Key Points
-
Germany has more dentists, dental technicians and dental nurses than any other EU member state.
-
Germany has a comprehensive oral health insurance scheme funded in equal measure by those in employment and their employers.
-
Access to care is excellent and 80% of German adults visited a dentist in 2013.
Abstract
Germany is the largest member state of the EU, both in terms of population and number of dentists and dental team members, with 80.5 million inhabitants and 69,236 active dentists, 182,000 dental nurses and 54,000 dental technicians in 2012. General dental practitioners in private practice provide almost all oral healthcare under a health insurance scheme. The tradition of compulsory health insurance goes back to the nineteenth century when it was introduced by Bismarck. Today, the majority of the German population (86%) are members of a statutory sick fund which reimburses a legally prescribed standard oral healthcare package provided by dentists in contract with the health insurance system. A smaller number are privately insured. Access to oral healthcare is excellent and 80% of adults visited a dentist in 2013. Healthcare expenditure in Germany has long been considered high. This has led to several reforms in recent years. This paper outlines the system for the provision of oral healthcare in Germany and explains and discusses the latest changes.
Similar content being viewed by others
Introduction
Co-operation between the European Union (EU) member states has increased in many fields. Although organisation of healthcare and oral care provision within each member state is decided by each member state and not centrally by the European Commission, there has been some harmonisation of systems across the EU. The recent directive on cross border healthcare1 together with the directives on education and specialisation2 and control systems for dental materials among others require co-operation.
The freedom of movement of professionals within the EU/European Economic Area (EEA) has enabled several thousand EEA qualified dentists, who are non-UK EEA nationals, to immigrate and practise in the United Kingdom. At the end of 2013, the names of 6,827 non-UK EEA nationals, who graduated from EEA dental schools outside the UK, were on the Dentists Register.3 This represented 17% of all dentists registered to work in the UK. According to data gathered by the Council of European Chief Dental Officers (CECDO), the UK had not only received more immigrant EEA dentists than any of the other 27 EU member states but also had more than all the other 27 put together.4 In 2011, an investigation into differences between the practice of dentistry in the UK and in 19 EEA member states found surprising variations.5 Against this background this series will describe the systems for the provision of oral healthcare in the EEA member states with the largest population (France, Germany, Italy) and those from which more than 500 dentists per member state have moved to the UK.
The first paper in the series describes the system for the provision of oral healthcare in Germany, which in terms of population (81,000,000) and total gross national product is the largest in the EEA. At the end of 2013 the names of 359 German dentists were listed in the Dentists Register.3 The paper covers the following aspects:
-
Insurance based healthcare provision system
-
Payment system and co-funding of oral healthcare for patients (benefits)
-
Reimbursement of costs of oral healthcare
-
Publicly funded services
-
Prevention and oral health promotion
-
Oral healthcare workforce
-
Dental education
-
Specialist training
-
Costs of oral healthcare
-
Epidemiology
-
Recent changes
-
Discussion.
Aim
The aim of this paper is to describe the system for the provision of oral healthcare in Germany and explain and discuss the latest changes.
