Key Points
-
Highlights that sepsis may be seen in dental practice, and is a potentially preventable condition if there is awareness of the warning signs and the need for referral for rapid treatment.
-
Suggests the key message is to stop and think, could this be sepsis in someone who presents with signs or symptoms that indicate possible infection.
-
Proposes that dentists and dental care professionals should think about sepsis, recognise what sepsis might look like, be aware of the pathognomonic warning signs of sepsis, the importance of rapid treatment, be able to advise their patients about sepsis and raise the profile of sepsis.
Abstract
This discussion paper gives an overview of current understanding around sepsis with the aim of raising awareness. NICE requires all healthcare professionals, including dental care professionals to be trained in identifying people who may have sepsis. Enhancing knowledge about sepsis will help the dental team to educate their patients about sepsis, recognise the pathognomonic warning signs and the need for rapid treatment. This paper describes the multiple missed opportunities to diagnose sepsis in a baby and it is hoped the impact of reading this from the mother's perspective will reduce the risk of this happening again.
Similar content being viewed by others
Introduction
There have been some high profile cases of sepsis in the national press over recent years that have been life changing for the people involved. Tom Ray is a quadruple amputee with additional facial amputations from gangrene as a consequence of sepsis. The infection that led to his life-changing situation is thought to have originated after a dental visit while he had a chest infection and when his gingivae were nicked. National initiatives have improved sepsis awareness in the medical, nursing, paramedic and pharmacy professions. NICE guidelines state, 'All healthcare staff involved in assessing people's clinical condition are given appropriate training in identifying people who may have sepsis.'1 The authors wish to use this paper to inform dentists and allied dental care professionals about sepsis: we want dentists to think about sepsis; recognise what sepsis might look like; be aware of the pathognomonic warning signs of sepsis; the importance of rapid treatment; be able to advise their patients about sepsis; and raise the profile of sepsis so that the physical, cognitive and psychological problems and mortality that arise from this potentially preventable condition may be reduced.
What is sepsis?
Terms such as sepsis syndrome, septicaemia and severe sepsis are no longer used and now the overarching term 'sepsis' is used. Sepsis has been defined as 'life-threatening organ dysfunction due to a dysregulated host response to infection.'2 In other words, the body's immune response reacts abnormally to infection by attacking its own tissues and organs, causing organs to eventually fail. It is a life-threatening condition that can be triggered by any infection but most commonly occurs in response to bacterial infection of the pulmonary, urinary or abdominal systems or skin infections. If treated early, outcomes are excellent. However, if treatment is delayed or overlooked, patients can rapidly decline over a matter of hours, with multi-organ failure leading to death. Post-sepsis survival problems are common, for example, cognitive dysfunction, post-traumatic stress disorder, fatigue and physical impairment.
Statistics
The complexity in coding sepsis in hospitals means that the incidence of the actual episodes of sepsis that occur in the UK is difficult to quantify, but it is thought to be between 200,000 and 1.7 million episodes each year.3
The number of deaths from sepsis in the UK is also difficult to quantify due to inadequate reporting, but it is thought there are at least 44,000 deaths from sepsis every year in the UK.3 This is more than all lives lost from breast, bowel and prostate cancer, HIV and road traffic accidents combined. Worldwide this equates to one death every 3.5 seconds from sepsis. In the UK this averages 120 adults and four children daily.
What sepsis looks like and critical warning signs
Clinically sepsis is difficult to diagnose, as there is no 'gold standard' test. People with sepsis look unwell but so do people with flu, a chest infection, pneumonia or gastroenteritis. It can be challenging to differentiate between similarly looking unwell people and someone who has genuine sepsis. It is particularly challenging in pre-verbal children or those with communication difficulties, for example, aphasia, dementia or learning difficulties. Additionally, people with sepsis will have been unwell with an infection leading up to their episode of sepsis, although sepsis can manifest in hours after an extremely short illness of 24 hours. Sepsis is unpredictable and it may be impossible to determine whether a person has tipped into sepsis. People with sepsis often report feeling so unwell that they feel as if they are going to die, but again this is difficult for children and those with communication difficulties who do not have the language to express this.
