Key Points
-
Provides an overview of the aetiology and classification of dens invaginatus lesions.
-
Discusses the clinical features of this anomaly which can lead to early diagnosis.
-
Provides an in depth discussion on the treatment options and management strategies for dens invaginatus.
-
Reviews the clinical challenges of treating such lesions.
Abstract
Dens invaginatus is a developmental malformation, in which there is an infolding of enamel into dentine. These infolds represent stagnation sites for bacteria and can predispose to dental caries. The carious infection can spread via enamel and dentine to contaminate the pulp and cause soft tissue necrosis. The altered and sometimes complex anatomy of affected teeth can make endodontic management challenging. Early diagnosis is therefore essential as prophylactic treatment of the dens can prevent degeneration and pulpal necrosis. The aim of this article is to review the aetiology, classification, diagnosis and management of teeth affected with dens invaginatus. Emphasis will be placed on describing the clinical features of this anomaly. Treatment options, management strategies and the challenges faced in managing this condition will be discussed.
Similar content being viewed by others
Introduction
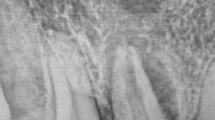
Dens invaginatus (DI) is a developmental dental anomaly where there is an invagination of the enamel organ into the dental papilla, before calcification is complete.1 The invagination begins in the crown and may extend into the root (Fig. 1).
Type II: the invagination extends into the pulp chamber but remains within the root canal with no communication with the periodontal ligament. Type IIIA: the invagination extends through the root and communicates laterally with the periodontal ligament space through a pseudo-foramen. Type IIIB: the invagination extends through the root and communicates with the periodontal ligament at the apical foramen; b) Intraoral radiograph illustrating a Type I Oehlers dens invaginatus on a lateral incisor. Notice the large periapical radiolucency; c) Intraoral radiograph of a lateral incisor with a Type II lesion; d) Intraoral radiograph of a canine with an Oehlers Type IIIA dens lesion
As a result, an infolding of the enamel into dentine occurs which creates a pocket of organic material underneath the enamel surface. These lesions are clinically relevant as bacteria from the oral cavity can contaminate and propagate within these malformations, leading to the development of early caries and consequently pulp death.1
Although these lesions usually form under the palatal pit or cusp tip, they can be extensive and grossly distort the anatomy of the root canal system (Fig. 1).2
The altered tooth morphology and concurrent pulpal necrosis (in an immature tooth) can disturb root formation. Therefore teeth with DI may present with wide open or 'blunderbuss' open apices, further complicating endodontic management. Therefore early diagnosis and prophylactic treatment of these lesions is important if pulp vitality is to be maintained.
Dens invaginatus lesions were first described in 1794 after being discovered in the tooth of a whale by Ploquet.2 A number of different terms have been used to describe the condition including dens in dente, dentoid in dente, invaginated odontome, dilated gestant odontome, dilated composite odontome and tooth inclusion.1
Aetiology
A number of theories regarding the aetiology of DI have been proposed. These include infection,3 trauma,4 growth pressure on the dental arches during odontogenesis causing infolding of the enamel5 and rapid proliferation of the internal enamel epithelium into the underlying dental papilla.6 However, the definitive cause of the lesions remains unclear.1
Authors have looked at genetic factors that could be responsible for dens invaginatus. During tooth development, growth molecules have been shown to regulate the folding and development of the enamel organ.7 If these genetically determined growth factors are absent or altered, the morphology of developing teeth can be disturbed.8,9,10,11,12 This theory is supported by the fact that DI can have a familial tendency, with the parents and siblings of DI patients also being affected by similar lesions,8 and that these lesions are associated with other genetically determined anomalies.13,14,15
Classification
There have been numerous attempts to classify DI.16,17,18,19,20 The most widely used classification system was produced by Oehler17 and this system separates these lesions into three simple categories. An understanding of these categories will help when discussing the appropriate treatment options for each lesion (Fig. 1).
-
Class I: This is a partial invagination that is confined to the crown of the tooth. These lesions involve dentine and enamel but do not extend past the cement-enamel junction (CEJ) or involve the pulp.
-
Class II: This partial invagination extends beyond the crown of the tooth and into the root, beyond the CEJ. These lesions may or may not involve pulp, but remain within the anatomy of the root. There is no communication with the periodontal ligament.