Insurance based health care provision system
In the Federal Republic of Germany, responsibility for the healthcare system is divided between central government, the 16 federal states and self-governing bodies of physicians, hospitals, dentists, psychotherapists, and public sick funds. Health insurance is separated between statutory and private schemes. The statutory health insurance, the so-called Gesetzliche Krankenversicherung (GKV - SHI), occupies a central position in the healthcare system in Germany. The SHI system requires mandatory membership of a state-approved 'sick fund'. The vast majority of the German population (86%) are members of such a fund which reimburses legally prescribed standard packages of healthcare including oral healthcare. The highest national decision-making institution for the SHI scheme is the Federal Joint Committee (Gemeinsamer Bundesausschuss, G-BA). Established in 2004, at a federal level, this authority includes representatives of the public, sickness funds and the professional organisations and is responsible for defining and redefining the benefit packages for the SHI. Systematic reviews are regularly performed to assess the benefits, costs, and cost-effectiveness ratios of for example, pharmaceuticals and medical interventions.6,7
The SHI is organised regionally and in 2014 it was operated by 131 separate sickness funds (in 1995 there were 960). In addition, there are a few special insurance funds for certain companies or guilds as well as for certain groups of people (such as farmers). With minor exceptions, all funds provide similar benefits. Services are supplied on a contractual basis. At national level, the delivery of SHI oral healthcare is organised and dentists' fees negotiated by the Federal Association of Statutory Health Insurance Dentists (Kassenzahnärztliche Bundesvereinigung, KZBV) and locally it is organised by the regional dental authorities Regional Associations of Statutory Health Insurance Dentists (Kassenzahnärztliche Vereinigungen, KZV) in partnership with the sick funds. The regional associations of SHI dentists must deliver the health services that have been defined by law and in contract with the sickness funds. In doing so, the regional associations guarantee to the sickness funds and the insured population that these services meet all legal and contractual requirements. Due to their supervisory and regulatory role, the regional associations were established as self-governing, quasi-public corporations.
Payment system and co-funding of oral healthcare for patients (benefits)
The vast majority of adults and children use dental services on an annual basis. Services provided by practice-based dentists, and many other health professionals, are paid for from an agreed fee scale. Regulated reimbursement fee lists have been developed for physicians and dentists. There are two fee schedules per profession, one for SHI services and one for private treatments. Both guarantee free access to a wide range of basic healthcare services for the insured persons.
SHI-service
Healthcare expenditure in Germany has been considered to be high and this has led to several reforms in recent years. A so called Central Reallocation Pool or National Health Insurance Fund (Gesundheitsfonds) was established in 2009 to centralise the collection of all SHI contributions. At the same time, the level of SHI contributions was fixed nationally and applied uniformly to all separate public sick funds. The National SHI-fund collects and pools the health insurance contributions of all SHI members, which were previously collected and pooled by the regional sick funds. In addition to the insurance contributions collected from the insured persons and their employers, the government provides a subsidy for the health fund. It varies from year to year and was €11.5 billion in 2013. The dental profession viewed the introduction of the National Social Health Insurance Fund very critically. It has resulted in additional bureaucratic structures and doesn't resolve the problems of the SHI. The Federal Government can influence the costs by legislative actions only; cost containment is the responsibility of the sick-funds and not the Government.
As mentioned previously, the contribution rate for membership of any sick fund belonging to the SHI-system is fixed. From January 2011 to December 2014 it was set at 15.5% of an individual's total pay of which the insured person pays 8.2% and their employer 7.3%. From January 2015, the rate will become 14.6% of total pay and both the insured person and the employer will each pay 7.3%. Most dentists (99%) have a contract with the SHI system and belong to the regional Associations of SHI-Dentists (KZV). In principle, membership of a statutory sickness fund entitles all adults and children to receive oral healthcare and in a normal year about 80% of the adults and 60-70% of children make use of the system. Children and spouses of insured persons are co-insured without making any contributory payments of their own. Unemployed persons obtain coverage by paying a reduced contribution.
Private insurance schemes
Private healthcare schemes can either provide a complete health service for those who opt out of the SHI, or top-up cover for those who remain within it. About 11% of the working population - whose yearly gross income exceeds €53,550 (£44,000 per year in 2014) – are members of a private insurance scheme.8 The premium for private insurance is lower and private insurance schemes offer more flexible packages of care. However, coverage applies only to the insured persons and excludes spouses and/or children. Thus family members need to be insured separately.
Reimbursement of costs of oral healthcare
For clinical and radiographic examinations, diagnoses, fillings, oral surgery, preventive treatments for children, periodontology and endodontics the SHI covers 100% of the costs. For light cured composites the sick funds cover the costs equal to those of an amalgam filling and the patient has to pay the additional costs. For orthodontics the SHI-funds pay 80% of the cost of the care for children, if the need for treatment is recognised by the sickness fund. If the child does not meet the criteria of the sick fund directives, the parents have to pay the orthodontic treatment costs themselves or via a top-up-private insurance policy.