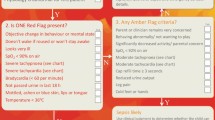
A structured approach is needed to decide when further medical help is needed. NICE have developed some algorithms for the identification of sepsis in the different age groups and the key message is to stop and think, could this be sepsis in someone who presents with signs or symptoms that indicate possible infection.1 There are some crucial pathognomonic warning signs and indicators for sepsis (Box 1). It is crucial to listen to patients and relatives and not to dismiss their concerns about deterioration. Some of these warning signs, known as red flags, require medical tests, but simply asking when was the last time someone passed urine could make the difference between life and death. The Sepsis Trust have some excellent sepsis decision support tools on their website and one for use in primary dental services for adults or children over 12 years is shown in Figure 1.3
If sepsis is suspected then the immediate action is to dial 999, state the patient has 'red flag sepsis', arrange a blue light ambulance transfer to hospital and administer oxygen to maintain saturations above 94%.
Secondary care treatment
Sepsis is treatable and 'the sepsis six' has been shown to be an effective treatment regime in reducing morbidity from sepsis by as much as 50%.4 These are:
-
Administer high-flow oxygen to maintain target oxygen saturations greater than 94% (or 88–92% in people at risk of hypercapnic respiratory failure)
-
Take blood cultures
-
Give intravenous antibiotics
-
Start intravenous fluid resuscitation
-
Check lactate level
-
Monitor hourly urine output.
Antibiotic stewardship has changed our thinking about prescribing antibiotics, but in cases of sepsis, the delivery of broad-spectrum antibiotics within the first hour of confirmed sepsis is crucial in maximising survival.5
What is the relevance of sepsis to DCPs?
The dental literature seldom cites cases of death from sepsis that is odontogenic in origin,6 although there has been a recent letter of concern highlighting the clinical warning signs of sepsis.7 The authors would like readers to consider the following story from one of the authors of this paper. While we acknowledge that the cause of this particular sepsis was not odontogenic, we hope the impact of this will lead dentists and their co-workers to consider sepsis when faced with a person deteriorating with an infection, whether that be a patient or their family, relatives and friends, and to be equipped to recognise the uncertainty around the signs and symptoms of sepsis and so to seek medical help quickly rather than postponing making a decision.
A personal story
William Mead, my one-year old son, died of invasive streptococcal A sepsis on 14 December 2014. An NHS root cause analysis report into William's death conducted by NHSE South found four missed opportunities to save his life had a different course been taken. I'm going to take you through William's journey from my perspective, William's mum, outlining what happened and what went wrong.
William was born on my birthday, the 27 November 2013, and he was born naturally without incident. I took ten months maternity leave and during this time William flourished, developed and continued to hit his physiological milestones.
When William was ten months old he started nursery four days a week when I returned to work in September 2014. He settled in well and really enjoyed his days there. Towards the end of the first month he developed a cold. He was snotty, had a bit of a cough and was generally a little under the weather. When William developed a fever and started to go off his food I took him to his doctor, whereupon he was diagnosed with tonsillitis and prescribed a five-day course of antibiotics. The very next day William started to display pinprick red spots and I promptly took William back to the doctors where they confirmed he was suffering from scarlet fever. As William was already taking antibiotics there was no change in the course of action already being taken. After a couple of days at home William recovered and returned to nursery as normal.
A week passed by and I noticed that William had developed a cough. It seemed to be a self-limiting cough that wasn't causing him any upset. He had no other associated symptoms, but after four days had passed, as his cough hadn't deteriorated or improved, I decided to take William to the doctors to have him checked over in case it was something more sinister than your average cough. The doctor examined William and he was found to be suffering with a viral cough, typical of children who attend mainstream nursery. The advice was to do nothing and to monitor him.
A further couple of weeks passed and the cough hadn't worsened but it was persisting, so I decided to take William to the doctors again as I was concerned that it wasn't subsiding. Once again, William was examined and found to be systemically well and the diagnosis was a viral cough. Our action was to do nothing. Reassured we went home and carried on life as normal. William remained at nursery. Approaching mid-November William begun to occasionally vomit when he was eating, the cough causing him to wretch and he was unable to keep his food down. It didn't upset him and he would carry on eating but nevertheless this caused me concern so we returned to the doctor. On this occasion I requested to see a different doctor so we could seek a second opinion. William was examined by this doctor and found to be suffering with an upper respiratory tract infection, and his chest upon examination was found to be clear. Although crackles were heard these were put down to sounds from the upper respiratory tract. I asked whether William should have antibiotics now as he had been suffering for five to six weeks with this cough. I was told that William didn't need antibiotics as his cough wasn't a bacterial infection. The doctor prescribed William a ventolin inhaler to be taken before eating to help to open his airways and to prevent the vomiting; there is a strong family history of asthma so it was deemed an appropriate course of action to take. We were told that the vomiting was normal for a child of William's age suffering with a cough.
