Key Points
-
Suggests that after preventive non-operative control of caries, selective caries removal in the minimally invasive operative management of non-cleansable, cavitated carious lesions should now be the norm.
-
Highlights that the justification of such minimally invasive operative interventions is to provide a cavity of adequate proportion to support mechanically the final restoration in more superficial lesions; maintaining pulp health becomes the priority in deeper lesions, with more carious tissue being retained selectively over the pulp.
-
Points out that carious dentine consistency/hardness are still the parameters that should be used clinically to distinguish that tissue requiring removal during minimally invasive operative management.
Abstract
The International Caries Consensus Collaboration (ICCC) presented recommendations on terminology, on carious tissue removal and on managing cavitated carious lesions. It identified 'dental caries' as the name of the disease that dentists should manage, and the importance of controlling the activity of existing cavitated lesions to preserve hard tissues, maintain pulp sensibility and retain functional teeth in the long term. The ICCC recommended the level of hardness (soft, leathery, firm, and hard dentine) as the criterion for determining the clinical consequences of the disease and defined new strategies for carious tissue removal: 1) Selective removal of carious tissue – including selective removal to soft dentine and selective removal to firm dentine; 2) stepwise removal – including stage 1, selective removal to soft dentine, and stage 2, selective removal to firm dentine 6 to 12 months later; and 3) non-selective removal to hard dentine – formerly known as complete caries removal (a traditional approach no longer recommended). Adoption of these terms will facilitate improved understanding and communication among researchers, within dental educators and the wider clinical dentistry community. Controlling the disease in cavitated carious lesions should be attempted using methods which are aimed at biofilm removal or control first. Only when cavitated carious dentine lesions are either non-cleansable or can no longer be sealed, are restorative interventions indicated. Carious tissue is removed purely to create conditions for long-lasting restorations. Bacterially contaminated or demineralised tissues close to the pulp do not need to be removed. The evidence and, therefore these recommendations, supports minimally invasive carious lesion management, delaying entry to, and slowing down, the destructive restorative cycle by preserving tooth tissue, maintaining pulp sensibility and retaining the functional tooth-restoration complex long-term.
Similar content being viewed by others
Introduction
The prevalence of dental caries has decreased in many countries over the last three decades. Despite this significant achievement dental caries, a preventable disease, still remains the most prevalent worldwide, affecting billions of people and generating significant global healthcare costs.1,2 Therefore, how the oral healthcare profession manages dental caries has become the central theme in reducing its burden globally. Strategies to achieve this must be evidence based and/or informed. Recommendations are becoming supported by evidence synthesised from clinical studies.3 However, this is complicated by the use of different terms describing more or less the same management strategies. Researchers and clinicians are not speaking the same professional language. Another complicating factor is the gap between research findings and their implementation into clinical practice. The reasons for this difference are complex but there are a number of likely contributing factors such as inconsistencies in clinical guidelines among professional groups, differences in dental education, which relies often on out-dated concepts, national healthcare policies, and remuneration systems.4 These issues need to be tackled if the oral healthcare profession is to be seen worldwide as a responsibility-taking health promoting organisation.
An initial step in achieving these changes was the establishment of the International Caries Consensus Collaboration (ICCC); 21 international clinical experts in cariology, operative dentistry, biomaterials science, clinical trials, systematic reviews and guideline development from 12 countries met in Belgium in February 2015, to develop expert consensus for recommendations on dental caries related terminology and for dealing with carious tooth tissue removal and managing cavitated carious lesions.5,6,7
Why are such recommendations necessary?
For the oral healthcare practitioner who treats patients on a daily basis, dental caries and its sequelae makes up the bulk of their workload. The traditional management approach has been to remove all carious tissue, in the erroneous belief that this will stop the caries process, and to restore the resulting cavity with a dental restorative material. Over the last 30 years however, better understanding of the caries process and clinical trial evidence on carious tissue removal methods have supported contemporary alternatives to this outdated 'drill and fill' protocol. The clinical circumstances around when to use which method are daunting and somewhat confusing, with information dispersed throughout an ever expansive literature. In addition, the same methods are explained using different terminology in different countries. This paper, therefore, discusses what the alternative terms for the methods mean and when to do what in the operative management of the cavitated carious lesion that has not responded to non-operative prevention regimes in the first instance. This paper deals with teeth with cavitated caries lesions where the pulp is diagnosed as vital (positive sensibility test) or reversibly inflamed.
MI management
What is dental caries?
