, a nasty-looking pressure ulcer of which the patient was completely unaware.
The aesthetics of complete dentures change subtly following delivery as they 'bed in' by approximately 0.5 mm into the soft supporting soft tissues. This results in slightly less tooth being visible. Bearing this in mind, it is prudent to err on the side of leaving the denture teeth, back as well as front, slightly over-long at the fitting stage. They can always be shortened later by grinding. In addition, the lip profile may change too, particularly in patients whose previous dentures were grossly plumped out by overly thick flanges. It can take a few weeks of intracellular fluid flow and circumoral muscle readjustment for the lip profiles to assume their stable relaxed natural position.
What happens if the patient doesn't like the new denture appearance?
Even following all of the careful steps described in these papers, the patient (and other members of the clinical team) may come to be dissatisfied with the appearance of the fitted denture. These concerns must be addressed. The alterations may be minor, such as altering the shape of an incisal edge, or thinning a flange if less lip support is desired, or removing some applied surface stains. It may even be necessary to remove and re-set some visible teeth. Occasionally, though, the problems may be too great to rectify by alteration and the simplest way to solve the problem is to re-make the denture. If a remake is necessary, the newly made denture (Mk I) is used as a rehearsal/prototype for a new denture (Mk II). The features that the patient does not like in Mk I will be changed in the Mk II denture.
Jack Turbyfill, following methods taught by Earl Pound,24 advocates routinely making a simpler Mk I rehearsal denture, modifying and learning from this (while using repeated tissue-conditioner linings to heal the mucosa) so as to make a better definitive Mk II. This two-denture approach is inherently expensive and probably appropriate only for patients with sufficient wealth, who have a protracted history of difficulty in coping with dentures. They will possibly have made up most of Messrs Pound and Turbyfill's private clientele.
If a remake is required – the patient or patient's partner, etc, having changed their mind about the appearance of a finished denture – there is the problem of who pays for it. Normally the patient will be called upon to finance this, having been given ample time to consider every aspect of the appearance of the dentures and having indicated (in writing) at the completion of the try-in stages a) that he or she was completely happy with their appearance, including their effect on lip support, face height, etc, and b) understood that, once the dentures were finished, large alterations would require further visits and professional fees. If a remake is required and the fault lies with the clinician, technician, nurse, etc, it is important that no further charge is made to the patient for the necessary additional treatment and lab fees.
Dealing with aesthetic problems
Processed denture different from the try-in
It is distressing if an arrangement of denture teeth, which has taken several hours in the clinic and laboratory to perfect and has been approved only after the most stringent examination, returns from processing with an altered appearance. Damage in transit from the clinic to the lab may be the cause, usually the result of inadequate packing, or else some untraceable and inexplicable laboratory error. There is usually no alternative to resetting the teeth on the existing base or remaking the denture entirely.
One method of protecting the valuable investment of clinical time and energy is to make a plaster key in the clinic of the approved front eight teeth, directly connecting them to the land of the cast, so as to form an accurate matrix of their positions. Even if the set-up is damaged in transit, the teeth can be returned to their exact original positions before processing. Their positions can be checked after processing too. Detail note: when the plaster matrix has set and been received by the technician, after removing it from the cast he or she should grind away from the inside that part which covers the gingival wax. This will allow the matrix to be repositioned on the cast without touching the wax after the wax-up is finished.
In patients with body dysmorphic disorder (BDD), a psychological condition which results in patients seeking treatment for an imagined defect in appearance, their aesthetic objectives can prove to be impossible to satisfy.25 Those whose denture appearance is the cause of their distress are likely to have had multiple dentures made and still remain unhappy. It is outside the scope of this article to discuss the management of suspected BDD but cognitive behaviour therapy (CBT) seems to be currently the best management strategy to treat this condition. Clinicians working in the field of aesthetic dentistry should be aware that some patients presenting for treatment may have body dysmorphic disorder. However, detecting these patients at an early stage is notoriously difficult, as professional defence organisations will confirm. And referring them to a clinical psychologist instead of providing dental treatment requires tact.
Keeping the dentures in optimal aesthetic condition
Patients are taught to clean their dentures twice per day. The dentures should be rinsed to remove food debris and brushed using a medium toothbrush with liquid soap. Denture cleaning creams and regular toothpaste are quite abrasive and may take the polished surface off the teeth and acrylic, resulting in a matt appearance and increased tendency to retain stains. Once the dentures have been brushed, residual bacteria, yeasts, etc, can be removed by soaking them once a day, for 20 minutes, in a solution of alkaline hypochlorite, such as Milton, diluted 1 part Milton to 20 parts cold water. This is particularly needed to protect silicone soft linings from microbial invasion and blister formation. After disinfectant soaking, the dentures can be left in fresh water overnight. However, many patients understandably prefer to keep their dentures in their mouths during sleep for dignity and privacy. In these cases, we respect their wishes and do not insist that they leave them out. Instead we encourage meticulous denture and oral hygiene. At the review visits the denture hygiene and oral hygiene are assessed and further coaching is given if necessary.