Reassured, once again we went home. After several days William was sent home from nursery as he had vomited there. Due to nursery restrictions for attendance of children with possible gastrointestinal problems we visited the doctor again to have William checked over and to get a letter for the nursery to confirm this wasn't a 'gastro' bug but was due to the cough. William was checked over by the doctor and again the diagnosis was a viral cough. The doctor wrote us a letter for the nursery explaining that a 'gastro' bug had not caused William's sickness and we left.
A week or so later William started to be a little lethargic and less playful. On Friday 12 December he drank his milk at breakfast but pushed his toast around the plate. This was very unusual for him, as he loved his food. He had been teething so we assumed that might be causing him some bother. When we dropped him to nursery we let them know that he was a little 'off' and to give us a ring if there was any concern. Around lunchtime they called to say that William hadn't eaten his morning snack and seemed a little warm so they had taken his temperature and found it to be slightly raised. They gave him some Calpol, and he had a nap. Upon waking him up he hadn't eaten his lunch and was still warm. They took his temperature again and found it to be 38.4°C. Given that his temperature had now increased despite the Calpol and his general wellbeing, they called us immediately to collect him. As soon as we received this phone call, I telephoned the doctors and asked for an emergency appointment with the GP. As this was after lunch we had to 'sit and wait'. Eventually we went in to see the GP, the consultation was around 4.15 pm on a Friday afternoon. This was the same GP that had seen him on all previous attendances (apart from the second opinion we'd sought). William wasn't himself at all, he was really quite upset and out of sorts. The doctor found his temperature to now be 40.1°C. He examined William, his chest, ears, stomach and throat and found them all to be clear. At the time we assumed that he had done a thorough examination of William – being lay people, we didn't know what an appropriate triage was made up of, or what the standard observations were supposed to be. The doctor told us that it was nothing serious, that it was likely a viral infection, with his teeth causing some problems as well. We were advised to maintain Calpol for the temperature, with plenty of fluids and rest. When leaving the appointment, we asked 'when should we take him in', the response to this was 'don't worry it's nothing grisly'.
We took William home and shortly after he went to bed, absolutely exhausted. During the night I had to maintain the Calpol to control his temperature and settle him back to sleep. During the next morning, which was a Saturday, William's temperature started to drop. We assumed this was a good thing as we'd been told to bring the temperature down. However, William didn't seem to be improving, he was deathly pale, and had begun to vomit green bile. In addition, he seemed very cold to touch. He was upset most of the time, whimpering, but very tired and wanting to sleep all the time. We decided to call 111 to seek advice, as we were unsure about what to do.
Calling 111 was very typical; they triaged and asked lots of questions, and we answered them as best we could. We explained that William had had a persistent cough for a number of weeks. We described the visits to the doctors, especially the one the day before, that William's temperature had been 40.1°C and was now 35.4°C, that he was pale, vomiting green bile, he was cold to touch and he wasn't really wetting his nappies. During the phone call William could be heard whimpering in the background. The call handler triaged our phone call and the disposition was found to be a non-urgent three-hour call back from a clinician. We were given basic advice about William's temperature and the call was ended. Satisfied that we were doing the right thing, we waited for the out-of-hours doctor to return our call. William's condition didn't improve and at around 6.15 pm I put him to bed as he was simply exhausted. At around 7.00 pm the doctor called back and we explained the situation. William, by this point, was asleep in bed. I asked 'In your professional opinion what do you think I should do?' The doctor replied that we should leave him in bed, with plenty of rest, fluids and give him Calpol if his temperature rose again, that it was likely a viral infection and would get better without treatment. Reassured we were doing the right thing, we left William to sleep. He had been assessed by his primary GP, we had called 111 and we had spoken to another clinician in one 24-hour period. We were hoping that William would feel much brighter in the morning.