Dental caries is the disease that results from an ecologic shift in the bacteria within the dental plaque biofilm. An initially balanced population of commensal micro-organisms in a healthy plaque biofilm alters as an increasingly favourable environment for aciduric and acidogenic microflora develops within the stagnating biofilm, following stimulation by frequent consumption of fermentable dietary carbohydrates. The resulting shift in biofilm activity brings about an imbalance in de- and re-mineralisation, leading to net mineral loss within dental hard tissues; the earliest sign and symptom is the carious lesion.8 Dental caries is not an infectious disease, which needs be 'cured' by removing bacteria. Instead, it can be managed behaviourally by controlling its causative factors, that is, the supply of fermentable carbohydrates, and the presence and maturation of the bacterially-populated dental biofilms. If, however, such patient behaviour change is not initiated by the practitioner along with their oral healthcare team, or the responsibility taken by the patient to adhere to such preventive advice, and thus the lesion activity is not controlled, the cariogenic biofilm promotes further lesion progression. If lesion activity continues unchecked, it will lead to pulpal inflammation, pain and dental infection.
Why restore teeth?
Traditional restorative management involves carious tissue removal and reasons for this have historically included to:
-
1
Withstand the packing of restorative materials and to help retain the restoration mechanically (for example, dental amalgam)
-
2
Remove bacteria so stopping the caries process
-
3
Remove demineralised discoloured dentine.
However, thanks to research leading to a better understanding of the caries process and improved evidence from clinical studies, these reasons need updating, clarification and translation into clinical practice:
-
With the development of adhesive bioactive/bio-interactive restorative materials, removal of such large quantities of dental hard tissues is no longer justified
-
Given the adverse effects that a good peripheral seal of the adhesive restorative material to prepared cavity walls have on the viability of remaining bacteria and their cariogenicity, carious tissue removal simply to remove bacteria in order to halt the caries process is neither logical nor justified.9,10,11,12 In a similar fashion, neither is disinfecting the cavity prior to restoring, in order to kill all remaining bacteria
-
Demineralised, but structurally intact dentine that can be remineralised should be preserved.13,14,15 However, clinical discrimination between these layers of infected and affected dentine is difficult.
Carious lesions will arrest if the biofilm is regularly disturbed, 'any lesion at any stage of its progression can arrest'8 (Fig. 1). However, there are circumstances where this is not possible and these are related to patient behavioural factors or where it is desirable to restore lost structure, integrity, form and/or aesthetics. The contemporary aims of operative restorative management have now evolved to:
-
1
Aid biofilm control on a restored, rather than from a cavitated, tooth surface and thereby manage caries activity at this specific location
-
2
Protect the pulp-dentine complex and arrest the lesion activity by sealing the coronal part with an adhesive dental material
-
3
Restore the function, form and aesthetics of the tooth.
The lesion was active (detectable by being rough when a ball ended probe is dragged across the surface) whilst the tooth was erupting and the area was caries prone by being sheltered by the gingivae but is now inactive (smooth when a ball ended probe is dragged across the surface). The patient's oral hygiene habits improved and the area around the gingivae has not undergone demineralisation indicating that during the last stages of eruption the biofilm was removed and cleaning has continued. The lesion shape follows the shape of the gingiva and the white area can be thought of as a scar from previous disease. Note this is an example of an incipient lesion that has not taken up dietary stains to form the arrested 'brown spot lesion'
In conclusion, the only evidence-based reason for selective carious tissue removal is to create a sufficiently large cavity volume and surface area to provide restoration bulk and bond to, whilst maintaining adequate tooth structure to support the restoration, so as to optimise tooth-restoration complex longevity.
What are the guiding principles for removal of carious tissue?
Carious tissues should only be removed when there is no feasible alternative management such as cleaning cavities regularly with brush and fluoride toothpaste, a method particularly suitable in primary teeth. The guiding principles behind that process of removal are to:
-
1
Preserve non-demineralised and remineralisable tissue
-
2
Achieve an adequate peripheral seal by placing the restoration material onto sound dentine and/or enamel where achievable
-
3
Avoid discomfort/pain and dental anxiety. Use methods that have a proven track record of initiating no or low levels of anxiety and pain, such as atraumatic restorative treatment (ART), Hall technique on primary dentition, chemomechanical agents (eg, Carisolv™ gel [Rubicon Lifesciences, Sweden]) etc
-
4
Maintain pulp health by avoiding dentine excavation close to the pulp so minimising the risk of pulp exposure; ie, leave softer affected dentine in close proximity to the pulp if required. Avoiding pulp exposure significantly improves the lifetime prognosis of the tooth and reduces long-term management costs16,17,18
-
5
Maximise longevity of the tooth-restoration complex by removing enough soft dentine to place a durable restoration of sufficient bulk and resilience, whilst maintaining sufficient surrounding tooth support for the restoration.