-
Class IIIa: This complete invagination extends through the root. It communicates with the periodontal ligament through a second foramen on the lateral aspect of the tooth. There is usually no involvement of the pulp itself, but it causes a significant anatomical malformation.
-
Class IIIb: This complete invagination extends through the root, and communicates with the periodontal ligament at the apical foramen. Again, often there is no direct involvement of the pulpal anatomy but the lesion causes significant disruption to the dental anatomy.
Prevalence
Dens invaginatus lesions have been reported to affect 0.3% to 10% of the population.2 These figures may initially seem small, however, they are significant as they suggest that dens lesions occur more commonly than other developmental dental anomalies, including peg-shaped lateral incisors (0.8%), germination (0.3%) and taurodontism (0.3%).1
The teeth most commonly affected by DI are lateral incisors21 followed by maxillary central incisors, and more rarely premolar and canine teeth. Although rare, case reports have detailed DI lesions in mandibular teeth,22,23 deciduous teeth,24,25,26 supernumerary teeth27,28 and multiple lesions found in a single tooth.22,27,29 In 43% of cases, DI can be bilateral.8 Therefore, if a dens is identified, clinicians should always check the contralateral tooth.
Clinical examination
DI are often asymptomatic and the crowns of affected teeth may show very little external deformity. Extensive malformations are more likely to result in abnormal crown anatomy. Patients may complain of an abnormally shaped tooth which may be wider mesially/distally; wider labially/lingually;30,31 associated with an exaggerated talon cusp32 or even conical in shape.32,33
If undiagnosed, affected teeth are prone to developing caries and peri-radicular pathology. Clinicians should be mindful that lateral incisors are the most commonly affected teeth. If these teeth exhibit any clinical features of a dens (such as a pronounced talon cusp or incisal notching), adjunctive radiographic examination should be performed to exclude the possibility of an underlying invagination (Fig. 2).33
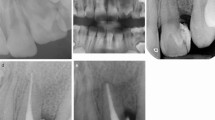
Note the pronounced palatal cingulum; b) Post-treatment: The central incisors were sealed with acid-etched flowable composite; c) A pre-treatment lateral incisor with a Type I dens invaginatus lesion and a large periapical radiolucency; d) The Type I invaginatus lesion was incorporated into the access cavity; e) Post-treatment radiograph of the Type I dens invaginatus lesion. The lesion was fully incorporated into the access cavity and the tooth obturated with thermoplastic GP
Finally, patients may present with symptoms of irreversible pulpitis or apical periodontitis. The possibility of DI should be considered in cases where there is no obvious history of trauma or caries, especially if the lateral incisors are affected bilaterally.
Radiographic features
Invagination lesions usually appear as radiolucent pockets underneath the cingulum and incisal edges of affected teeth. These pockets can be surrounded by radio-opaque enamel and may either be confined to the crown or involve the pulp.
More extensive lesions may appear as fissures, with or without radio-opaque borders. These fissures may involve the pulp and the root canal anatomy may appear complex.37 Communications between the invaginations and the periodontal ligament may be evident either on the lateral aspects of the tooth or its apex. If such communications are present and a patient develops pulpal pathology, a 'butterfly' like periapical radiolucency may be seen, corresponding to two sources of inflammation.33
These features may be picked up as incidental findings on routine radiographs and warrant further investigation. Periapical radiographs are usually the image of choice for identifying DI lesions, however two images would be required at different horizontal angulations to ensure the lesion is not masked on a single view.33
The use of cone beam computed tomography (CBCT) has been described in assessing dens invaginatus lesions prior to treatment.38 CBCT can provide a more detailed 3D view of the complex anatomical variations seen in dens invaginatus malformations. It can help the clinician diagnose the class of dens affecting the tooth and allow clinicians to assess the feasibility of any planned endodontic treatment, especially proximity of adjacent anatomical structures if apical surgery is being planned.
