Key Points
-
Highlights that restoration of the severely worn teeth are challenging.
-
Notes that the long term survival of composites appear to suggest they are successful.
-
Suggests that fractures, chips or bulk loss are common outcomes when using composites for worn teeth.
-
Proposes that patients should be warned of the possibility of fractures before restorations are commenced.
Abstract
Objectives The aim of this audit was to monitor the outcome of composite restorations placed at an increased vertical dimension in patients with severe tooth wear.
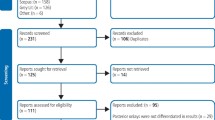
Methods This convenience sample of patients were treated by 11 specialist trainees in prosthodontics, and restored with direct composites. Exclusion criteria included bruxism, poor medical health and a preference for monitoring rather than intervention. The restorations were placed between 2012 and 2016 and were placed over more than one appointment and the outcome monitored for up to 14 months. Failure was assessed at a binary level, either success or failure (minor or major).
Results A total of 35 patients with a mean age of 45 years (range 24–86), 27 of whom were male, received 251 restorations placed from November 2012 to November 2016. The patients had a mean of 11.51 (range 4 to 16) occluding pairs of teeth. There was a total of 40 restoration failures (17%) which was an 83% success rate based on the total number of restorations. For the patient-based data, 14 patients (39%) had no chips or bulk factures while 22 (61%) patients had failures, of which 60% were chips and 40% bulk fractures.
Conclusion Restoration of worn teeth with composites is associated with a high incidence of fractures.
Clinical significance The restoration of worn teeth with composite can involve regular maintenance following fractures and patients need to be aware of this when giving consent.
Similar content being viewed by others
Introduction
Tooth wear is a multifactorial condition where erosion, attrition and abrasion combine to reduce crown height and change the appearance of teeth.1,2 The nature of the condition means that although each may contribute to the wear it is almost impossible, on a case by case basis, to identify which may be the most dominant factor in the progression. Clinical experience suggests that when erosive factors predominate, the outcome for restorations is better than when bruxism is present.
Epidemiology suggests that severe tooth wear affects between 2–10% of each study sample.3,4,5 When extrapolated to the community this implies that severe levels of tooth wear should be common, however, this is not seen clinically. But the restoration of worn teeth remains a clinical challenge and is mainly indicated for those who have severe levels of wear affecting more than one tooth. The most commonly quoted method to restore worn teeth in the UK is using composites.
Previous work suggests that the outcome of composites has good long-term success. One of the first studies to report the outcome from 16 patients restored with a micro-hybrid or a microfilled composite was by Haemmings et al.6 The mean follow up of the study was 30 months and with a success rate reported to be 89.4%. Later, another study by the same team reported the outcome of 283 composites on 26 patients, placed by different clinicians, with a median survival of 5.8 years.7 However, within the data the authors reported 13% of restorations fractured or debonded and of these some patients had repeated fractures and were replaced with conventional crowns. More recently, Milosevic and Burnside reported the outcome of composites placed by one clinician in an eight year study.8 The outcome of 1,010 restorations in 164 patients with a mean age of 51.35 years had an estimated failure rate of 5.4% over a mean follow-up time of 33.8 months and from these data 71 restorations failed in 39 subjects. A recent systematic review of the treatment options for tooth wear reported outcomes for composite resins and conventional ceramic materials.9 From these studies it appears that composites are effective restorations, but for a proportion of patients the restorations fail for a variety of reasons. This study reports the outcome of restorations placed in patients with tooth wear in a hospital setting by specialist trainees.
Methods
Patients were referred to a tertiary care centre for the restoration of worn teeth. The cases were not randomised and were selected for care for reasons related to convenience of travel, ability to attend for multiple visits and because they consented to be treated by specialist trainees. Patients were generally fit and well and able to commute to a dental hospital located in central London. Patients were allocated to a postgraduate dentist who either had qualified in the UK or were from overseas. Exclusion criteria included bruxism being identified as the major component, poor medical health and a preference for monitoring rather than intervention. All patients were treated under the conditions of the NHS in a hospital setting and care was free at the point of delivery. The experience of the operators varied, but all were registered on a three or four year training pathway leading to the MRD exit exam and equivalence of specialist registration at Kings College London Dental Institute. The treatment was supervised by consultants, checking each stage, and the restorations were placed between 2012 and 2016 and were placed over more than one appointment. The audit was registered with the Guy's and St Thomas' Foundation Trust (Audit number 6,504).