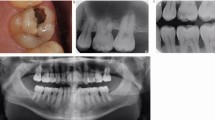
When dealing with permanent teeth with sensible (vital) pulps free from pathologic signs and symptoms, these last two aims, maintaining pulp health and maximising tooth-restoration complex longevity, should be balanced against each other. In deep carious dentine lesions (radiographically involving the inner [pulpal] third or quarter of dentine, or with a clinically assessed risk of pulp exposure), preservation of pulp health should be prioritised (Fig. 2A). In shallow or moderately deep carious lesions (those not reaching the inner third or quarter of the dentine), maintenance of tooth-restoration complex longevity might have more significance (Fig. 2B).
(A) Radiograph of a maxillary left first permanent molar with a deep carious lesion extending to the inner (pulpal) one third of dentine where preservation of pulp health should be prioritised during operative intervention; and (B) a shallow carious lesion in the mandibular left second molar (confined to the inner third of the dentine) where the tooth-restoration complex longevity might have more significance when deciding on the minimally invasive operative management options
How should different carious lesions be managed?
The decision process as to which management strategy to use should follow a rational justifiable pathway (as described here), with the single most important question being, 'When does one need to intervene operatively (invasively)?'
The recommended minimally invasive operative interventions described here are for:
-
Primary and permanent teeth (distinctions are discussed where relevant)
-
Teeth that are pain-free (or presenting with reversible pulpitis only)
-
Teeth with an active carious lesion extending into dentine
-
Where there is no irreversible pulp pathology detected.
Non-cavitated carious lesions
Non-cavitated (that is, cleansable) incipient lesions can be managed non-operatively using biofilm disruption/removal (regular toothbrushing using fluoridated toothpaste)19 coupled with adjunctive topical remineralisation therapies where necessary (targeted at high caries risk individuals), or by therapeutic fissure sealing over the early lesion, predominantly carried out for occlusal pits and fissures (Fig. 3).20
(A) radiograph taken when the child was 5 years old showing initial carious lesions in all four right first primary molars. These were fissure sealed and radiograph (B) was taken 2 years later. There is no clinical or radiographic evidence of progression of any of the lesions. The fissure sealants were repaired as necessary in order to maintain the seal
Non-cavitated but radiographically extensive carious lesion
Occlusal lesions that appear clinically non-cavitated but radiographically extend significantly into dentine might not arrest through biofilm control alone. Such lesions can be therapeutically fissure sealed but the integrity of the sealant must be monitored and consideration given to the possibility of a 'trampoline' effect from the underlying softer infected, completely demineralised dentine leading to mechanical failure of the sealant. If that happens the tooth eventually will also require further invasive restoration. The positive evidence for this kind of treatment is slowly increasing.21,22
Cavitated carious lesions
Cavitated dentine lesions that are accessible to visual-tactile and activity evaluation are potentially cleansable lesions (that is, lesions that are assessed as being cleansable by the motivated patient). These can be made inactive, that is, not requiring further operative treatment, as their progression is unlikely and as such they can be managed non-operatively (non-invasively), via biofilm removal through oral hygiene procedures and fluoridated toothpaste or remineralisation therapies. Lesions that are not cleansable are likely to be pathologically active and progress, but might be made into cleansable lesions ('Non-restorative cavity control'). This type of cavity modification appears applicable for use in primary teeth and was advocated by G. V. Black in 1908. Currently, more evidence is required for guiding the practitioner, particularly related to the age when the non-restorative cavity control can start. This includes additional supporting control measures such as application of fluoride varnish, remineralising agents or placing a layer of high-viscosity glass ionomer over the floor of the cavity. Lesions with surface cavitation that cannot be managed by making them cleansable should be considered non-cleansable and therefore, active. These lesions usually need further operative interventions for their management (Fig. 4).
Clinical presentation of carious dentine
Given the available clinical and microbiological evidence, the level and extent of carious tissue removal can be centred around levels of hardness of the remaining dentine.3,23 These subjective hardness levels include the descriptors soft, leathery, firm and hard. For practical purposes, assessing the force required for a sharp dental explorer to make a mark on carious tooth tissue is currently the most practical way for the clinician to assess its degree of 'softness' or 'hardness'. Some practical guidance is offered below to describe the physical properties that are associated with different histological states of dentine. It should be remembered that these states are only part of a continuous spectrum of presentation of carious dentine and do not exist in discrete zones or layers (Fig. 5).
Soft dentine
Soft dentine deforms when a dental explorer (sharp probe) is pressed onto it, with a latent 'stickiness'. It can be easily scooped up (eg, with a sharp hand excavator) with little force being applied. This dentine consistency is often described as caries-infected dentine and can appear moist in consistency.
Leathery dentine
Leathery dentine does not deform when an instrument is pressed onto it. Without much force, it can still easily lifted – a latent 'tackiness' can be elicited. There may be little differencebetween leathery and firm dentine with leathery being a transition on the spectrum between soft and firm dentine. This dentine consistency is often described as caries-affected dentine.