Management strategies
The anatomy of DI lesions can be extremely complex.39 Consequently, adequate chemo-mechanical debridement and obturation of these malformations can be challenging. Treatment is further complicated by the tendency for affected teeth to develop pulpal necrosis, often before root formation has taken place. This can result in a 'blunderbuss' apex which can complicate obturation of an affected tooth due to the lack of an apical constriction to compact gutta percha against (Figs 3a-c). These factors had previously meant that many teeth affected with DI lesions were routinely extracted if patients presented with peri-radicular pathology. However, improvements in modern endodontics have now meant that more of these teeth can be treated successfully with a combination of non-surgical and sometimes apical surgical techniques. Despite these improvements, treatment of these lesions is still challenging and should not be underestimated. Consequently most cases tend to be treated in specialist practice or the secondary care sector. The management of invaginated immature teeth with necrotic pulps can be extremely complex.40 In these situations a multi-professional approach may need to be considered. Teeth with complex and untreatable dens may need to be extracted and replaced with a prosthesis. Alternatively the resulting space can be orthodontically closed (to avoid a prosthesis) or unaesthetically wide spaces should be orthodontically optimised to allow prosthodontic rehabilitation.
Notice how the dens has been incorporated into the root canal system; d) A pre-treatment intraoral radiograph of a Type III dens invaginatus lesion. The internal root canal anatomy is grossly distorted and the invagination communicates with the periodontal ligament laterally; e) Post treatment: the lesion was filled with MTA and the root canal system was obturated with thermoplastic GP; f) One year post treatment and the lesion is starting to show signs radiographically of bony healing
Within this section, potential operative management options for DI lesions will be discussed.
Treatment of Oehler's Class I Lesions
Class I invaginations can be minimal. As soon as a lesion is detected either clinically or radiographically, the palatal surface of the tooth should be sealed with acid-etched flowable composite to prevent the development of caries (Figs 2a and b).2
If pulpal necrosis is evident, de nova root canal treatment should be performed. The root canals of teeth with Class I lesions are usually not grossly deformed. However, the entire invagination should be incorporated into the access cavity (Figs 2c-e).
Instrumentation of the invagination can be achieved with Gates Glidden burs or ultrasonic tips (Figs 4a and b).41 An operating microscope can be useful in ensuring that the invagination is completely eradicated.33
d) An ultrasonic tip can be used to activate irrigants and ensure penetration of the irrigant into the invagination; e) Whilst placing a MTA plug a paper point can be held upside and used to condense and adapt the MTA to the apical walls; f) Whilst placing a MTA plug a paper point can be held upside and used to condense and adapt the MTA to the apical walls; g) A Class IIIb invagination pre-and post-treatment after obturation of the invagination only
Treatment of Oehler's Class II Lesions
In Class II invaginations, a more extensive defect is present. Caries can develop deep within these lesions, leaving the enamel surface appearing intact and underlying caries clinically undetectable. It is therefore not advisable to seal these lesions using the methods described for Class I lesions. Opening the entrance of the invagination will allow any caries to be visualised and removed with long-shanked burs (Fig. 4c). The invagination should be thoroughly debrided using ultrasonic instruments and hypochlorite. If the tooth does not exhibit any signs of pulpal pathology the invagination can be restored without accessing the root canal system. As Class II lesions may be in close proximity with the pulp, the invagination can be dressed with a material that will promote hard tissue formation such as mineral trioxide aggregate (MTA).33 The remaining defect can then be restored and sealed with composite resin.
However, MTA has a prolonged setting time and can be difficult to manipulate. It is also expensive and has the potential to discolour the tooth, which is not ideal in the anterior dental segment. An alternative would be to use setting calcium hydroxide cement, for example, Dycal, when operatively managing an Oehler's Class II invagination.
If the invagination and resultant caries has caused pulpal necrosis, root canal therapy is indicated. As with Class I defects, the invagination should be incorporated into the defect using suitable diamond burs, long shanked stainless steel round burs and ultrasonic alloy tips.
Treatment of Oehler's Class III Lesions
The management of Class III lesions is more complex. If the tooth is asymptomatic and does not exhibit signs of pulpal disease, the tooth should be sealed only. Due to the close proximity of the invagination to the root canal system, prophylactically accessing and debriding Class III invaginations would likely result in pulpal involvement. Therefore, a more conservative approach is recommended.
Peri-invaginatus periodontitis is a condition in which the tissue within an invagination becomes infected. The pulp itself may still remain vital and healthy, with the tooth responding to pulp testing. Treatment of these lesions involves attempting to endodontically treat the infected invagination. This is complex and referral to an endodontic specialist is indicated. Depending on the relationship of the invagination and root canal system, the invagination can either be treated in isolation (Fig. 4g) or in combination with the root canal system if both the pulp and invagination are infected.