Each patient's tooth wear was scored using the BEWE and an attempt was made to identify the major cause of tooth wear using empirical clinical experience and judgement.5 Those lesions with flat incisal surfaces were allocated to attrition while a more rounded and scalloped lesion was more likely to be erosive in nature. Treatment was only offered to those with severe wear and where the severity altered the appearance of the teeth and when patients accepted care. Consent was taken over a number of visits and included verbal explanation of the process and a mock-up placed on teeth using provisional composite materials used for crowns.
All patients had upper and lower impressions, the casts mounted on a semi-adjustable articulator (Denar Mark II; Whip Mix, Louisville, USA) and diagnostic wax ups made at an increased occlusal vertical dimension (OVD). The increase in OVD was estimated from the loss of clinical crown height and the ideal tooth height. Conventional rubber dam was not used but effective isolation was performed using cotton wool rolls or dry dam. Separate etching with 40% phosphoric acid (Henry Shein; Melville, NY, USA) was conducted for 15 to 20 seconds and the dentine-bonding agent (Scotchbond Universal; 3M St Paul, MN, USA) was placed followed by the composite (Duo Ceram; Dentsply UK) build up using an incremental technique following the manufacturer's instructions. At the end of placement even occlusal contacts were assessed using GHM articulating paper and verified with Shimstock (Hanel, Langenau, Germany). An attempt was made to restore the patients in retruded contact position (RCP), but this was not always possible to identify, and in those situations the increase in OVD was determined by tooth shape and the intercuspal position. The review period was arranged by mutual agreement within a few weeks of placement and the outcome of the restorations assessed. Fractures, either minor (chips) or major (bulk fracture), were recorded in the notes and decisions made between the patient and the operator to what was offered.
Results
A total of 35 patients with a mean age of 45 years (range 24–86), 27 of whom were male, received 251 restorations placed between November 2012 and November 2016 (Table 1). The most common diagnosis was a combined aetiology of tooth wear (23 and 66%) followed by nine (26%) with erosion and three (8%) with mainly attrition. Patients had a combined mean BEWE score of 11 (range 6–18) and a mean of seven teeth restored (range 5–21) and the majority were on anterior teeth (23 anterior, one posterior and 11 both). The most common incisal relationship was: class I was 19 (53%), class II div I was one (3%), class II div II was four (11%) and class III was ten (28%). The patients had a mean of 11.51 (range 4-16) occluding pairs of teeth.
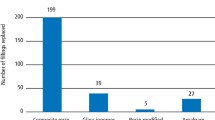
There was a total of 40 restoration failures; 16% based on the total number of restorations. For the patient-based data, 14 patients (36%) had no chips or bulk factures while 22 (63%) patients had failures of which 60% were chips and 40% bulk fractures. From these, nine patients had one (25%), seven had two (19%), three had three (7%) and two had four fractures (10%). These occurred a mean of 4.4 (range 0.5–14) months after restoration placement and all but one involved anterior teeth with the most common being the central incisors and canines. Following the composites, nine (25%) elected to have their teeth crowned with a total of 58 teeth each receiving a mean of six crowns.
Discussion
The management of tooth wear is not simple and involves complex prosthodontics often requiring repeated visits over long periods of time. Composite restorations remain a viable and effective restorative approach but they also involve failures and maintenance. In this study although the analysis by restoration showed 83% success, which is comparable to other studies, 63% of patients had at least one fracture.6,7,8 Based on patient experience this technique has some disadvantages that might impact upon the decision for the patient. Although the cost of care is free in UK dental schools, repairs to teeth in practice are self-funded and can take long appointments, which carry a cost to the patient. Conversely, conventional crowns or partial crowns have lower complication rates, particularly in the period after placement, and therefore remain a treatment option, but they are more expensive and less conservative of tooth tissue.9
The reason for failure was not immediately obvious. This might be related to the relative inexperience of the trainees, although they were qualified dentists and they were enrolled on a training programme. Another reason might be the aetiology of the tooth wear. The most common diagnosis was a combined aetiology suggesting that attrition as well as erosion were related to progression of tooth wear. The impact of a bruxing habit onto brittle composites was not a surprising outcome. While erosion is a smooth surface condition the impact on the survival of restorations is probably not deleterious, whereas bruxism imparts higher occlusal loads onto teeth and restorations and affects their success. However, assessing on an individual basis, the impact of bruxism or erosion is not possible. Clinical experience suggests that bruxism is more likely to lead to failure and this area needs more evaluation.