Firm dentine
Firm dentine is physically resistant to hand excavation requiring some pressure to be exerted through an instrument to lift it.
Hard dentine
A pushing force needs to be used with a dental explorer instrument to engage the dentine and only a sharp cutting edge or a bur will lift it. A scratchy sound or 'cri dentinaire' can be heard when a straight probe is taken across the dentine. This consistency classically signifies sound dentine.
How should carious tissue be removed in teeth with sensible, asymptomatic pulps?
Previous terms for the removal of carious tissues described the outcome of the excavation process and were problematic. The criteria that demarcate the extent to which carious tissues are removed have not been defined or agreed. These might include tissues being free from bacteria, demineralised dentine, discoloured dentine or even 'soft dentine'. Furthermore, there are no commonly used and easily accessible technologies available to reliably assess any of these rather subjective endpoint criteria in a clinical setting. Lastly, if more advanced techniques are available in the future that can, for example, measure bacterial load or mineral loss, it is most likely that areas of dentine will be found where there is incompletely removed carious tissue seen after previously attempted complete removal and vice versa. In other words, when to stop removing carious tissue is arbitrary and dependent upon the operator's understanding of the caries process in the individual tooth and patient that is being treated.
Thus, it seems logical to use procedural definitions to describe exactly what has been done instead of measuring what was attempted to achieve. Using this rationale, the term 'selective removal' is preferred. In selective removal, different excavation criteria are used when assessing the periphery of the cavity as opposed to the area in close proximity to the pulp. The periphery of the cavity should ideally be surrounded by 'sound' enamel to allow the optimal adhesive seal. The peripheral dentine should ideally be hard – with similar tactile characteristics to sound dentine, such as a scratching noise when scraping the surface with a sharp hand excavator or dental probe. However, firm/leathery carious tissue should be left towards the pulpal aspect of the cavity, with only enough of it removed to allow a durable bulk of restoration to be placed, whilst avoiding pulp exposure at all costs. Following this rationale, five main strategies for removing carious dentine, based on the hardness of the dentine are proposed. Decisions regarding the use of these strategies are guided by the lesion depth and activity (Fig. 6).
Decision-making flowchart for the minimally invasive operative management non-cleansable carious lesions in retainable teeth with vital pulps7
Non-selective removal to hard dentine
Non-selective removal to hard dentine (formerly known as complete excavation or complete caries removal) uses the same criterion to assess the endpoint of carious tissue removal for all parts of the cavity, that is, peripherally and pulpally. Only hard sound dentine remains so that demineralised dentine, 'free' of bacteria is 'completely' removed. This unnecessarily aggressive traditional operative approach is considered gross over-treatment and no longer advocated.
Selective removal to firm dentine
Selective removal to firm dentine leaves 'leathery' dentine pulpally; there is a feeling of resistance to a hand excavator whilst the cavity margins and peripheral dentine are left hard (scratchy) after excavation is complete. 'Selective removal to firm dentine' is the treatment of choice for both dentitions, in shallow or moderately deep cavitated dentine lesions (that is, lesions radiographically extending less than the pulpal third or quarter of dentine). In deeper lesions, 'selective removal to firm dentine' puts the pulp at risk of 'physiological stress' or exposure, which is why other strategies should be considered in these cases.
Selective removal to soft dentine
Selective removal to soft dentine is recommended in deep cavitated lesions (that is, extending into pulpal third or quarter of the dentine). Soft carious tissue is left over the pulp to avoid exposure and 'stress' to the pulp, encouraging pulp health, whilst peripheral enamel and dentine are prepared to hard dentine, to allow an adhesive seal to be achieved by placement of a durable restoration. 'Selective removal to soft dentine' reduces the risk of pulp exposure in deep lesions significantly compared with 'non-selective removal to hard dentine' or 'selective removal to firm dentine'.
Stepwise removal
Stepwise removal is carious tissue removal in two stages/visits.12,24,25 Soft carious tissue is left only over the pulp in the first visit and peripheral dentine is prepared to hard dentine, to allow a complete and durable seal of the lesion. A provisional restoration, sufficiently durable to last up to 12 months is placed (eg, high-viscosity glass-ionomer cement). After this time, the restoration is removed and the previously retained carious dentine is further removed until firm dentine is reached, formed during the restoration period as the caries process arrests. There is clinical evidence that the second removal stage may be omitted as this increases risk of pulp exposure.3,26,27 The second visit also adds additional cost, time and potential discomfort to the patient. In the primary dentition, teeth have a limited lifespan so stepwise removal is not considered necessary for primary teeth and 'selective removal to soft dentine' should be carried out.