As a training exercise, it is helpful for the patient to see plaque on the denture surfaces more clearly. Dark red food colouring, used in cake decoration, can be applied to the denture in a cup, swished around with a little water to coat all the surfaces, then rinsed under running water to remove excess colouring. The dental plaque is suddenly and dramatically visible. The dental nurse or clinician supervises the patient in brushing the stained plaque away and recommends checking with food dye at home from time to time. The patient should be assured that food dyes will not stain the materials of which any dentures are currently constructed. They will only stain the plaque biofilm.
Remaking the dentures in the future
Once the patient has invested time, energy and money in getting a denture appearance of which everyone involved is proud, it seems important to make a permanent record of the shapes of these dentures. Two-part silicone putty moulds of each denture can be made. These three-dimensional silicone records may be stored in the patient's dental laboratory box or given to the patient for safekeeping. The dimensional stability of silicone is impressive and the moulds help in making replacement dentures akin to the originals. (This kind of record may soon come to be superseded by digital scanning and computer controlled milling or 3D printing.) It is important that the patient is instructed to never throw any successful dentures away, even when they have been replaced. There is always much to learn from earlier success. And just as it would be risky for a spectacle wearer to own only one pair of glasses, so it is prudent for a removable denture wearer to have one or more spare dentures, in case of future loss or damage.
Concluding remarks
We hope in these papers to have given a brief report on the condition of people deprived of natural teeth for whom removable dentures are the most practical solution but have not yet proved entirely satisfactory in their appearance or speech. The deficiencies of removable appliances are many, even the best ones. However, there is at least one positive feature of removable dentures: they can be made to look exactly as the patient wishes. No aesthetic dental objective is out of reach, from the most formal whiter-than-white, regular, 'look-at-me' perfection, to the most natural-looking, age-appropriate, irregular, discreet, imperfect appearance – and everything in between. The former dentures are relatively easy to make, requiring little imagination or attention to aesthetic detail because every case looks similar. The latter are more difficult. They require minute attention to detail, skill beyond mere competence, and they consume much more time, at least in the area of their appearance. This is especially the case when one is trying to recreate the individual person's natural dentition. The subtleties and variations of nature, celebrated in the ancient Japanese aesthetic tradition called 'Wabi-sabi',26 are always difficult to reproduce convincingly.* However, for denture-wearing realists, that last stage – regaining their own personal imperfect dental identity – is the most rewarding, comforting, morale-boosting result possible. Comments like 'You've brought me back', 'It's like coming home', 'A deep sense of recognition of a lost self' have come spontaneously to patients' lips, sometimes accompanied by emotional tears of relief and happiness.
Yet we believe that there is a major disconnect between the denture-providing community and the providers of implants. This can be seen in the paucity of 'removable prosthodontist' speakers at the many meetings of societies and academies of aesthetic dentistry around the world, currently preoccupied with the minutiae of dental implants and single tooth dentistry. The committees of these societies seem to consider removable dentures as having nothing to do with dental aesthetics. This is absurd.
As well as highlighting the current 'state-of-the-art' and best practice in connection with the appearance of removable dentures, we feel it is important to emphasise that many of the aesthetic principles described in these papers apply equally well to large scale fixed dental implant restorations. Indeed, it is considered advisable in making full arch implant-stabilised fixed restorations, to carry out a full three-dimensional 'dress rehearsal' with well-made, aesthetically pleasing complete dentures worn for weeks or months. (This has the further advantage that in some cases the patient may be able to settle for very good removable dentures and save the considerable effort and expense of implants, etc)
That being so, it is disappointing to note that removable prosthodontics, particularly with complete dentures, are forming a progressively smaller component of undergraduate dental curricula, to the point of vanishing altogether in some schools. Complete denture prosthodontics is inherently difficult and therefore unpopular – it is usually the first 'whole mouth' branch of dentistry, pit-fall prone, that dental students are faced with – and as the completely edentulous sectors of populations dwindle, at least in more affluent countries, complete denture prosthodontics looks destined to become a postgraduate speciality appealing only to a few. This will mean that most qualified dentists will have received little or no training in how to create plausible and attractive dentitions 'out of thin air', so to speak, when there are no natural teeth left to guide them. This lack of experience will not help younger practitioners placing dental implants in edentulous people. We must hope that, if this trend continues, the training of clinical dental technicians (dental prosthetists, etc) will come to fill this void and keep alive the art of recreating lost dentitions.
In today's climate of Hellenic visual idealism, where affluent populations are exposed daily to images of exaggerated computer-enhanced perfection in various media, and the practitioners of body modification are only too willing to correct nature's so-called 'imperfections' when asked, the skills and commitment necessary to recreate individually authentic dentitions with Wabi-sabi realism are hard to find.
We should like to finish by re-stating that, for us, restoring the lost dental identities of people who have been deprived of teeth is the most joyous, life-enhancing, if sometimes exhausting, and the most spiritually rewarding branch of dentistry.
