Key Points
-
Informs regarding the size and breadth of the wheelchair-using population in the UK.
-
Outlines factors to consider when assessing these patients prior to provision of dental care or appropriate referral.
-
Provides guidance to facilitate the treatment of some groups of wheelchair users in general dental practice.
Abstract
The number of wheelchair users in the UK is increasing, and it may be more convenient and appropriate for many of these individuals to receive their dental care in a general dental practice rather than in a community or tertiary facility. This article is intended to provide the average general dental practitioner (GDP) with the basic tools and increased confidence to effectively triage this cohort of the population, and accept them for treatment or refer appropriately.
Similar content being viewed by others
Background context
There are more than 11 million people in the UK living with a limiting long term illness, impairment or disability,1 and 3.3% of UK households have one or more wheelchair users.2 In recent years, there has been much attention and effort given to improving access and equality for wheelchair users: between 2004–2005 and 2014–2015, the percentage of buses with low-floor wheelchair access in England increased from 52% to 95%.3
The proportion of the population who are wheelchair users is already substantial and is likely to increase as the population ages: 44% of those with a limiting illness, impairment or disability are over the state pension age.2
Significant attention has been given to reducing inequalities in society, and more specifically in healthcare, with multiple publications regarding access to healthcare for individuals with physical disabilities. Service providers have a legal obligation under the Equality Act (previously the Disability and Discrimination Act, 1995) to provide equality as regards all elements of care; including access, informed decision-making, communication, and the treatment itself4,5,6. It is important that general dental practitioners (GDPs) are equipped with the necessary information to fulfil their role in minimising inequalities of access for these, and all, patients.
Many GDPs do not regularly treat patients who are wheelchair users, and may be daunted by this prospect. In some cases, a referral to community dental or tertiary specialist services may be indicated, but many other patients can be treated in general practice. This article is intended to provide information to assist with the treatment of patients who have a physical impairment, including but not limited to spinal cord injuries, neurological conditions and ill-health. Some of these patients may have additional needs with regard to, for example, communication. This aspect is beyond the scope of this article, but there is a wealth of information to this effect available in special care dentistry text.
In the UK, individuals can be referred by a health or care professional to their local NHS Wheelchair Centre for assessment and, if deemed appropriate, provision of a self-propelled or electric-powered wheelchair. Those receiving the high rate for 'mobility' under the Disability and Living Allowance (DLA) may also be entitled to further funding for an outdoor electric wheelchair, scooter or car.7
The position and size of the wheels determines the manoeuvrability and portability of a manual chair. Electric-powered chairs are generally bulkier, particularly those designed for outdoor use.8 A document published by the Department for Transport9 found that the average dimensions from a survey of wheelchair users were 1085 × 627 mm. The relevant International Organization of Standardisation standard (ISO 7,176–5:2008)10 gives further information as regards space requirements for doorways, corridors, and corners. It may be a useful tool when planning and designing a dental surgery, or when purchasing any equipment to accommodate wheelchair users.
There are hundreds of wheelchairs on the market with properties to suit a whole range of needs and preferences. The more basic wheelchairs (Fig. 1, left) do not allow much adjustment, but are often more portable, and tend to be used by those who, for example, may be mobile but are unable to walk great distances. Although traditionally bulkier, technological advances mean that powered wheelchairs are becoming more compact (Fig. 1, middle). The features of more advanced chairs that are particularly relevant to the dental setting, are those that can recline or tilt-in-space (Fig. 1, right). The capabilities of an individual patient's wheelchair, and the possible utilisation of this for dental examination and/or treatment, would need to be discussed with patients on an individual basis.
Assessing the patient's needs
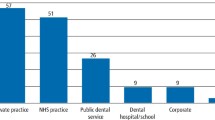
For a successful consultation with a wheelchair user, it is important to avoid making assumptions about the physical and cognitive abilities of the person who uses the wheelchair; speak directly and respectfully to them while remaining mindful of their personal space; and to offer to assist where relevant.11 While these are general tips for anyone interacting with a wheelchair user, for the GDP to lay down the foundations of a clinician-patient relationship and to determine the patients' specific needs, it would be necessary to have a frank discussion with the individual to discover more about their preferences – see Figure 2 for an overview of the options.
As well as discussing a patient's preference with them directly, with their permission, discussion with any relative or carer they might bring to their appointment could also be informative. The relative or carer is likely to be more experienced as regards moving the patient than the average GDP, and be able to advise, or to assist with the use of a transfer board; an inexpensive item of equipment for a general dental practice.