The reimbursement for advanced treatments from the statutory insurance has been subject to a system of fixed grants since 2005. This system of 'diagnosis-based fixed subventions' applies to all fixed and removable prosthodontics and implants. For these treatments, the patient receives a fixed amount irrespective of the treatment and pays the balance.
Public services
A limited number of dentists, about 450, are employed in the Public Dental Service (PDS) which, in some of the German federal states, conducts oral health screening of all children between three and 12 (and for some up to 16) years and group prevention. Parents are informed of any treatment needed, and it is then their responsibility to arrange for that treatment. In addition, public services exist in dental wards of hospitals (with 250 dentists), in universities (with 1,900 dentists) and in the Armed Forces (with 450 dentists).
Prevention and oral health promotion
As mentioned previously, the PDS provides group prevention: oral health education, screening, fluoridation etc) for children between the ages of three and 12 (and for adolescents with a high caries risk up to 16 years). In the federal states with little or no publicly funded oral health screening, private practitioners provide the vast majority of oral healthcare. Preventive programmes for groups of children started in 1989 and were introduced as a nationwide service by the Social Security Code (Sozialgesetzbuch V, 1988). At the same time, private dentists started their own Grassroots-Programme in which they developed a preventive programme for local kindergartens and schools. Regional dental chambers (associations), the Statutory Health Insurances and the communities have founded regional and national councils to promote oral health for children and adolescents. At federal level they are organised in Regional Working Groups for Children's Dentistry and Dental Hygiene and are responsible for the implementation of group prevention, which was outlined in federal laws for the health system in 2000.
In order to stimulate a further positive development of the children's and adolescents' oral health, individual prevention (IP) for children between six and 18 years was included in the SHI in 1991.8 IP covers, for example, professional tooth cleaning, fluoridation and fissure sealing of the molars.
Oral healthcare workforce
There are about 69,000 dentists in active practice in Germany.
Auxiliary personnel can only work under the supervision of a dentist; they cannot practise independently. The range of auxiliaries is fairly complex, leading progressively (with training) from dental chairside assistant (dental nurse) (Zahnmedizinische Fachangestellte) to dental hygienist. After three years training in a dental practice, attendance at a vocational school and a successful examination conducted by the regional Dental Chamber, they are awarded a registrable qualification (German Dual System 'Vocational Education').
A dental chairside assistant may then qualify as a Zahnmedizinische Fachassistentin (specialised chairside assistant, ZMF), or a Zahnmedizinische Verwaltungsassistentin (dental administration assistant, ZMV), or a Zahnmedizinische Prophylaxeassistentin (dental prophylaxis assistant, ZMP) or a Dentalhygieniker (dental hygienist). These qualifications are supervised by the German Dental Association (Bundeszahnärztekammer)9 (Council of European Dentists 2014).
The number of dental hygienists is low, just over 600, but there are over 15,000 specialised dental chairside assistants who have undergone extended training and perform supra-gingival scaling. The total number of dental chairside assistants (dental nurses) is estimated to be 182,000,10 that is, more than two per dentist.
A typical feature of German dentistry has been and still is a high number of dental technicians – 58,000 in 2011 – relative to the numbers of dentists.
Dental technicians are not permitted to treat patients. They are also trained in a dual system of 'vocational education' for three years: in a vocational school and in the dental laboratory. After a successful examination, conducted by the Chamber of Handicraft, they are awarded a registrable qualification.
Dental education
In 2013, dentistry was taught at 31 publicly funded dental schools which are within the Medical Faculties of universities and at one private dental school (in Witten-Herdecke). In total, there were 2,222 first year students and 1,813 graduates in 2012. The percentage of female dental students was above 60%. To enter a dental university, a student must have passed the general qualification for university entrance and, in addition, obtained a successful result in a Medical Courses Qualifying Test. The undergraduate course takes five years. A state examination certificate is part of the degree and it is a compulsory requirement for registration as a dentist with a regional dental chamber (association).