*It goes without saying that the kind of natural appearances advocated and illustrated in these articles are simply not achievable within the fees for removable dentures indicated within the National Health Service in the UK.
Key to clinicians and technicians involved in these cases:
JB – John Besford (clin)
REB – Ruth Bourke (tech)
TB – Trevor Brooker (CDT)
BF – Birger Fondell (tech)
RG – Rowan Garstang (tech)
FS – Finlay Sutton (clin)
AT – Andrew Taylor (CDT)
CW – Christian Wibberley (CDT)
MW – Matthew Wilde (CDT)
References
Glantz P O . Personal communication to John Besford. 1981.
Ibrahimagić L, Jerolimov V, Ćelebić A . The Choice of Tooth Form for Removable Dentures. Acta Stomat Croat 2001; 35: 237–244.
Kumar M V, Ahila S C, Devi S S . The Science of Anterior Teeth Selection for a Completely Edentulous Patient: A Literature Review. J Ind Pros Soc 2011; 11: 7–13.
Williams J L . A new classification of human tooth forms with special reference to a new system of artificial teeth. Dent Cosmos 1914; 56: 627–628.
McCord J F, Grant A A . Prosthetics: Registration: Stage I — Creating and outlining the form of the upper denture. Br Dent J 2000; 188: 529–536.
Wright W H, Selection and arrangement of artificial teeth for complete prosthetic dentures. J Am Dent Assoc 1936; 23: 2291–2307.
Bindra B, Basker R M, Besford, J N, A study of the use of photographs for denture tooth selection. Int J Prosthodont 2001; 14: 173–177.
Magne P, Gallucci G, Belser U . Anatomic crown width/length ratios of unworn and worn maxillary teeth in white subjects. J Pros Dent 2003; 89: 453–461.
Hyde T P, McCord, J F, Macfarlane T, Smith J . Gender aesthetics in the natural dentition. Eur J Prosthodont Restor Dent 1999; 7: 27–30.
Frush J, Fisher R . Introduction to dentogenic restorations. J Pros Dent 1955; 5: 586–595.
Brisman A H, Paige H H, Hamburg M, Gelb M . Tooth shade preferences in older patients, Gerodontics 1985; 1: 130–133.
Carlsson G . Facts and Fallacies: An Evidence Base for Complete Dentures. Dent Update 2006; 33: 134.
Hajtó J . Anteriores. Fuchstal: Teamwork Media, 2006, Reprint 2015.
Schottlander. Enigma Colour Tones: Part of the Enigma Denture System. A professional guide to custom matching of gingival tissue. 2004. Available at http://www.enigmasystem.co.uk/Enigma_ColourTone_Book.pdf (accessed March 2018).
Schottlander. Enigma Gingival Composite. Available at http://www.schottlander.com/docs/default-source/dfu-pdf%27s/enigma_gingival_composite_0817.pdf?sfvrsn=2 (accessed March 2018).
Anxadent. Anaxgum. Available at http://www.anaxdent.com/194.0.html?&L=1 (accessed March 2018).
Ivoclar Vivadent. SR Nexco Paste. Available at http://www.ivoclarvivadent.co.uk/en-uk/p/laboratory-professionals/sr-nexco-paste (accessed March 2018).
Avadent. Homepage. Available at http://www.avadent.com/ (accessed March 2018).
Ivoclar Vivadent. Wieland Digital Denture. Available at http://www.ivoclarvivadent.co.uk/en/wieland-digital-denture (accessed March 2018).
Dentca. Homepage. Available at https://www.dentca.com/ (accessed March 2018).
Allen L . Improved phonetics in denture construction. J Prosth Dent 1958; 8: 753.
Zaki Mahross H, Baroudi K . Spectrogram Analysis of Complete Dentures with Different Thickness and Palatal Rugae Materials on Speech Production. Int J Dent 2015; 2015: 1–5.
Clive James . I got used to Hollywood, but never got used to the teeth. The Guardian 2016. Available at https://www.theguardian.com/lifeandstyle/2016/mar/19/clive-james-dentist-teeth-white-american-ideal (accessed March 2018).
Pound E . Personalized Denture Procedures. Anaheim: Denar Corporation, 1973.
Scott S E, Newton J T . Body dysmorphic disorder. Dent Update 2011; 38: 112–118.
Juniper A . Wabi Sabi: the Japanese art of impermanence. Tuttle, 2003.
Acknowledgements
Special thanks are due to Rowan Garstang and Matt Wilde and John Wibberley for their technical advice with these three articles.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Besford, J., Sutton, A. Aesthetic possibilities in removable prosthodontics. Part 3: Photometric tooth selection, tooth setting, try-in, fitting, reviewing and trouble-shooting. Br Dent J 224, 491–506 (2018). https://doi.org/10.1038/sj.bdj.2018.222
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2018.222
This article is cited by
-
Improvement of embouchure after correction of irregular front teeth: the case of a professional French horn player
British Dental Journal (2019)
-
Reader panel profile
British Dental Journal (2019)