It is also worth contacting the local community or hospital dental services about the equipment they have available. This will help to direct referrals appropriately, as some community services will not have wheelchair tippers. Special care departments in tertiary settings are more likely to have these, such as shown in Figure 3.
It may be relevant to know that patients who are not exempt from NHS charges will still have to pay for their treatment under the UDA system in a community setting. However, this in itself should not be a reason for a referral to a tertiary centre.
Many community and tertiary settings will be able to provide dental treatment under inhalation or intravenous sedation. This may be beneficial to children and adults with certain conditions, notably those causing anxiety, muscle spasms, dystonia or involuntary movements. The GDP should be able to provide patients with a basic overview of these techniques, particularly with regard to the practical considerations such as the need for an adult escort for intravenous sedation with midazolam.
Treatment in general practice
For patients for whom treatment in the general practice setting is most appropriate, there may be additional considerations as well as the wheelchair itself. The GDP should consider the following for all patients, but some aspects may be particularly relevant for wheelchair users. There may be additional requirements for those with any sensory impairments (for example, hearing loops, hazard warning on ramps), but these are beyond the scope of this article. 'Document M' is a piece of legislation which forms part of The Buildings Regulations12 and is concerned with ensuring all people can access buildings and use their facilities.
It is worth highlighting the significant benefit in terms of continuity of care that may come from attending a local dental practice rather than a community or tertiary care facility. This may particularly apply to those individuals who have been long-standing patients of a particular practice, and whose circumstances have changed such that they have become wheelchair users. Familiarity with the team may benefit the patient as well as any relative or carer, as long as physical access is practical. In some cases, care may be shared between a GDP and specialist centre, depending on the procedure.
Physical access
Parking and access to the premises
All members of the dental team, including reception staff, should be able to advise patients and relatives/carers of the arrangements for wheelchair users. This may include the location of any nearby parking spaces for Blue Badge holders.13 If the practice has its own car parking facilities, details of the requirements for a parking space suitable for a wheelchair user are available in Document M:12 4800 × 2,400 mm with a 1200 mm access zone on two sides and a levelled kerb (Fig. 4). This document also gives details of the minimum requirements for a 'level approach', which should be well-lit and signposted, a minimum 1500 mm wide, with passing places, a maximum 1:60 gradient, and feature a firm, durable and slip-resistant surface. At the top of any ramp or incline, there should be a level landing immediately in front of the entrance, clear of any door swings. External doors to new buildings should be 1000 mm wide (775 mm is acceptable for existing buildings). There should be alternative provision for a total rise exceeding 2000 mm. Document M provides more detailed specifications.
Transport
For those patients who do not have their own car and are unable to transfer from their wheelchair into a conventional taxi, it may be useful to have the contact details of a reliable taxi firm with wheelchair-accessible cars.
Doors and hallways
The minimum requirement for widths of internal doors varies dependent on factors such as the angulation of approach, but the range is 750–825 mm. In addition to the width of the door, there should be a space (minimum 300 mm) alongside the leading edge of the door so that a wheelchair user can reach and grip the handle and open the door without the edge of the door coming into contact with the footrest. Corridors should be at least 1200 mm wide, again with passing place.
Reception area
The reception desk should be low enough (or have a portion that is low enough) to accommodate a wheelchair user. The manoeuvring space in front of the desk should be a minimum 2200 × 1400 mm (unless there is a knee recess in which case the requirement is slightly lower). An example is shown in Figure 5.
Facilities
Wheelchair users should be able to access and use unisex WC facilities within the building, again specified by Document M as a minimum 1500 × 2200 mm.
Availability
Timing of appointments
This encompasses both the best time of day for dental appointments, which may relate to patients' medications or carer hours, for example, and the maximum duration of appointments. This may limit the complexity of treatment; patient expectations should be managed appropriately and a referral for sedation for any involved procedures may be considered if this would be beneficial. The timing of appointments should also be agreed with relatives or carers, allowing sufficient time for travel and access to the premises.