In order to register as a dentist and provide care within the SHI, a German dentist, with a German diploma, must complete a further two years of approved supervised experience in an existing SHI practice after leaving university. They can then apply to the admission committee of the KZV for registration. This vocational training is not required of dentists from European Economic Area (EEA) member states with an EEA diploma.
Continuing professional education (CPD) is mandatory for dentists practising in the SHI system. A mandatory minimum during a five year cycle is 125 credit points of CPD (one hour's CPD equals one credit point). Regular monitoring has to be completed every five years. In addition a dentist must undergo mandatory training in ionising radiation protection every five years. The compliance with mandatory CPD requirements is taken into account and there are consequences in case they fail to comply with what is required, if the requirements are not fulfilled within a certain delay. If dentists are non-compliant with the CPD requirements, they face financial sanctions (remuneration reductions) and may risk losing their social health insurance affiliation.
Specialist training
In recent years, postgraduate Master studies have been established by universities. They are mostly part-time, allowing students to continue to work in their own practices. The programmes are offered in implantology, functional therapy, periodontics, endodontics, orthodontics, oral surgery, oral aesthetics and lasers in dentistry. The courses are rated at 60-120 ECTS (European Credit Transfer System in which one ECT corresponds to 25-30 hours of work). These programmes provide dentists with enhanced skills but not recognitions as specialists.
Six dental specialties are recognised in Germany, although not in all 16 federal states. They are:
-
Oral surgery
-
Orthodontics
-
Dental public health
-
Periodontology
-
General dentistry
-
Paediatric dentistry [specialty from the former German Democratic Republic].
Periodontology is only recognised in Westphalia, while general dentistry is only recognised in Brandenburg. Training for all specialties lasts four years and takes place in university clinics and recognised training practices, except for dental public health, for which training takes place in the workplace and an academy.
In principle, there is no theoretical limitation as to the number of specialist trainees, because there are sufficient specialists dentists working in general dental practices with the permission to train a dentist in orthodontics or oral surgery. However, since all dentists who want to specialise have to attend one year at university, there is in fact a practical limitation. The trainee has the status of an employee and is paid a salary by his or her employer. After completion of the specialised training, the trainee has to pass an examination organised by the regional dental chamber. The dentist is then recognised as specialist and is registered by the German dental chamber (association).
Costs of oral healthcare
In 2012, the Federal Statistical Office (Statistisches Bundesamt) reported that in Germany, 11.3% of GDP was spent on healthcare and 0.7% of GNP was spent on oral care.
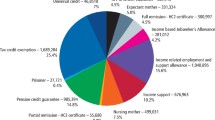
In 2012, the expenditure by the statutory health insurance system on oral care was an estimated €11.75 billion11 (BMG 2013). Patients contributed an estimated, further €10.44 billion and expenditure by Statutory Health Insurance for group - and individual prophylaxis, including fissure sealing, was about €512 million in 201112 (GKV 2013).
Thus the total expenditure on oral health in Germany can be estimated to be €22.70 billion.13
Epidemiology
National epidemiological studies of four age groups of the population have been conducted every ten years over the last 30 years. They have indicated that caries prevalence in children and young adults has decreased markedly since the early 1980s. In 2005, the mean national DMFT was 0.7 in 12-year-olds and 1.8 in 15-year olds. For adults (35-44-year-olds), the DMFT was 14.5, and for the 65-74-year-olds 22.114 (IDZ 2006). Total edentulousness was observed in 1.0% of the adult population and in 22.6% of the 65-74-year-olds all of whom had received prosthetic treatment. The number of teeth present had increased in both groups since the previous study. About 49% of the missing teeth in adults and 89% of those in over 65-year-olds had been replaced, predominantly with fixed prosthetics in the first group and removable partial dentures in the second group. Of the adults participating in the survey 1.4% overall and 2.6% of those over 65 years had implants. Deep pockets (>6 mm) were found in 0.8% of adolescents, 20.5% of adults and 39.8% of the over 65-year-olds. Greatest risk for advanced periodontal breakdown was found among smokers with low basic education.14 The next nationwide Fifth German Oral Health Survey (DMS V) is planned to take place in 2014-2015.
