Key Points
-
Highlights that bisphosphonates continue to be the most common drug implicated in medication-related osteonecrosis of the jaw.
-
Shows that an additional use of bisphosphonates has been indicated and now a further 20,000 women may be prescribed the medication and be exposed to the risk of jaw necrosis.
-
Suggests the burden of additional dental assessment for these patients will fall upon GDPs.
-
Introduces a new communication idea of the dental alert card which provides a warning to dentists for 'at risk' patients.
Abstract
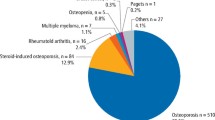
Medication-related osteonecrosis of the jaw (MRONJ) has most commonly been associated with bisphosphonates. The routine uses of these drugs are now well established predominantly in metastatic cancer with bone involvement, multiple myeloma, hypercalcaemia, osteoporosis and Paget's disease. Recently, however, the use of bisphosphonates in early breast cancer has shown a reduction in breast cancer recurrence and breast cancer deaths. This new indication for their use approximates to a further 20,000 women per year in the UK being prescribed bisphosphonates. In this article, we consider the dental impact of this new use of bisphosphonates, report on the rates of MRONJ seen in early breast cancer bisphosphonate trials and discuss strategies aimed at minimising the risk of bisphosphonate-exposed patients developing MRONJ.
Key Points
Summary
Giving bisphosphonates (BPs) to postmenopausal women with intermediate to high risk early breast cancer is beneficial in reducing breast cancer recurrence and mortality
In the UK, approximately 20,000 women a year may benefit from adjuvant BPs as part of their early breast cancer treatment
Oral clodronate and i.v. zoledronic acid appear to be equally effective in reducing breast cancer recurrence and mortality in the adjuvant setting
In early breast cancer studies, oral clodronate was associated with a lower risk of MRONJ IV than zoledronic acid
In the adjuvant setting, the risk of MRONJ from BPs is small relative to the larger risk of breast cancer recurrence and mortality
All patients offered adjuvant BPs (oral or IV) should be informed of the associated risk of MRONJ
Patients treated with adjuvant BP should undergo the same pre-BP dental assessment and MRONJ preventative measures (eg regular dental checks, avoiding extractions) as patients treated with BPs in other settings
The risk of MRONJ may continue long after completion of adjuvant BP treatment due to the long half-life of BPs in bone (estimated >ten years) and so dental precautions should be continued (especially after zoledronic acid)
As MRONJ risk increases with duration of BP exposure, adjuvant treatment should be stopped once the period of known benefit is complete (3–5 years)
Dental health professionals should be aware of this new use of BPs when obtaining patient drug histories
A patient-held Dental Alert Card may help dental health professionals identify patients at risk of MRONJ
Similar content being viewed by others
Introduction
Medication-related osteonecrosis of the jaw is now a well-recognised, rare but serious complication predominantly associated with bisphosphonates such as alendronate and zoledronic acid.1 Additional drugs, most commonly used in cancer patients, have been implicated (Table 1) and it appears the list will continue to grow.2 For many years, the clinical indications for bisphosphonate treatment have remained unchanged. Within oncology, bisphosphonates have been used in the palliative setting to treat patients with advanced stage disease, often in conjunction with other therapies such as chemotherapy. Since bisphosphonates were first approved (Table 2) by the Food and Drug Administration, more than 20 years ago, several randomised phase 3 clinical trials have demonstrated their efficacy in reducing complications from skeletal metastases (for example, pathological fracture, spinal cord compression, pain requiring radiotherapy) across many types of cancer including breast, lung, prostate and multiple myeloma.3,4 Reducing complications from skeletal metastases or delaying their onset is important in maintaining a good quality of life for cancer patients as these events are frequently associated with hospitalisation, loss of independent mobility and pain.5
Bisphosphonates in the curative breast cancer setting
A new development in the management of early stage breast cancer has recently led to the call for bisphosphonates to be brought into the curative setting. In 2015, a meta-analysis of 27 randomised trials in early breast cancer showed that adjuvant bisphosphonates given to postmenopausal women reduced the development of secondary breast cancer and improved survival.6 Though it has been shown that adjuvant bisphosphonates reduce breast cancer deaths in this subgroup from 18% to 14.7% at ten years, regulatory approval for this indication does not yet exist and so a European consensus panel has produced interim guidance for prescribing. Postmenopausal women (or those with ovaries pharmacologically suppressed) at intermediate to high risk of breast cancer recurrence are recommended to receive a regimen of either oral clodronate (1600 mg daily) or intravenous (IV) zoledronic acid (4 mg six monthly) for a period of three to five years.7 It has been estimated that in the UK, around two-thirds of postmenopausal women with breast cancer are at sufficient risk of breast cancer recurrence to benefit from adjuvant bisphosphonate therapy equating to approximately 20,000 women a year.8