Dental facilities, equipment, training and skills
Surgery design
Where additional equipment is present (for example, hoist, tipper), a prior assessment should be made about the practicalities of where within the surgery to install these (if they are to be fixed in position). When considering this, factors such as access to the bracket table, position of the dental light, and X-ray facilities should be taken into account. If necessary, for example if the existing light does not accommodate for the height of the wheelchair when reclined, free-standing dental lights are available. Headlamps serve as a potential alternative to this. This could be proprietary camping lights or, where possible, LED lights intended for clinical use attached to dental loupes – an example of each is shown in Figure 6. The magnification provided by dental loupes as well as the power of these lights may be of benefit to clinician and patient.14 As regards radiography, if a patient is to be treated in the practice they must be able to access a dental X-ray set, as this will provide essential diagnostic information.15 The suction must be able to reach the patient's mouth, and where there is a spittoon in surgery, alternative arrangements such as disposable kidney dishes may need to be considered. In broader terms, the layout of the surgery will determine how easy or difficult it is for a wheelchair user to manoeuvre in the space.
Work within skills, professional competence and practical limitations
A practice should have policies and protocols in place covering all likely eventualities, for example, where a wheelchair tipper is not available, and patients attend who cannot or do not feel comfortable transferring from their wheelchair. The appointment of a responsible person within the practice, perhaps an 'equality lead' may be able to provide advice and training to the other team members. In line with General Dental Council (GDC) standards,16 dental professionals should work within their professional competence to provide quality treatment. Difficult operating conditions may influence the competence and confidence of members of the dental team to complete an item of treatment safely and to a high standard, in which case these guidelines state that a referral to a colleague who is appropriately trained and competent should be made.
Access to the mouth
As mentioned, access to the mouth may be difficult, either for reasons of cognitive impairment, or due to difficulties with muscle control or dystonia. Ensuring that the patient is well-supported with cushions is recommended to assist with the latter, in order to relax the muscles and reduce spasticity.6 As mentioned above, there are countless designs of wheelchair. Many of these do not come with a head rest, but most wheelchair tippers allow for head support. This is an essential part of ensuring safety and comfort when treating patients in wheelchairs. In some cases, the dental nurse may be able to support the patient's head to allow safe access.
Occupational hazards
The Manual Handling Operations Regulations17 counsels that lifting of heavy loads should be avoided wherever possible, and if essential, handling aids or automation, such as the use of hoists or tippers, should be considered. A 'load' may be an object, a person or an animal, and is considered to be 'heavy' if over 25kg (the threshold is lower if lifting above shoulder height, involving twisting movements, and/or for female workers). On this basis, no member of the dental team should be attempting to lift a patient, or otherwise put themselves in a position where they are supporting a patient's weight. There is a significant and well-documented risk of back injury if this advice is not heeded. Putting lifting aside, poor posture in general dentistry poses a significant risk of back pain to members of the dental team.18 'Perfect posture' may be difficult to achieve in less-than-perfect operating conditions, that is, where access to the mouth is difficult as discussed above. Members of the dental team should additionally assess the risks to their own health and take necessary precautions. It is important to avoid prolonged periods straining in positions which confer stress to dentists' and dental nurses' spines. Seated dentistry is generally safer, and is facilitated by the use of wheelchair tippers. Where standing is necessary, the use of a footstool at the appropriate height may avoid some of the strain on clinicians' backs, and bending should be at the knee rather than at the waist. The ideal set-up in ergonomic and efficiency terms is four-handed dentistry according to the 'clock face' working positions.19 This may not always be possible but should be adopted wherever possible to minimise back strain.
Oral health
There may be specific considerations arising from an individual patient's medical history, but in general the likelihood of drug-related xerostomia will also be higher, as many patients with chronic conditions will be taking multiple medications and are therefore at risk of xerostomia. This should be managed to improve patient comfort, and to reduce the risk of caries in line with the Delivering Better Oral Health guidelines.20
Training and education
Members of the dental team may want to expand their knowledge and skill-base as regards special care dentistry. The National Examining Board for Dental Nurses offers a certificate in special care dentistry; and some dental schools provide post-graduate education to dentists in the form of a Diploma or MSc. There is also evidence that experience of special care dentistry by dental students at undergraduate level equips dentists to feel more confident and able to provide dentistry to patients with disabilities in general practice.21 At present, the opportunities for practical training on a less formal or academic basis than the courses mentioned are fairly limited in the UK. There are, however, books which serve as an important and useful resource for the GDP for example, Fiske et al.,22 Scully11 as well as journal articles such as those published by Dougal and Fiske.6 If short courses of practical training were more widely available and GDPs were encouraged to undertake them, perhaps as part of CPD, it would be expected that they would be more likely to feel confident and equipped to manage more patients in practice, thus relieving some of the strain on community and tertiary special care dental services.