How should carious tissue removal be carried out?
There are several methods and different technologies for clinical carious tissue removal, including excavation with hand instruments, tungsten carbide/ceramic/carbon-steel/polymer burs, air-abrasion, sono-abrasion, chemo-mechanical agents, and lasers. Studies on clinical advantages and disadvantages of the different excavation methods indicate some evidence finding hand or chemo-mechanical excavation potentially advantageous towards selective removal.28,29,30,31 These technologies may also reduce pain and discomfort during treatment in comparison to the other methods mentioned above,32 although further evidence is required.
Examples of specific caries management protocols
Atraumatic restorative treatment (ART)
ART uses hand instruments for opening small cavities and for removing carious tissue. The cavity is sealed with an adhesive restorative, usually a high-viscosity glass-ionomer cement that simultaneously is used to seal any available remaining pits and fissures. In small and medium dentine cavities, ART follows the 'selective removal to firm dentine' protocol whilst in deep lesions the 'selective removal to soft dentine' is followed.33
Hall Technique
The Hall Technique is a method for sealing carious lesions in primary molar teeth using preformed metal crowns. The correct size of crown is chosen to fit the tooth, filled with glass-ionomer luting cement and seated firmly over the tooth. This avoids the need for tooth tissue removal and local anaesthetic and in two randomised control trials children preferred the technique to conventional restorations34,35 and results indicated that this technique outperformed conventional restorations.36,37 The technique compares favourably with conventional crowns.38 Appropriate lesions and how to carry out the technique are explained at https://en.wikipedia.org/wiki/Hall_Technique.
How should the resulting cavity be managed?
Traditionally, cavity disinfection and cavity lining procedures have been advocated after removing carious tissue, prior to restoring the cavity definitively. Cavity disinfection has been advocated to reduce the number of remaining bacteria. However, given that the presence and number of bacteria are of limited importance in continued caries progression and the development of 'caries associated with restorations and sealants' (CARS, also known as secondary or recurrent caries), the necessity for cavity disinfection is now questionable. Studies have shown no difference in restoration survival rate after disinfecting cavities compared to no cavity disinfection.39 Cavity disinfection procedures do increase treatment time and cost.
Cavity lining (most commonly accomplished with calcium hydroxide or its derivatives) has been used traditionally when treating deep carious lesions in an attempt to keep the pulp-dentine complex viable and functioning through reducing the number of residual viable bacteria, remineralising dentine, inducing reactionary dentine, isolating the pulp and protecting pulp cells from noxious stimuli.40 Again, the antibacterial effects are of limited relevance.41,42 Remineralisation of remaining demineralised dentine seems to be mediated by pulp cell activity and may not be aided by separate liners.43 Although certain liners seem capable of inducing tertiary dentine production and reducing pulpal inflammation,44 the evidence is sparse and the clinical relevance unclear.27,45,46 The isolation of the pulp against thermal insult is relevant when placing thermally conductive restorative materials (ie, dental amalgam). Isolating the pulp when placing resin-based restorations might be beneficial as monomers may penetrate through dentine into the pulp.47,48 In summary, placement of separate cavity lining materials are not necessary to control pathological progression within the sealed lesion, but might help impede monomer penetration and avoidance of fracture of the remaining dentine when resin composite is the restorative material. More clinical evidence is required for the latter.
How should the cavity be restored?
The choice of materials for restoring cavities should be guided by the location and extent of the lesion, the caries risk, lesion activity and specific patient conditions and environment. There is no definitive evidence to support particular materials for restoring teeth after selective carious tissue removal to soft or firm dentine.