Risk of MRONJ in the adjuvant breast cancer setting
The frequency of MRONJ from oral bisphosphonates in the early breast cancer setting is 0.06 to 0.7% of the bisphosphonate-exposed patient population (Table 3), a higher frequency to that documented in the osteoporosis population (for example, 0.004%).15,16 A major difference between the two populations (early breast cancer and osteoporosis) is that immediately before commencing bisphosphonates, most of the early breast cancer group will have been exposed to an intensive course of systemic chemotherapy typically lasting four to six months. A recognised risk factor for developing MRONJ when given concomitantly with bisphosphonates, we do not yet know whether systemic chemotherapy administered just before bisphosphonates increases the risk of MRONJ.17
The potential for MRONJ in early breast cancer studies notably increases when intravenous zoledronic acid is used with reported frequencies of up to 1.5% of patients exposed to zoledronic acid (Table 4). Similar to the MRONJ risk from bisphosphonate use in metastatic cancer and osteoporosis, the risk with adjuvant zoledronic acid appears to increase with both treatment duration (three years versus five years) and dose intensity (cumulative doses of 28 to 76 mg) (Table 4).1 It is interesting to note that when zoledronic acid was given for only three years with a low cumulative dose of 28 mg (4 mg every six months), there were no reported cases of MRONJ.12 However, the study by Gnant, et al. was relatively small for an MRONJ study with only 900 patients exposed to zoledronic acid and larger studies are needed to accurately assess the true risk of developing MRONJ. Small study size is an ongoing challenge that affects the assessment of true MRONJ disease frequency, especially in the use of oral bisphosphonates where the risks of developing MRONJ are smaller than for IV bisphosphonates.1
Risk factors for developing MRONJ continue to be studied and there is strong evidence that dentoalveolar surgery, denture use, pre-existing inflammatory dental disease (for example, periodontal disease, peri-apical pathology), concomitant systemic chemotherapy, corticosteroid therapy and anti-angiogenic drugs increase the risk of MRONJ.17 However, as we do not yet understand the pathophysiology of MRONJ and still debate the potential mechanisms involved, we are unable to provide individualised MRONJ risk estimates to patients about to embark on bisphosphonate therapy.1
The risk of MRONJ for postmenopausal women with early breast cancer treated with either oral bisphosphonate (≤0.7%) or IV zoledronic acid (≤1.5%) is small when compared with the much larger risk of breast cancer mortality (18% at ten years).6 However, as breast cancer is the commonest cancer in the UK with more than 55,000 new cases a year, the group of patients at risk of MRONJ could grow by 20,000 each year as eligible patients are started on adjuvant bisphosphonates.8,18 Moreover, as this use of bisphosphonates is in the early breast cancer setting, as part of curative breast cancer treatment, many women will be cured of their cancer and have many decades of 'normal life' to live beyond their cancer treatment. This is in contrast to the use of bisphosphonates in the metastatic cancer setting where life expectancy can be significantly limited for many patients, being measured in months or in some cases a few years.5 In recent years, there have been a number of reports of successful resolution of MRONJ, of all stages, following both surgical and non-surgical interventions.1 While these reports provide welcome hope, we are presently far from being able to promise a certain cure to patients newly diagnosed with MRONJ. With unresolved MRONJ, patients suffer long term morbidity as they live with a chronic disease and experience the associated negative impact on their quality of life. In the current financial climate of the NHS, we cannot ignore the economic impact of managing patients with MRONJ although very little work has been published in this area. A recent analysis of patients with osteoradionecrosis from our institution estimated the total cost of surgical resection (with or without mandibular reconstruction) to be approximately £30,000 per patient.19
It is said that, 'prevention is better than cure' and this is no more true than in the case of MRONJ. We now have some evidence that optimising oral health before commencement of bisphosphonates reduces the risk of MRONJ.20,21 If a dental extraction becomes unavoidable in a patient at risk of MRONJ, prophylactic antibiotics, although not providing complete protection, may reduce the chance of a MRONJ lesion developing.22 As oncologists and dental health professionals, we need to help the 20,000 women each year with early breast cancer who may be embarking on adjuvant bisphosphonate therapy to minimise their MRONJ risk. The first step is to ensure that all the relevant parties are aware of the patient's MRONJ risk.