Recent changes
In 2010, the German Dental Association (BZÄK), the Federal Association of SHI-Dentists (KZBV) and scientific organisations worked together to develop a reform draft (Oral health despite handicap and old age, AuB-Konzept) for the elderly and disabled with the objective of improving the oral healthcare for people in need of nursing care. There is a great need for oral healthcare in these groups and also more sophisticated treatment plans must be taken into consideration as well as general anaesthesia. In 2012 a law was passed (Versorgungsstrukturgesetz) which can be regarded as first step towards the implementation of the AuB-Konzept. A new item 'fees for visiting immobile patients' was included in the scale of fees of the Statutory Health Insurance. This was a first step to compensate for the extra effort but unfortunately there are no additional fees for prevention or treatment.
In 2014, the German Legislative Authority proposed the change of the electronic health insurance card into an electronic health card (elektronische Gesundheitskarte – eGK) to promote electronic data transmission in the healthcare sector in order to reduce costs and to improve the quality of the medical services. The eGK contains the same administrative data as the old health insurance card. These include name, address, date of birth, sex, insurance number and so on. The eGK is designed so that it will allow medical data to be stored in an electronic format. The further development of the eGK and the creation of the infrastructure is the task of the professional associations and of Organization for Telematics Applications of the Health Card.15
In 2009, the general medical practices in the region of Nordrhein were equipped with the eGK for a test period. Before the end of 2011, the SHIs were obliged to provide at least 10% of their insured people with an eGK - more than five years after the planned date. Dental practices also had to be equipped for the use of the eGK. The costs of this equipment are covered by the respective insurance companies, which means by the insured people and their contributions. The main criticisms of the eGK from the health professions, as well as from patient organisations, were the high costs, the safeguarding of data protection and the prevention of data abuse.
Since 2004 the dental profession has had a statutory obligation to perform internal quality management of their practices and also external interdisciplinary quality management. The implementation of these statutory responsibilities is regulated by guidelines of the Federal Joint Committee (Gemeinsamer Bundesausschuss, GBA). At the end of 2010, for the first time, the measures for internal quality management were approved. Internal and external quality assurance is performed using indicators for procedure and by a comparison of different dental surgeries. Furthermore, obligatory guidelines for dentistry and general quality assurance guidelines for hospitals, outpatients' medical surgeries, and outpatients' dental practices have been prepared. The plan is that sample surveys in dental surgeries will be carried out annually in order to check patient records for completeness and accuracy.
Online evaluation programmes for potential patients of doctors and dentists have become popular. Many evaluation programmes of differing quality for medical practitioners have been developed. Many of them are not reliable. Before asking the question: 'Where do I find a competent practitioner?', the question should be: 'Where do I find a reliable online portal?'. Therefore, the BZÄK and KZBV have together with the medical associations prepared quality criteria, which are meant to support and advise programme operators in designing and structuring their online programmes, and also to assist the medical and dental practitioners and patients when looking for reliable programmes.16
Since 2013, there has been a law for patients' rights in Germany which unifies all the old regulations for patients' protection and their rights. Emphasis has been put on the following:
-
Patient records must contain full information and documentation of the treatment planned
-
An extensive liability clause (no general reverse of the burden of proof) must be included
-
Information on the procedure(s) to be followed in case of treatment failure(s)
-
Information on the patient's rights and on encouraging patient's participation in the treatment measures must be given.17
A new item is the introduction of a system to report and register critical incidents in order to provide an effective quality assurance for in and outpatient care. By these means a system of error prevention was established in 2011. To achieve this in 2009 both the BZÄK and KZBV instructed their Agency for Quality in Dentistry (Zentrum Zahnärztliche Qualität - zzq), a body which is run by both organisations, to prepare a pilot project on a reporting system for critical incidents. The Critical Incident Reporting System 'CIRS Dent – every tooth counts' started online in January 2012.