What should be done to make these suggested changes work
It takes a long time to change clinical practice in medicine and dentistry. It is acknowledged how difficult it can be to change patients' behaviour/lifestyle and it is no different in trying to change the professions' own attitudes. Contemporary knowledge is necessary for this change to take place but alone, this is not sufficient. Minimally invasive clinical skill sets, for detection, diagnosis and operative techniques need to be mastered as well as nurturing the right attitude for evidence-based change to deliver the best oral healthcare for patients. An important starting point for such change are dental training institutions globally. Cariologists and particularly faculty-based instructors at the skill laboratories and those employed in the clinic should be trained in-house in contemporary cariology and cavity treatments that furnish them with the knowledge to then educate dental students.4
Summary recommendations
-
1
Preventing carious lesions means managing the disease, the caries process, with inputs from both the oral healthcare team and the patient. For existing lesions, dentists, alongside and leading their oral healthcare teams, should work with the patient to manage oral health and as a consequence to control disease activity. In doing so, dental hard tissues are preserved, initiation of the destructive restorative cycle is avoided and the tooth retained in clinical function for as long as possible. Further recommendations for managing non-cavitated lesions are beyond the remit of this paper
-
2
When carious lesions are non-cleansable by the patient and sealing is no longer an option, minimally invasive operative restorative interventions are indicated
-
3
Restorations are placed in cavitated lesions to help the patient in plaque biofilm control, to protect the dentine-pulp complex, and to restore the function, form and aesthetics of the tooth. Carious tissue removal aims to create conditions for a long-lasting tooth-restoration complex, preserving healthy and remineralisable tissue, achieving a sufficient physical seal and maintaining pulp health. It is accomplished preferably with methods that minimise dental anxiety and pain/discomfort for the patient
-
4
In deeper lesions, in teeth with sensible (vital) pulps, preserving pulp health should be prioritised over 'mechanical' restoration success, whilst in shallow or moderately deep lesions, restoration longevity might be considered the more important factor
-
5
For teeth with shallow or moderately deep lesions, 'selective removal to firm dentine' excavation protocols should be followed
-
6
In deep lesions (radiographically extending into pulpal third or quarter of the dentine) in primary and permanent teeth, 'selective removal to soft dentine' should be performed
-
7
In permanent teeth, 'stepwise removal' might also be an option for deep lesions (with the understanding that the second stage visit may not be necessary)
-
8
Hardness of the dentine should be the primary criterion for assessing, describing and reporting on carious tissue and its removal. There is insufficient published evidence to recommend one method for carious tissue removal over another. Variations will always occur due to the different MI operative skill sets practised by dentists the world over
-
9
Cavity disinfection currently has no significant evidence-base for its inclusion in routine operative caries management protocols.
-
10
Recommendations for restoring teeth with particular restorative materials after using different carious tissue excavation protocols cannot be made at present.
Notes
This is a modified manuscript from an original publication: Schwendicke F, Frencken JE, Bjørndal L, Maltz M, Manton DJ, Ricketts D, Van Landuyt K, Banerjee A, Campus G, Doméjean S, Fontana M, Leal S, Lo E, Machiulskiene V, Schulte A, Splieth C, Zandona AF, Innes NP. Managing Carious Lesions: Consensus Recommendations on Carious Tissue Removal. Adv Dent Res; 28(2), pp. 58-67. Copyright © 2016 International & American Associations for Dental Research.
The following are members of the ICCC (International Caries Consensus Collaboration: Falk Schwendicke (Germany), Jo E. Frencken (Netherlands), Nicola Innes (UK), Avijit Banerjee (UK), Lars Bjørndal (Denmark), Wolfgang Buchalla (Germany), Marisa Maltz (Brazil), David J. Manton (Australia), David Ricketts (UK), Kirsten Van Landuyt (UK), Guglielmo Campus (Italy), Sophie Doméjean (France), Margherita Fontana (USA), Soraya Leal (Brazil), Edward Lo (China), Vita Machiulskiene (Lithuania), Andreas Schulte (Germany), Christian Splieth (Germany), Andrea Ferreira Zandona (USA).
Contributors: Falk Schwendicke, Jo E. Frencken, and Nicola Innes conceived the collaboration and organised the consensus meeting. All members of the ICCC attended the meeting, contributed to content, drafted and revised the original manuscripts.5,6
References
Marcenes W, Kassebaum N J, Bernabé E et al. Global burden of oral conditions in 1990–2010: a systematic analysis. J Dent Res 2013; 92: 592–597.
Listl S, Galloway J, Mossey P A, Marcenes W . Global Economic Impact of Dental Diseases. J Dent Res 2015; 94: 1355–1361.
Ricketts D, Lamont T, Innes N P, Kidd E, Clarkson J E . Operative caries management in adults and children. Cochrane Database Syst Rev 2013; 28: CD003808.
Banerjee A . 'MI' opia or 20/20 vision? Br Dent J 2013; 214: 101–105.
Frencken J E, Innes N P, Schwendicke F . Managing Carious Lesions: Why Do We Need Consensus on Terminology and Clinical Recommendations on Carious Tissue Removal? Adv Dent Res 2016; 28: 46–48.
Innes N P, Frencken J E, Bjørndal L et al. Managing Carious Lesions: Consensus Recommendations on Terminology. Adv Dent Res 2016; 28: 49–57.
Schwendicke F, Frencken J E, Bjørndal L et al. Managing Carious Lesions: Consensus Recommendations on Carious Tissue Removal. Adv Dent Res 2016; 28: 58–67.
Fejerskov O, Nyvad B, Kidd E A . Pathology of dental caries. In Fejerskov O, Kidd EAM (editors) Dental caries: The disease and its clinical management. Volume 2. pp 20–48. Oxford, Blackwell Munksgaard, 2008.