Highlighting those at risk of MRONJ
Identifying patients on oral bisphosphonates is often straightforward through their active prescription. However, recognising patients receiving intravenous therapy that has been implicated in MRONJ is more difficult as it does not appear on repeat prescription forms. Moreover, as the administration interval of MRONJ associated drugs can be long (for example, every six months), the patient may inadvertently omit the drug from their current drug history. It remains even more difficult to identify historic intravenous bisphosphonate use. As dentists we often ask 'what medicines are you currently taking?' and it is uncommon to ask 'what medication have you been on?' However, in patients who have previously received bisphosphonates, this remains vitally important as even after the medication has been stopped, due to its extremely long half-life in bone (ten years), patients retain a MRONJ risk for many years and even decades. The dentist must be careful in their medical history taking and remain alert for patients who have conditions such as, cancer, osteoporosis and hyperparathyroidism, knowing that it is very likely that they would have received bisphosphonates and are hence, at risk of MRONJ.
The early breast cancer group of bisphosphonate-exposed patients poses a huge challenge to general dental practitioners (GDPs) as their risk of MRONJ continues long after they have been given the 'all clear' from their breast cancer and discharged from the oncology clinic. However, GDPs are key players in helping patients minimise the risk of developing MRONJ, as they can encourage good oral health, avoid invasive dental procedures and refer patients to secondary care for specialist dental management. Oncologists and dental specialties involved in commencing bisphosphonate therapy in hospital need to help patients communicate their risk of MRONJ to their GDPs (both current and future) so that together, they can be proactive in reducing the risk of MRONJ.
In the dental hospital, across all sub-specialties, we have seen an increase in referral for patients in both our MRONJ pre-assessment clinic as well as our jaw necrosis clinic. Our initial attempt of contacting the drug companies to establish a central database to log the patients on known MRONJ drugs to allow for surveillance was poorly received requiring the need for a different approach. Highlighting certain drugs to medical professionals caring for patients is not a new concept and has been successful through past intervention such as:
-
Steroid card
-
Warfarin anticoagulation (Yellow) book
-
Non-vitamin-K oral anticoagulants alert card (dabigatran, rivaroxaban, apixaban).
Based on this concept we formulated the Dental Alert Card (Fig. 1). This small credit card sized card is provided to all patients at the start of their MRONJ associated drug therapy. The card can easily fit in a wallet or purse and patients are advised to show their dentist the card when having any dental assessment or treatment. This process means that no longer does the patient need to remember historic medications they may have been on while still being able to communicate to a dentist they have an underlying risk of MRONJ. Furthermore, if they change dentist or practice the information is still successfully transferred. The front of the card has the name of their oncology consultant while on the reverse the card provides the dentist relevant information and a referral pathway link when they feel it is appropriate to refer.
Left – The front of the Dental Alert Card, Right – The back of the Dental Alert Card. Following completion of dental assessment the card is completed with the patient's details, laminated and given to the patient to keep and show to a dental professional prior to dental treatment. The card is the same size as a credit card and can fit into a wallet or purse
The Dental Alert Card may find its use in a number of different situations (see case studies). The Dental Alert Card helps the patient in their responsibility of informing dental health professionals of their risk of MRONJ and alerting them to the possible impact this may have on any dental treatment they may provide. Dental health professionals will still need to assess each patient and situation on an individual basis and discuss the risks and benefits of treatment with the patient. The current Dental Alert Card is in its early phase and we aim to contact the first cohort of patients after a year to gain feedback and further evolve the process. The use of the Dental Alert Card has now been extended to our large head and neck radiotherapy cohort.