Discussion
Germany has the world's oldest national social health insurance system with its origins dating back to Otto von Bismarck's Sickness Insurance Law of 1883. Dental care has been part of the system since 1922, after the National Insurance Office (Reichsversicherungsamt) decided in 1917 that caries is a disease that required treatment.18 This development led to a Contract Code in 1935, which formed the collective contract basis for the provision of oral healthcare under the health insurance scheme following the creation of the German Association of Health Insurance Dentists as a public legal entity. In 1943, the cover provided by SHI funds was extended to include prosthodontic treatment as an optional benefit. Since World War II the range of dental treatment covered has constantly broadened.
Healthcare has long been considered to be too expensive and much effort has been put into reforming the system in Germany. Owing to the upward trend of expenditure in the SHI-system, especially in the hospital and pharmaceutical sectors, due to demographic trends, to changing morbidity patterns and to progress in medical science, legislative intervention in the contractual and remuneration structures of the SHI-scheme was repeatedly found to be necessary, from the 1970s onwards, in the form of a series of cost containment laws. The manifest signs of these legislative changes are the constantly changing rules for the provision of prosthetic treatment and a number of 'restructurings' of the SHI-assessment scale for dental treatments, with the aim of reducing orthodontic and prosthetic services.
The establishment of a so called Central Reallocation Pool or National Health Insurance Fund (Gesundheitsfonds) to collect and pool the money centrally to run the SHI and re-organising the national Federal Joint Committee to become the highest decision making body for insurance covered healthcare are fundamental reforms in the German social health insurance system in the past decade. After the 2005 elections, when the Christian Democratic Union and Social Democratic Party joined to form a grand coalition, the fund emerged as a compromise between two different fundamental reform models for health insurance. The Social Democrats had proposed a so called Bürgerversicherung ('citizen's insurance'), which is an income-based model for the whole population which would have expanded the mandatory health insurance requirement to additional population groups. Whereas the Christian Democrats suggested a concept of a capitation-based, uniform scheme for all social health insured citizens, ie a per capita payment (a so-called Kopfpauschale) combined with a fixed employer contribution based on an employee's gross wages. People unable to pay the premium would receive subsidies financed through general taxation. Consequently, the majority of self-governing professions have moved towards more concentrated governance structures, over the past decade. Thus, centralisation of the system has been the guiding principle.
The German Dental Association has been concerned about this shift of tasks and responsibilities – formerly at regional level and a responsibility of the dental profession - to the federal level and in the responsibility of the federal social legislative. In the Joint Federal Committee (Gemeinsamer Bundesausschuss), the SHI and the service providers (hospitals and general medical and dental practitioners) are equally represented. This Joint Federal Committee is charged with an increasing number of tasks which are regulated by compulsory guidelines, for example in matters of quality assurance, compulsory continuing education or patients' rights. The dental profession considers that the reforms mean additional bureaucratic structures and don't resolve the problems of the SHI. The Federal Government can control the Central Reallocation Pool directly through tax subsidies, whereas cost containment is a task for the sick funds themselves. Because of the complex responsibilities concerning patients' information and instruction as well as documentation, the dental profession fears that the consequence will leads to a further increase in bureaucratic work in their dental surgeries.
The rapid medico-technical progress and developing E-health-systems and IT networks will put further pressure on the dental profession and the demand for quality assurance is increasing.