Going R E, Loesche W J, Grainger D A, Syed S A . The viability of microorganisms in carious lesions five years after covering with a fissure sealant. J Am Dent Assoc 1978; 97: 455–462.
Banerjee A, Yasseri M, Munson M . A method for the detection and quantification of bacteria in human carious dentine using fluorescent in situ hybridisation. J Dent 2002; 30: 359–363.
Munson M, Banerjee A, Watson T F, Wade W G . Molecular analysis of the microflora associated with dental caries. J Clin Microbiol 2004; 42: 3023–3029.
Paddick J S, Brailsford S R, Kidd E A, Beighton D . Phenotypic and genotypic selection of microbiota surviving under dental restorations. Appl Environ Microbiol 2005; 71: 2467–2472.
Ogawa K, Yamashita Y, Ichijo T, Fusayama T . The ultrastructure and hardness of the transparent layer of human carious dentin. J Dent Res 1983; 62: 7–10.
Kreulen CM, de Soet J J, Weerheijm KL, van Amerongen WE . In vivo cariostatic effect of resin modified glass ionomer cement and amalgam on dentine. Caries Res 1997; 31: 384–389.
Ngo H C, Mount G, Mc Intyre J, Tuisuva J, Von Doussa RJ . Chemical exchange between glass-ionomer restorations and residual carious dentine in permanent molars: An in vivo study. J Dent 2006; 34: 608–613.
Whitworth J M, Myers P M, Smith J, Walls A W, McCabe J F . Endodontic complications after plastic restorations in general practice. Int Endodontic J 2005; 38: 409–416.
Bjørndal L, Reit C, Bruun G et al. Treatment of deep caries lesions in adults: randomized clinical trials comparing stepwise vs. direct complete excavation, and direct pulp capping vs. partial pulpotomy. Eur J Oral Sci 2010; 118: 290–297.
Schwendicke F, Stolpe M, Meyer-Lueckel H, Paris S, Dörfer C E . Cost-effectiveness of oneand two-step incomplete and complete excavations. J Dent Res 2013b; 90: 880–887.
Hilgert L, Leal S, Mulder J, Creugers N, Frencken J . Caries-preventive effect of supervised toothbrushing and sealants. J Dent Res 2015; 94: 1218–1224.
Griffin S O, Oong E, Kohn W et al. The effectiveness of sealants in managing caries lesions. J Dent Res 2008; 87: 169–174.
Fontana M, Platt J A, Eckert G J et al. Monitoring of sound and carious surfaces under sealants over 44 months. J Dent Res 2014; 93: 1070–1075.
Wright J T, Crall J J, Fontana M et al. Evidence-based clinical practice guideline for the use of pitandfissure sealants: A report of the American Dental Association and the American Academy of Pediatric Dentistry. J Am Dent Assoc 2016; 147: 672–682.e12.
Banerjee A, Watson T F . Pickard's Guide to Minimally Invasive Operative Dentistry. 10th edition. Oxford University Press, 2015.
Bjørndal L, Larsen T, Thylstrup A . A clinical and microbiological study of deep carious lesions during stepwise excavation using long treatment intervals. Caries Res 1997; 31: 411–417.
Bjørndal L, Larsen T . Changes in the cultivable flora in deep carious lesions following a stepwise excavation procedure. Caries Res 2000; 34: 502–508.
Maltz M, Garcia R, Jardim JJ et al. Randomized trial of partial vs. Stepwise caries removal: 3year follow-up. J Dent Res 2012; 91: 1026–1031.
Schwendicke F, Meyer-Lückel H, Dorfer C, Paris S . Failure of incompletely excavated teeth – a systematic review. J Dent 2013; 41: 569–580.
Banerjee A, Kidd E A, Watson T F . In-vitro evaluation of five alternative methods of carious dentine excavation. Caries Res 2000; 34: 144–150.
Celiberti P, Francescut P, Lussi A . Performance of four dentine excavation methods in deciduous teeth. Caries Res 2006; 40: 117–123.
Banerjee A . Minimally invasive operative caries management: rationale and techniques. Br Dent J 2013: 214: 107–111.
Schwendicke F, Paris S, Tu Y . Effects of using different criteria and methods for caries removal: A systematic review and network meta-analysis. J Dent 2014; 43: 1–15.
Rafique S, Fiske J, Banerjee A . Clinical trial of an air-abrasion/chemomechanical operative procedure for the restorative treatment of dental patients. Caries Res 2003; 37: 360–364.
Frencken J E, Leal S C, Navarro M F . Twentyfiveyear atraumatic restorative treatment (ART) approach: a comprehensive overview. Clin Oral Investig 2012; 16: 1337–1346.
Innes N P T, Evans D J P, Stirrups D R . The Hall Technique: a randomized controlled clinical trial of a novel method of managing carious primary molars in general dental practice; acceptability of the technique and outcomes at 23 months. BMC Oral Health 2007; 7: 18.