Case studies
Case study 1
A 60-year-old musician who completed three years of oral clodronate for early breast cancer a year ago develops toothache and is seen by her GDP who decides that a dental extraction is indicated. On viewing the patient's Dental Alert Card, the GDP refers the patient to the necrosis clinic for advice. Following patient assessment the hospital practitioner provides the GDP with information and reassurance that the risk of jaw necrosis is very low and that with the appropriate informed consent, an extraction can be provided in primary care.
Case study 2
A 40-year-old journalist receiving six monthly intravenous zoledronic acid as part of her early breast cancer treatment sees her GDP for her routine, six-monthly, check-up and is found to have developed an asymptomatic area of MRONJ. Using the referral information on the Dental Alert Card, the patient is promptly referred to the necrosis clinic where the diagnosis is confirmed and management initiated.
Case study 3
A 58-year-old solicitor who completed three years of zoledronic acid treatment for early breast cancer five years ago is referred to a specialist orthodontist whose ideal treatment plan involves extractions. However, having seen the patient's Dental Alert Card and been made aware of the patient's MRONJ risk, a safer, non-extraction treatment plan is recommended with the patient accepting that the orthodontic outcome may be less ideal as a consequence.
Modifying dental treatment goals for patients at risk of MRONJ
MRONJ lesions can be limited and asymptomatic but they can progress to a more advanced stage and in its severest form, MRONJ is a devastating condition. Patients diagnosed with MRONJ commonly experience cyclic or constant symptoms such as pain, swelling and infection. These symptoms can lead to functional difficulties with eating, drinking, swallowing and talking that then impact on a patient's quality of life. A further consequence of a diagnosis of MRONJ is the possible delay or even complete cessation of bisphosphonate therapy in order to optimally manage this complication and this can cause additional negative health effects.
Although MRONJ can occur spontaneously, the majority of reported cases have been associated with triggering factors, the commonest being dental extraction, but also denture trauma, dental implants, as well as dental pathology such as infections or periodontal disease. With no guaranteed cure, prevention continues to be the mainstay approach in MRONJ.
The conventional treatment goal for any patient who presents with a dental problem is to render them free of dental disease and to maintain optimum oral hygiene. However, similar to the historic approach for patients at risk of osteoradionecrosis, treatment goals need to be adjusted when approaching a dental problem in a patient at risk of MRONJ.23 Symptom control and minimisation of the risk of MRONJ are paramount and this may result in a necessary compromise in aesthetics and function, a point highlighted in the 2010 American Association of Endodontics position statement.23 In practice, all dentists experience cases where compromised treatment has been delivered due to the wider clinical context and a necessary departure made from the ideal treatment plan. In such cases, through the process of informed consent, the various challenges of the dental treatment are explained to the patient with a discussion of the risks and benefits, with a warning that ongoing, unresolved symptoms may require a more definitive solution in the future.
Examples of alternative solutions that avoid or reduce bony manipulation in patients 'at risk' of MRONJ
Selective extractions approach
The selective extraction approach has been commonly used in clinical settings such as head and neck radiotherapy patients at risk of osteoradionecrosis, severely unwell palliative care patients and patients suffering from dementia. Since the recognition of MRONJ, this approach has also been implemented in those at risk of this condition. The aim is to prioritise management of the most symptomatic tooth while delaying management of less symptomatic teeth with acceptance of the associated risks that this approach may incur.
In the situation where multiple extractions are required across multiple quadrants, the selective extraction approach can be extended to a quadrant-based extraction approach. Priority is given to the symptomatic side, and teeth within this quadrant are extracted. Further extractions in another quadrant are only performed once evidence of successful mucosal healing is seen in the first quadrant. The aim of this watchful, step-wise approach is to reduce the risk of creating multiple areas of MRONJ.
Scenario 1
A 70-year-old pensioner with early breast cancer receiving six monthly zoledronic acid attends with retained carious roots in the upper left and lower right quadrants. Only the upper left region is symptomatic. She has had three infusions of zoledronic acid to date and was due the next dose in three weeks time. Treatment included delaying the upcoming infusion following discussion and agreement with the oncology team. First the roots in the upper left quadrant were extracted under local anaesthesia and following healing of the sites, the roots in the lower right quadrants were also extracted under local anaesthesia. At the subsequent one month review, full mucosal coverage was evident and the oncology team were notified so that the delayed zoledronic acid infusion could be rescheduled.