In general, coronal caries is becoming less prevalent; the situation with respect to the prevalence of periodontitis is unclear. However, there appears to be under-treatment of people with periodontitis. Tooth loss among the adult population in Germany has decreased considerably. Overall the trends seem to be favourable. The oral health of children and adolescents has improved considerably since 1997, probably due to increased use of fissure sealants and regular check-ups.14 About 70% of 12 and 15-year-olds had at least one fissure-sealed tooth in 2005. Also oral health among working age adults has improved greatly and their treatment need has changed because they have more natural teeth. The majority of the population brush their teeth at least twice a day (IDZ 2006). Their oral health habits are generally good. A contributory factor to this could be that since 1990 sickness funds have offered insured persons a bonus payment to reduce the costs for prosthetic treatment if the patients visit a dentist at least once per year over a five and ten-year period.19
As in other countries, with well-functioning oral healthcare systems, more emphasis needs to be put on the elderly and special needs groups. To address this need, in 2010, the Federal Association of Statutory Health Insurance Dentists, the German Dental Association and the German Association of Geriatric Dentistry developed a proposal entitled Oral health despite handicap and old age with the objective of improving the oral health of people in need of care and of disabled people at a population level. At the beginning of 2012, a law was passed which can be regarded as the first step towards the implementation of this concept. A new item 'fees for visiting immobile patients' has been included in the scale of fees of the public sick funds. In addition, a new order regulating licences to practise dentistry is under development in which the first two years post-graduation will be nearly identical with those in medicine and the medical licensure act. This closer orientation towards medicine is reasonable as here are more patients with multi-morbidities and they will have a need for dental treatment in general dental practice and co-operation with physicians will be more frequent in the future.
The SHI-system of Fixed Grants established in 2005 as 'diagnosis-based fixed subventions' to all prosthodontic measures has been accepted by the people. For prosthetic dentistry, the patient receives a diagnosis-based fixed amount independent of his/her socio-economic status and independent of the treatment. It is fairer than the previous regulation, in which the treatment-based percentage co-payments paid depended on the income of the patient.
An increase of female graduates and female dentists has been observed. At present 42% dentists in practice are female. By 2017 it is expected that there will be more than 50%. In consequence of this and 'work-life-balance' it seems likely that there will be an increasing number of dentists working part-time and working as salaried personnel in bigger dental units.
After years of deliberations, a new scale of private dental fees (Gebührenordnung für Zahnärzte, GOZ) was adopted in November 2011 and came into force in January 2012. After 24 years, the out-dated scale of private fees no longer covered all dental services provided and therefore some new items were added to the list. The free choice of a practitioner by the patients was maintained. This was one of the objectives strongly and successfully supported by the dental profession against a strong opposition. Despite these successes, the new scale of private dental fees is not sufficiently orientated towards the state of science in dentistry and ignores the increases in the costs of materials and equipment over the last few years.
A prognosis for the future of the German health system is that demographic changes, medico-technical progress and the decreasing revenue of the SHI will make the system more expensive. In particular, if society wants to maintain the present high care standard, medical and dental fees will need to be linked with the quality of services. Patients will have to pay more than in the past for medical and dental services out of their own pockets – via insurance premium, taxes, additional contributions or flat rates.
References
EU (European Union) Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients' rights in cross-border healthcare. 4.4.2011: L 88/45L 88/65. Available at: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2011:088:0045:0065:en:PDF (accessed January 2015).
EU (European Union) Directive 2013/55/EU of the European Parliament and of the Council of 20 November 2013 amending Directive 2005/36/EC on the recognition of professional qualifications and Regulation (EU) No 1024/2012 on administrative cooperation through the Internal Market Information System ('the IMI Regulation'). 28.12.2013: L 354/132L 354/170. Available at: www.eaeve.org/fileadmin/downloads/sop/DIR_2013_55_EU_amended_rpq.pdf (accessed January 2015).
Data from the General Dental Council.
The Council of European Chief Dental Officers. Oral Health Database. www.cecdo.org (accessed on 24 September 2014).
Patel R, Eaton K A, Garcia A, Rincon V, Brooks J . An investigation into the numbers of dentists from 19 European Economic Area (EEA) member states currently registered to work in the United Kingdom and key differences between the practice of dentistry in the UK and their member states of origin. 2011; 211: 133137.
WHO. The changing national role in health system governance. A case-based study of 11 European countries and Australia. Jakubowski E, Saltman R B (eds). The European Observatory on Health Systems and Policies, 2013.