Referring to secondary/tertiary care
As has been mentioned, upon arriving at the conclusion that treating a particular patient in practice is outside the GDP's own competencies, an appropriate referral should be made. It is important to establish the patient's specific needs, and reconcile these with the equipment, facilities and services (for example, sedation) available in local specialist services, when deciding where to refer.
Conclusion
The increasing prevalence of wheelchair use within the population means it is more important than ever for the GDP to feel confident in providing appropriate care to these individuals. The focus of this must be on establishing the individual's needs, and proceeding accordingly. This article may provide some areas for consideration in order to do this.
References
Department for Work and Pensions and Office for Disability Issues. Disability Prevalence Estimates 2011–12. 2014. Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/321594/disability-prevalence.pdf (accessed January 2018).
Department for Communities and Local Government). Guide to available disability data. 2015. Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/416475/150323_Guide_to_disability_data___final_web_version.pdf (accessed January 2016).
Department for Transport. Annual Bus Statistics: England 2014/15. 2015. Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/485296/annual-bus-statistics-year-ending-march-2015.pdf (accessed January 2016).
HM Government. Equality Act 2010. 2013. Available at https://www.gov.uk/guidance/equality-act-2010-guidance (accessed September 2017).
Edwards D, Merry A, Pealing R . Disability part 1: the disability discrimination act (1995). — implications for dentists. Br Dent J 2002; 193:199–201.
Dougall A, Fiske J . Access to special care dentistry, part 1: Access. Br Dent J 2008; 204: 605–616.
Age UK. Factsheet 42: Disability equipment and home adaptations. 2015. Available at https://www.ageuk.org.uk/globalassets/age-uk/documents/factsheets/fs42_disability_equipment_and_home_adaptations_fcs.pdf?dtrk=true (acccessed April 2016).
NHS Choices. Choosing mobility equipment, wheelchairs and scooters. 2015. Available at https://www.nhs.uk/conditions/social-care-and-support/mobility-equipment-wheelchairs-scooters/ (accessed April 2016).
Department for Transport. Guidance: Inclusive Mobility. 2015. Available at https://www.gov.uk/government/publications/inclusive-mobility (accessed April 2016).
International Organization for Standardisation. ISO 7176-5:2008 Preview Wheelchairs -- Part 5: Determination of dimensions, mass and manoeuvring space. 2008. Available at https://www.iso.org/standard/46429.html (accessed April 2016).
Scully C . Scully's Medical Problems in Dentistry. London: Elsevier Health Sciences, 2015.
HM Government. Building Regulations: Approved Document M Access to and use of buildings volume 2 – buildings other than dwellings. 2010. Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/441786/BR_PDF_AD_M2_2015.pdf (accessed February 2018).
Department for Transport. Blue badge scheme. 2014. Available at https://www.gov.uk/blue-badge-scheme-information-council (accessed April 2016).
James T, Gilmour A S . Magnifying loupes in modern dental practice: an update. Dent Update 2010; 37: 633–636.
Faculty of General Dental Practitioners. Selection criteria for dental radiography. London: FGDP, 2013.
General Dental Council. Standards for the Dental Team. 2013. Available at https://www.gdc-uk.org/professionals/standards/team (accessed February 2018).
The Health and Safety Executive. The Manual Handling Operations Regulations (SI 1992/2793). 1992.
Breslin M, Cook S . No turning back: posture in dental practice. Vital 2013 10:23–25. https://www.nature.com/vital/journal/v10/n4/full/vital1720.html (accessed March 2018).
Dentistry.co.uk. 'Work smarter, not harder' – Four-handed dentistry. 2007. Available at http://www.dentistry.co.uk/2007/08/23/work-smarter-not-harder-four-handed-dentistry/ (accessed September 2017).
Public Health England. Delivering Better Oral Health: An evidence-based toolkit for prevention. London: Public Health England. Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/605266/Delivering_better_oral_health.pdf (accessed February 2018).
Casamassimo P S . The great educational experiment: has it worked? Spec Care Dentist 1983; 3: 101–107.
Fiske J, Dickinson C, Boyle C, Rafique S, Burke M . Special Care Dentistry. London: Quintessence, 2010.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramirez, L., Dickinson, C. Wheelchair users: a guide for the GDP. Br Dent J 224, 408–412 (2018). https://doi.org/10.1038/sj.bdj.2018.214
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2018.214