Retained roots approach
Elective root retention is an approach that has been used by restorative dentists for many years as a basis for overdenture abutments.24 Commonly, these are roots with sclerosed canals and no apical infection or those that have been electively root treated and decoronated. Following successful orthograde root treatment, the canal can be sealed off with an appropriate restorative material and any residual coronal tissue removed. Following decoronation, maintaining oral hygiene around the roots is straightforward and an overdenture may be fitted. The retained roots approach has long been used in patients at risk of osteoradionecrosis and may now also be considered in patients at risk of MRONJ for teeth where coronal restoration is not possible. The aim of such an approach would be to avoid bony manipulation that may trigger MRONJ.
Scenario 2
A 54-year-old nurse is referred to the jaw necrosis clinic by her dentist with a palatal wall fracture of the upper left first molar which has been deemed unrestorable. She has a history of early breast cancer treated with six monthly infusions of zoledronic acid for four years. In order to reduce the risk of MRONJ, the jaw necrosis clinic recommends the tooth not be extracted but the tooth root filled, decoronated and coronally sealed.
The unconventional treatments suggested above should be seen as interim measures while approaches and techniques are being investigated for safe extraction of teeth in this vulnerable group. A number of methods are potentially showing promise such as platelet rich fibrin (PRF) and plasma (PRP) as well as the application of locally delivered bone morphogenic proteins (BMPs) and the use of piezosurgery.25 If these new approaches show sustained and reliable outcomes, then these interim and unconventional options may no longer be required. Clearly, it is not the dental extractions themselves that pose the challenge in these patients at risk of MRONJ but rather the MRONJ lesions that can occur as a consequence.
Summary
Bisphosphonates given to postmenopausal women with intermediate to high risk, early stage breast cancer, are beneficial in reducing breast cancer recurrence and mortality. Both bisphosphonates recommended by the European consensus panel (oral clodronate and IV zoledronic acid) are equally effective in reducing breast cancer recurrence and mortality. However, clodronate has a lower risk of MRONJ than zoledronic acid, the highest rates in the adjuvant breast cancer studies being 0.3% and 1.5% respectively. In the osteoporosis setting, it is well established that the nitrogen containing oral bisphosphonates such as alendronic acid have a very low MRONJ risk and that extractions and dental implants can still be performed.1 The use of clodronate (non-nitrogen bisphosphonate) would incur the same benefits as zoledronic acid (nitrogen containing bisphosphonate) with regards to reduction in breast cancer recurrence but with little to no change to dental treatment. One possible advantage of IV zoledronic acid over oral clodronate is improved compliance. Low compliance with oral bisphosphonates has been documented in osteoporosis patients with rates as low as 25–35% at one year.26 Administering the bisphosphonate intravenously every six months enables monitoring of patient compliance. However, compliance rates with oral bisphosphonates in early breast cancer studies were relatively high with a rate of 78% in one study.10 In a double blinded, adjuvant breast cancer study using oral clodronate and placebo, the compliance rates were 56% and 60% respectively suggesting that drug side effects are not the only factor in compliance.9 Patient choice is an important factor when selecting drug treatments and the SWOG SO307 study comparing IV zoledronic acid and oral bisphosphonates found that 76% of women stated a preference for oral versus IV bisphosphonates if they both had the same efficacy.27 Women being offered adjuvant bisphosphonate therapy should be made aware of both bisphosphonates and informed of the advantages and disadvantages of each including the difference in MRONJ risk.
The risk of MRONJ increases with both bisphosphonate dose and duration of exposure, so the risk can be reduced by using the lowest dose of bisphosphonate for the shortest duration that still provides the clinical benefit (reduction in breast cancer recurrence and mortality). In the early breast cancer trials, the risk of MRONJ from oral bisphosphonates was higher than in osteoporosis patients treated with oral bisphosphonates. This may simply be related to differences in study size between adjuvant breast cancer studies and osteoporosis studies but there are clear differences in the two patient groups (for example, immediate prior chemotherapy in breast cancer patients) and so we must be cautious in treating the two groups in the same way without further data.
It is important to remember that for women with intermediate to high risk early breast cancer, the risks of recurrence and death from their breast cancer are much higher than their risk of MRONJ. However, all patients offered adjuvant bisphosphonates (both oral and IV) should be made aware of the small but serious risk of MRONJ and given instructions about MRONJ risk reduction. Due to the very long half-life of bisphosphonates in bone (estimated > ten years), the risk of MRONJ may continue for many years after completion of adjuvant cancer treatment. This requires long-term vigilance on the part of the patient and may be helped by the use of a Dental Alert Card to inform dental health professionals of the MRONJ risk and the need for ongoing preventative measures.