Given that histologically the pulp/dentine complex and invagination are often interconnected,33 endodontic therapy of both systems is not unwise and will allow the patient to have the tooth treated in its entirety.42 To manage such lesions, good quality peri-apical radiographs (often at different angles) and an operating microscope are essential. The invagination will be lined with enamel and cementum. Endodontic files are not indicated for use to debride these lesions as they will be ineffective. Ultrasonic alloy tips can be used to debride the lesions, and irrigants should be ultrasonically activated (Fig. 4d) to maximise their efficacy and ensure that they reach all parts of the anomaly.43 The invagination will communicate with the periodontal ligament space and will need obturating with MTA to promote healing of the peri-radicular tissues (Figs 3d-f). The pulpal portion of the tooth should be treated conventionally with endodontic files, thorough irrigation of sodium hypochlorite (which should be ultrasonically activated) before being obturated with thermoplastic gutta percha (to ensure that the complex anatomy has been completely sealed) (Figs 3d-f).
The tooth should then be kept under long term review. If symptoms do not improve, microsurgery can be considered or alternatively the dental unit should be extracted.
Conclusion
Teeth affected with dens invaginatus lesions are predisposed to developing pulpal disease. The resulting endodontic treatment is complex due to the unpredictable and aberrant internal anatomy of teeth affected with these lesions. Although CBCT, modern endodontics and surgical endodontics have improved the management of such anomalies, early identification and prophylactic treatment of these lesions is imperative in preventing pulpal pathology from developing and avoiding complex and specialised endodontic treatment.
References
Alani A A, Bishop K . Dens Invaginatus. Part 1: Classification, prevalence and aetiology. Int Endod J 2008; 41: 1123–1136.
Hulsmann M . Dens Invaginatus: aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endo J 1997; 30: 79–90.
Sprawson E C . Odontomes. Br Dent J 1937; 33: 177–201.
Gustafson G, Sunderberg S . Dens in dente. Br Dent J 1950; 88: 111–122.
Atkinson S R . The permanant maxillary lateral incisor. Am J Ortho 1943; 29: 685–698.
Rushton M A . A collection of dilated composite odontomas. Br Dent J 1937; 65–85.
Kettunen P, Laurikkala J, Itäranta P, Vainio S, Itoh N, Thesleff I . Associations of FGF-3 and FGF-10 with signaling networks regulating tooth morphogenesis. Dev Dyn 2000; 219: 322–332.
Grahnen H, Lindahl B, Omnell K . Dens invaginatus. I. A clinical, roentgenological and genetical study of permanent upper lateral incisors. Odontol Revy 1959; 10: 115–137.
Casamassimo P S, Nowak A J, Ettinger R L, Schlenker D J . An unusual triad: microdontia, taurodontia, and dens invaginatus. Oral Surg Oral Med Oral Pathol 1978; 45: 107–112.
Ireland E J, Black J P, Scures C C . Short roots, Taurodontia and multiple dens invaginatus. J Pedodont 1987; 11: 164–175.
Pokala P, Acs G . A constellation of dental anomalies in a chromosomal deletion syndrome (7q32): case report. Pediatr Dent 1994; 4: 306–309.
Hosey M T, Bedi B . Multiple dens invaginatus in two brothers. Endod Dent Traumatol 1996; 12: 44–47.
Peck S, Peck L, Kataja M . Prevalence of tooth agenesis and peg-shaped maxillary lateral incisor associated with palatally displaced canine (PDC) anomaly. Am J Ortho Dento Ortho 1996; 110: 441–443.
Segura J J, Hattab F, Rios V . Maxillary canine transpositions in two brothers and one sister: associated dental anomalies and genetic basis. ASDC J Dent Child 2002; 69: 54–58.
Kansu O, Avcu N . Mandibular lateral incisor-canine transposition associated with dental anomalies. Clin Anat 2005; 18: 446–448.
Hallett G E . The incidence, nature and clinical significance of palatal invagination in the maxillary incisors teeth. Proc Royal Soc Med 1953; 46: 491–499.
Oehlers F A . Dens Invaginatus. I. Variations of the invagination process and associated anterior crown forms. Oral Surg Oral Med Oral Pathol 1957; 10: 1204–1218.