The analysis of the data at the level of restorations is comparable to other work,7,8 although the period of review for this study was significantly shorter. However, the analysis at the patient level showed a higher experience of failure with 63% experiencing at least one fracture. While composites are repairable and remain a viable option, any treatment decision must consider the impact of cost to patients if repairs are needed. The cost of care for patients with tooth wear is generally high because of the number of teeth involved.
This study reported the outcome from multiple operators and had a relatively short duration. Milosevic and Burnside, reported a 7% failure rate in 39 patients but the restorations were placed by a single operator; this difference presents a dilemma. It is possible that the experience of operators in this study had a negative effect on outcome. There may also have been a difference in the level of tooth wear between the two studies. The operators were all qualified dentists undergoing specialist training and carried out the restorations in a hospital environment. Extrapolating these results to general practice must be approached with caution, but the probability that fractures are a common outcome should be discussed with patients before restorations.
Compared to other studies this is short. For this paper the emphasis was not on the overall success of the restoration but the experience of the patient with fractures. As these fractures occur quite quickly after placement the decision was made to publish rather than wait to emphasise the long-term benefits of the technique.9
The decision to crown teeth that have received failed composites is a balance between the needs of the patient, the availability of tooth tissue and cost of care. As care under the NHS is free at the point of delivery in hospitals, there is a trend to promote composites as a viable and effective form of management. The decision-making process is influenced by cost, as composites are cheaper than crowns, which are produced by laboratories. This study, in part, lends support for this concept but it also raises the awareness that failures, even if they are repairable, occur. For the patient who has to make the decision, which is partly influenced by cost, this will have some influence on the treatment decision. The advantage of composites is that they are simpler to place and can act as a provisional restoration to allow control of the occlusion. The term simpler in this context applies to not using a laboratory technique.
It is not the intention of this paper to reduce the support for restorations involving composites but to raise awareness that they are not without problems and when discussing the options for restorations a discussion about expectations is important to achieve consent. For some patients preservation of tooth tissue is fundamental, but for others a maintenance free option is equally valued. It is for the operator to discuss the options with the patient and then to come to an agreed decision.
References
Bartlett D W . Erosion and tooth surface loss. Int J Prosthodont 2003; 16 Suppl: 87–88.
Smith B G, Knight J K . A comparison of patterns of tooth wear with aetiological factors. Br Dent J 1984; 157: 16–19.
Bartlett D W, Lussi A, West N X et al. Prevalence of tooth wear on buccal and lingual surfaces and possible risk factors in young European adults. J Dent 2013; 41: 1007–1013.
Van't Spijker A, Rodriguez J M, Kreulen C M et al. Prevalence of tooth wear in adults. Int J Prosthodont 2009; 22: 35–42.
Bartlett D, Ganss C, Lussi A . Basic Erosive Wear Examination (BEWE): a new scoring system for scientific and clinical needs. Clin Oral Investig 2008; 12: 65–68.
Haemmings K W, Darbar U R, Vaughan S . Tooth wear treated with direct composite restorations at an increased vertical dimension: Results at 30 months. J Prosthet Dent 2000; 83: 287–93.
Gulamali A, Haemmings K, Tredwin C et al. Survival analysis of composite Dahl restorations provided to manage localised anterior tooth wear (ten year follow-up). Br Dent J 2011; 211: E9.
Milosevic A, Burnside G . The survival of direct composite restorations in the management of severe tooth wear including attrition and erosion: A prospective 8year study. J Dent 2016; 44: 13–95.
Muts E J, van Pelt H, Edelhoff D et al. Tooth wear: a systematic review of treatment options. J Prosthet Dent 2014; 112: 752–759.
Acknowledgements
The authors wish to thank past and present MClin Dent students in Prosthodontics at King's College London Dental Institute.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Bartlett, D., Varma, S. A retrospective audit of the outcome of composites used to restore worn teeth. Br Dent J 223, 33–36 (2017). https://doi.org/10.1038/sj.bdj.2017.583
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.583
This article is cited by
-
The use of the monolithic ceramic and direct monolithic composite in the aesthetic rehabilitation of tooth wear
British Dental Journal (2023)
-
Deterioration of anterior resin composite restorations in moderate to severe tooth wear patients: 3-year results
Clinical Oral Investigations (2022)
-
CAD/CAM techniques for the conservative and efficient management of tooth wear
British Dental Journal (2019)
-
The treatment need and associated cost of erosive tooth wear rehabilitation – a service evaluation within an NHS dental hospital
British Dental Journal (2018)
-
A guide to managing tooth wear: the Radboud philosophy
British Dental Journal (2018)