Denosumab, a humanised antibody against RANK ligand that inhibits osteoclast function and associated bone resorption, is currently used alongside bisphosphonates in the metastatic setting.28 Studies are currently underway in the early breast cancer setting to assess the utility of denosumab in reducing breast cancer recurrence in bone.2 From a MRONJ risk perspective, denosumab is an attractive alternative to bisphosphonates as it does not bind to bone and so the antiresorptive effects subside after six months of treatment cessation.1 However, as the MRONJ risk while on denosumab treatment is considered to be the same as that of zoledronic acid, the benefit for the patient may be limited to reduction in the duration of risk once the antiresorptive agent is stopped.
In conclusion, dental health professionals across all the dental specialties should be made aware of this recent change in bisphosphonate use as breast cancer is the commonest cancer in the UK and many more patients will be receiving bisphosphonates in the coming months and years.
References
Ruggiero S L, Dodson T B, Fantasia J et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw-2014 update. J Oral Maxillofac Surg 2014; 72: 1938–1956.
Patel V, Kelleher M, Sproat C, Kwok J, and McGurk M . New cancer therapies and jaw necrosis. Br Dent J 2015; 219: 203–207.
Rosen L S, Gordon D, Tchekmedyian S et al. Zoledronic Acid Versus Placebo in the Treatment of Skeletal Metastases in Patients With Lung Cancer and Other Solid Tumours: A Phase III, Double-Blind, Randomized Trial – The Zoledronic Acid Lung Cancer and Other Solid Tumours Study Group. J Clin Oncol 2003; 21: 150–157.
Berenson J R, Lichtenstein A, Porter L et al. Long-term pamidronate treatment of advanced multiple myeloma patients reduces skeletal events. Myeloma Aredia Study Group. J Clin Oncol 1998; 16: 593–602.
Coleman R E . Clinical Features of Metastatic Bone Disease and Risk of Skeletal Morbidity. Clinical Cancer Research 2006; 12: 6243s–6249s.
Early Breast Cancer Trialists' Collaborative Group. Adjuvant bisphosphonate treatment in early breast cancer: meta-analyses of individual patient data from randomised trials. Lancet 2015; 386: 1353–1361.
Hadji P, Coleman R E, Wilson C et al. Adjuvant bisphosphonates in early breast cancer: consensus guidance for clinical practice from a European Panel. Ann Oncol 2016; 27: 379–390.
Breast Cancer Now. Lay summary of adjuvant bisphosphonates financial modelling. Breast Cancer Now, 2016.
Paterson A H, Anderson S J, Lembersky B C et al. Oral clodronate for adjuvant treatment of operable breast cancer (National Surgical Adjuvant Breast and Bowel Project protocol B-34): a multicentre, placebo-controlled, randomised trial. Lancet Oncol 2012; 13: 734–742.
von Minckwitz G, Mobus V, Schneeweiss A et al. German adjuvant intergroup node-positive study: a phase III trial to compare oral ibandronate versus observation in patients with high-risk early breast cancer. J Clin Oncol 2013; 31: 3, 531–539.
Gralow J, Barlow W E, Paterson A H G et al. Phase III trial of bisphosphonates as adjuvant therapy in primary breast cancer: SWOG/Alliance/ECOG-ACRIN/NCIC Clinical Trials Group/NRG Oncology study S0307. J Clin Oncol 2015; 33: abstract 503.
Gnant M, Mlineritsch B, Stoeger H et al. Zoledronic acid combined with adjuvant endocrine therapy of tamoxifen versus anastrozol plus ovarian function suppression in premenopausal early breast cancer: final analysis of the Austrian Breast and Colorectal Cancer Study Group Trial 12. Ann Oncol 2015; 26: 313–320.
Coleman R, de Boer R, Eidtmann H et al. Zoledronic acid (zoledronate) for postmenopausal women with early breast cancer receiving adjuvant letrozole (ZO-FAST study): final 60-month results. Ann Oncol 2013; 24: 398–405.