Busse R, Blümel M . Germany: Health system review. 2014; 16: 1–296.
Bundesministerium der Justiz und für Verbraucherschutz. SGB V (Social Security Code V) (1988). Gesetzliche Krankenversicherung (Artikel 1 des Gesetzes v. 20. Dezember 1988, BGBl. I S. 2477) last update 11 August 2014. Available at: www.gesetzeiminternet.de/sgb_5/BJNR024820988.html (accessed 2 September 2014).
Council of European Dentists. 5th ed. Brussels, February 2014. Available at: www.eudental.eu/library/eu-manual.html (accessed 2 September 2014).
BZAEK (Bundeszahnärztekammer – German Dental Association, ed.) (2013): Statistisches Jahrbuch BZÄK, 2012/2013, Berlin.
BMG (Bundesministerium für Gesundheit Federal Ministry of Health, ed.) (2013a): KJ1 und Fachserie 12, Reihe 7.1.2.
GKV (Statutory Health Insurance, SHI, ed.): KV 45, Finanzielle Entwicklung in der Gesetzlichen Krankenversicherung 1.4. Quartal 2012.
Patel R. The state of oral health in Europe. Report Commissioned by the Platform for Better Oral Health in Europe. September 2012. Available at: http://www.oralhealthplatform.eu/sites/default/files/field/document/A5-Summary-BOHEP_State%20of%20Oral%20Health_Executive%20Summary_A5_FINAL.pdf (accessed January 2015).
IDZ (Institute of German Dentists, ed) Fourth German Oral Health Study (DMS IV) - Present results on the prevalence of oral diseases, risk groups and the degree of dental care in Germany 2005. Materialienreihe, Vol. 31, Deutscher Zahnärzte-Verlag, Köln/Cologne.
Gesellschaft für Telematikanwendungen der Gesundheitskarte (gematik) (Organization for Telematics Applications of the Health Card) (2012). Für ein Gesundheitswesen mit Zukunft. Die elektronische Gesundheitskarte. Berlin, Gematik.
äzq (Ärztliches Zentrum für Qualität in der Medizin - German Agency for Quality in Medicine): Qualitätsanforderungen für Zahnarztbewertungsportale. German Dental Association, Federal Association of Statutory Health Insurance Dentists in cooperation with German Medical Association, Federal Association of Statutory Health Insurance Physicians and German Agency for Quality in Medicine, Berlin, February 2012. Available at: www.bzaek.de/fileadmin/PDFs/qualitaet/1105_bewertungsportale.pdf (accessed 2 September 2014).
BMG, BMJ (Bundesministerium für Gesundhei t Federal Ministry of Health, Bundesministerium der Justiz Federal Ministry of Justice, ed.): Informiert und selbstbestimmt Ratgeber für Patientenrechte. Berlin, June 2013.
IDZ (Institute of German Dentists, ed) The system of dental care in Germany. Materialienreihe 2003, Vol. 28, Deutscher Zahnärzte-Verlag, Köln/Cologne.
Klingenberger D, Micheelis W . Finanzielle Anreize im Gesundheitswesen - Bonusregelung auf dem Prüfstand. 2006; 96: 18–19.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Ziller, S., Eaton, K. & Widström, E. The healthcare system and the provision of oral healthcare in European Union member states. Part 1: Germany. Br Dent J 218, 239–244 (2015). https://doi.org/10.1038/sj.bdj.2015.95
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.95
This article is cited by
-
Dental caries at enamel and dentine level among European adolescents – a systematic review and meta-analysis
BMC Oral Health (2022)
-
Developments in oral health care in the Netherlands between 1995 and 2018
BMC Oral Health (2020)
-
The healthcare systems and provision of oral healthcare in European Union member states. Part 10: comparison of systems and with the United Kingdom
British Dental Journal (2019)
-
The healthcare system and provision of oral healthcare in European Union member states. Part 4: Greece
British Dental Journal (2016)