Ulmansky M, Hermel J . Double dens in dente in a single tooth. Oral Surg Oral Med Oral Pathol 1964; 17: 92–97.
Vincent-Townend J . Dens invaginatus. J Dent 1974; 2: 234–238.
Schulze C, Brand E . Uber den dens invaginatus (Dens in dente). Zahna¨rztliche Welt, zahna¨rztliche Reform 1972; 81: 569–573: 613–20, 653–60; 699–703.
Hamasha A A, Al-Omari Q D . Prevalence of dens invaginatus in Jordanian adults. Int Endod J 2004; 37: 307–310.
Conklin W W . Bilateral dens invaginatus in the mandibular incisor region. Oral Surg Oral Med Oral Pathol 1978; 45: 905–908.
Kharangate N, Figueiredo N R, Fernandes M, Lambor R . Bilateral dens invaginatus in the mandibular premolars – Diagnosis and treatment. Contemp Clin Dent 2015; 6: 428–431.
Rabinowitch B Z . Dens in dente: primary tooth-report of a case. Oral Surg Oral Med Oral Pathol 1952; 5: 1312–1314.
Holan G . Dens invaginatus in a primary canine: a case report. Int J Paediatr Dent 1998; 8: 61–64.
Eden E K, Koca H, Sen B H . Dens invaginatus in a primary molar: report of case. ASDC J Dent Child 2002; 69: 49–53.
Archer W H, Silverman L M . Double dens in dente in bilateral rudimentary supernumerary central incisors. Oral Surg Oral Med Oral Pathol 1950; 3: 722.
Shifman A, Tamir A . Dens invaginatus with concrescent supernumerary tooth. Oral Surg Oral Med Oral Pathol 1979; 47: 391.
Conklin W W . Double bilateral dens invaginatus in the maxillary incisor region. Oral Surg Oral Med Oral Pathol 1975; 39: 949–952.
Khabbaz M G, Konstantaki M N, Sykaras S N . Dens invaginatus in a mandibular lateral incisor. Int Endod J 1995; 28: 303–305.
Girsch W J, McClammy T V . Microscopic removal of dens invaginatus. J Endod 2002; 28: 336–339.
Ridell K, Mejàre I, Matsson L . Dens invaginatus: a retrospective study of prophylactic invagination treatment. Int J Paediatr Dent 2001; 11: 92–97.
Bishop K, Alani A . Dens invaginatus. Part 2: clinical, radiographic features and management options. Int Endod J 2008; 41: 1137–1145.
De Smit A, Jansen H W, Dermaut L . An histological investigation of invaginated human incisors. J Biol Buccale 1984; 12: 201–209.
Rotstein I, Stabholz A, Heling I, Friedman S . Clinical considerations in the treatment of dens invaginatus. Endod Dent Traumatol 1987; 3: 249–254.
Kronfeld R . Dens in dente. J Dent Res 1934; 49–66.
Gonçalves A, Gonçalves M, Oliveira D P, Gonçalves N . Dens invaginatus type III: report of a case and 10-year radiographic follow-up. Int Endod J 2002; 35: 873–879.
Patel S . The use of cone beam computed tomography in the conservative management of dens invaginatus: a case report. Int Endod J 2010; 43: 707–713.
Tagger M . Nonsurgical endodontic therapy of tooth invagination. Oral Surg Oral Med Oral Pathol 1977; 43: 124–129.
Holtzman L, Lezion R . Endodontic treatment of maxillary canine with dens invaginatus and immature root. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 82: 452–455.
Skoner J R, Wallace J . Dens invaginatus: another use for the ultrasonic. J Endod 1994; 20: 138–140.
Chen Y H, Tseng C C, Harn W M . Dens invaginatus: review of formation and morphology: 2 case reports. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 86: 347–352.
Mozo S, Llena C, Forner L . Review of ultrasonic irrigation in endodontics: increasing action of irrigating solutions. Med Oral Patol Oral Cir Bucal 2011; 17: e512–e516.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Gallacher, A., Ali, R. & Bhakta, S. Dens invaginatus: diagnosis and management strategies. Br Dent J 221, 383–387 (2016). https://doi.org/10.1038/sj.bdj.2016.724
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.724
This article is cited by
-
Dens invaginatus: a review and orthodontic implications
British Dental Journal (2021)
-
Double rooted lateral?
British Dental Journal (2020)