Rathbone E J, Brown J E, Marshall H C et al. Osteonecrosis of the jaw and oral health-related quality of life after adjuvant zoledronic acid: an adjuvant zoledronic acid to reduce recurrence trial subprotocol (BIG01/04). J Clin Oncol 2013; 31: 2685–2691.
Lo JC, O'Ryan F S, Gordon N P et al. Prevalence of Osteonecrosis of the Jaw in Patients With Oral Bisphosphonate Exposure. J Oral Maxillofac Surg 2010; 68: 243–253.
Malden N, Lopes V . An epidemiological study of alendronate-related osteonecrosis of the jaws. A case series from the south-east of Scotland with attention given to case definition and prevalence. J Bone Miner Metab 2012; 30: 171–182.
Khan A A, Morrison A, Hanley D A et al. Diagnosis and management of osteonecrosis of the jaw: A systematic review and international consensus. J Bone Min Res 2015; 30: 3–23.
Cancer Research UK. Breast cancer statistics. Available at http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer (accessed October 2017).
Patel V, Ormondroyd L, Lyons A, and McGurk M . The financial burden for the surgical management of osteoradionecrosis. Br Dent J 2017; 222: 177–180.
Ripamonti C I, Maniezzo M, Campa T et al. Decreased occurrence of osteonecrosis of the jaw after implementation of dental preventive measures in solid tumour patients with bone metastases treated with bisphosphonates. The experience of the National Cancer Institute of Milan. Ann Oncol 2009; 20: 137–145.
Dimopoulos M A, Kastritis E, Bamia C et al. Reduction of osteonecrosis of the jaw (ONJ) after implementation of preventive measures in patients with multiple myeloma treated with zoledronic acid. Ann Oncol 2009; 20: 117–120.
Montefusco V, Gay F, Spina F et al. Antibiotic prophylaxis before dental procedures may reduce the incidence of osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates. Leuk Lymphoma 2008; 49: 2156–2162.
AAE Special Committee on Bisphosphonates Endodontic implications of bisphosphonate-associated osteonecrosis of the jaws. American Association of Endodontists Position Paper. 2010. Available online at https://www.aae.org/uploadedfiles/clinical_resources/guidelines_and_position_statements/bisphosonatesstatement.pdf (accessed October 2017).
Patel V, Sproat C, Kwok J, Beneng K, Thavaraj S, and McGurk M . Histological evaluation of mandibular third molar roots retrieved after coronectomy. Br J Oral Maxillofac Surg 2014; 52: 415–419.
V. Patel D. Patel M. McGurk C. Sproat and J. Kwok . Flapless piezoelectric surgery in the management of jaw necrosis – a case series. Oral Surg 2017; DOI:10.1111/ors.12262.
Silverman S L, Schousboe J T, Gold D T . Oral bisphosphonate compliance and persistence: a matter of choice? Osteoporos Int 2011; 22: 21–26.
Gralow J, Barlow W E, Paterson A H G et al. SWOG S0307 phase III trial of bisphosphonates as adjuvant therapy in primary breast cancer: Comparison of toxicities and patient-stated preference for oral versus intravenous delivery. J Clin Oncol 2014; 32: 558.
Poznak C H V, Temin S, Yee G C et al. American Society of Clinical Oncology executive summary of the clinical practice guideline update on the role of bone-modifying agents in metastatic breast cancer. J Clin Oncol 2011; 29: 1221–1227.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Patel, V., Mansi, J., Ghosh, S. et al. MRONJ risk of adjuvant bisphosphonates in early stage breast cancer. Br Dent J 224, 74–79 (2018). https://doi.org/10.1038/sj.bdj.2017.1039
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.1039
This article is cited by
-
The presenting dental status of solid tumours with bone metastases requiring bone-targeting agents - part 1: an overview
British Dental Journal (2022)
-
The presenting dental status of solid tumours with bone metastases requiring bone-targeting agents - part 2: breast cancer
British Dental Journal (2022)
-
The presenting dental status of solid tumours with bone metastases requiring bone-targeting agents - part 4: miscellaneous cancers
British Dental Journal (2022)
-
The prosthodontic management of medication-related osteonecrosis of the jaw: a case report
British Dental Journal (2021)
-
Deciphering novel chemotherapy and its impact on dentistry
British Dental Journal (2020)