Santamaria R M, Innes N P, Machiulskiene V, Evans D J, Alkilzy M, Splieth C H . Acceptability of different caries management methods for primary molars in a RCT. Int J Paed Dent 2015; 25: 9–17.
Innes N P T, Evans D J P, Stirrups D R . Sealing Caries in Primary Molars; Randomized Control Trial, 5year Results. J Dent Res 2011; 90: 1405–1410.
Santamaria R M, Innes N P T, Machiulskiene V, Evans D J P, Splieth C H . Caries Management Strategies for Primary Molars: 1Yr Randomized Control Trial Results. J Dent Res 2014; 93: 1062–1069.
Ludwig, K H, Fontana M, Vinson L A, Platt J A, Dean J A . The success of stainless steel crowns placed with the Hall Technique. J Am Dent Assoc 2014; 145: 1248–1253.
Farag A, van der Sanden W J, Abdelwahab H, Mulder J, Frencken JE . 5 Year survival of ART restorations with and without cavity disinfection. J Dent 2009; 37: 468–474.
About I, Murray P E, Franquin J C, Remusat M, Smith A J . The effect of cavity restoration variables on odontoblast cell numbers and dental repair. J Dent 2001; 29: 109–117.
do Amaral GS, de Cassia Negrini T, Maltz M, Arthur R A . Restorative materials containing antimicrobial agents: Is there evidence for their antimicrobial and anti-caries effects? – a systematic-review. Aust Dent J 2016; 61: 6–15.
Schwendicke F, Tu Y K, Hsu L Y, Gostemeyer G . Antibacterial effects of cavity lining: A systematic review and network meta-analysis. J Dent 2015; 43: 521–531.
Corralo D J, Maltz M . Clinical and ultrastructural effects of different liners/restorative materials on deep carious dentin: A randomized clinical trial. Caries Res 2013; 47: 243–250.
Fusayama T . The process and results of revolution in dental caries treatment. Int Dent J 1997; 47: 157–166.
Hebling J, Giro E M, Costa C A . Biocompatibility of an adhesive system applied to exposed human dental pulp. J Endod 1999; 25: 676–682.
Dalpian D M, Ardenghi T M, Demarco F F, Garcia-Godoy F, De Araujo F B, Casagrande L . Clinical and radiographic outcomes of partial caries removal restorations performed in primary teeth. Am J Dent 2014; 27: 68–72.
Galler K, Hiller K A, Ettl T, Schmalz G . Selective influence of dentin thickness upon cytotoxicity of dentin contacting materials. J Endodont 2005; 31: 396–399.
Modena K C, Casas-Apayco L C, Atta M T et al. Cytotoxicity and biocompatibility of direct and indirect pulp capping materials. J Appl Oral Sci 2009; 17: 544–554.
Acknowledgements
Grateful thanks to Lisbet Brike and Amy Caldwell-Nichols for administrative support. Prof. Edwina Kidd, for so generously sharing her wisdom and experience and to Prof. W. Buchalla for his contribution to the ICCC meeting and respecting his decision not to support the content of the manuscript through authorship.
We thank the sponsors of the ICCC conference: GC Europe (Leuven, Belgium), DMG (Hamburg, Germany), 3M Oral Care (Seefeld, Germany) and Dentsply DeTrey (Konstanz, Germany). The sponsors had no role in the design or conduct of the conference or the content of the presentations and the two Advances in Dental Research (ADR) manuscripts and were not present during the conference. Thanks also to GC Europe for the use of their premises in Leuven.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Declaration of interest at the organisational and individual consensus conference levels are detailed in the two ADR papers 5,6. None of the participants received honoraria.
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Banerjee, A., Frencken, J., Schwendicke, F. et al. Contemporary operative caries management: consensus recommendations on minimally invasive caries removal. Br Dent J 223, 215–222 (2017). https://doi.org/10.1038/sj.bdj.2017.672
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.672
This article is cited by
-
Knowledge and attitudes toward evidence-based cariology and restorative dentistry among Egyptian dental practitioners: a cross-sectional survey
BMC Oral Health (2023)
-
Minimally invasive selective caries removal: a clinical guide
British Dental Journal (2023)
-
Methodological quality of evidence-based clinical practice guidelines in cariology
Clinical Oral Investigations (2023)
-
In vitro antibacterial activity of green tea–loaded chitosan nanoparticles on caries-related microorganisms and dentin after Er:YAG laser caries removal
Lasers in Medical Science (2023)
-
Color changes and shear bond strength to simulated caries lesions treated with a novel solution of 20% silver nanoclusters in polymethacrylic acid
Scientific Reports (2022)