We checked on William throughout the night, he was sleeping fairly soundly, and his temperature hadn't risen. At 5.30 am we checked on him and he had a little water and went back to sleep. I woke shortly after 8 am and looked at the camera monitor and William was sleeping. I got up and went to check on him. William's room had black out blinds and I hadn't put my glasses on so I couldn't see much. I went over to William in the cot and stroked his cheek but he didn't move. I knelt down and put my arms through the bar of the cot and stroked his arm, which was fairly cool, but he didn't stir. I stoked his side and he was stiff. I immediately opened the blinds and I could see that William was dead.
I'm not quite sure when the screaming ended. Perhaps when the paramedics arrived, perhaps when they turned to me and said, 'I'm sorry my love but he's gone', seven minutes after arriving, or perhaps when I had to walk out of hospital without my beloved baby. I don't think the screaming has ever stopped in my head. I didn't know why and I didn't know how, all I knew was that my baby was gone.
As William died at home unexpectedly he had to go away for a post-mortem examination. The results from this can take a number of weeks, but it was very obvious very quickly that something wasn't right. William died on 14 December. After eight days the coroner telephoned me and asked, 'had William had a cough at all?', 'Yes', I replied. The pathologist had found that William had a left collapsed lung, an abscess in his left upper lung lobe, a pleural effusion with over 200 mls of viscous fluid in his left lung cavity, pneumonia in both lungs, heavy inner and outer ear infection and sepsis. 'Sepsis' I replied. 'What's that?' Not only had William been let down in the most devastating way, I didn't know this condition that had ultimately claimed his life.
In the weeks leading to William's death, he in fact had a bacterial chest infection. When the vomiting started this was the early stages of pneumonia. In the last week or so of his life the pleural effusion was developing and in the last couple of days of his life sepsis took over his body. There were 16 failings in William's care and four missed opportunities to save his life. Not only had the doctors misdiagnosed the chest infection and pneumonia, they had failed to spot he was suffering with sepsis. Not only that, they had not informed us or provided us with any safety netting advice about what to look out for should William's condition worsen.
As a family, once the investigations into his death had concluded, we tried to concentrate on raising awareness of a condition that is causing so many avoidable and preventable deaths in the UK. We chose not to focus on individuals but rather change a system that was set up to fail.
I am delighted to be working with key people within the dental industry to ensure that dental staff are aware of sepsis, and to 'think sepsis', especially when treating an infective patient, a pre-infective patient and when prescribing antibiotics.
Conclusion
The key message to remember is to stop and think, could this be sepsis in someone who presents with signs or symptoms that indicate possible infection. Careful questioning and rapid response could make the difference between life and death in a person on the edge of tipping into sepsis.
References
National Institute for Health and Clinical Excellence. Sepsis: recognition, diagnosis and early management. NICE guideline 51. 2016. Available at https://www.nice.org.uk/guidance/ng51 (accessed November 2018).
Shankar-Hari M, Phillips G S, Levy M L et al. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016; 315: 775–787.
The Sepsis Trust. Homepage. 2018. Available at www.sepsistrust.org (accessed November 2018).
Daniels R, Nutbeam T, McNamara G, Galvin C . The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emerg Med J 2011; 28: 507–512.
NIHR Signal. Giving immediate antibiotics reduces deaths from sepsis. 2017. Availble at https://discover.dc.nihr.ac.uk/content/signal-000394/giving-immediate-antibiotics-reduces-deaths-from-sepsis (accessed November 2018).
Carter L, Lowis E . Death from overwhelming odontogenic sepsis: a case report. Br Dent J 2007; 203: 241–242.
Gilway D, Brown S J . Medical emergencies: Sepsis in primary dental care. Br Dent J 2016; 220: 278.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Coelho, C., Mead, M. Sepsis: the applicability to dental care professionals. Br Dent J 225, 1078–1081 (2018). https://doi.org/10.1038/sj.bdj.2018.1039
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2018.1039
This article is cited by
-
An evaluation of sepsis in dentistry
British Dental Journal (2021)
-
An evaluation of sepsis in dentistry
BDJ Team (2021)
-
Knowledge of sepsis risk and management among dental professionals in Wales: a service evaluation
British Dental Journal (2020)
-
Medical emergencies in the dental practice poster: revised and updated
British Dental Journal (2020)
-
Medical emergencies in the dental practice poster: revised and updated
BDJ Team (2020)