Key Points
-
Investigates a population (care home residents) not normally included in surveys of adult dental health surveys.
-
Considers a number of issues in relation to the provision of dental services for older adults.
Abstract
Aim To determine the oral health status of a sample of care home residents and provide data to inform local needs assessments and commissioning decisions.
Methods A stratified sampling methodology was used to sample care homes; residents were then selected at random and invited to participate. The survey consisted of a short questionnaire and a clinical examination; it attempted to capture data relating to current oral health status, treatment need and suitability for treatment.
Results Of 1761 residents sampled, 848 residents (mean age: 80 years) were competent to and consented to participate in the survey. Of those who consented to a clinical examination, 56% were dentate and 43.6% edentate. Among dentate residents, there was a caries prevalence of 55.8%. Just over half of examined residents (52.7%) were thought to be in need of dental treatment, and potentially suitable to receive treatment.
Conclusion These findings document the current state of oral health of a sample of care home residents in the West Midlands and provide valuable data to help inform strategic commissioning decisions. The particular oral health needs of this population group must be considered.
Similar content being viewed by others
Introduction
In 2010/2011, the NHS Dental Epidemiology Programme (now superseded by the Public Health England, Dental Public Health Intelligence Programme1) called for locally defined activities. In the West Midlands, it was agreed that the epidemiology survey would focus on care home residents. A combined methodology was adopted comprising of two separate components: a postal questionnaire survey of care home managers and a clinical survey of a sample of care home residents. The questionnaire survey has previously been reported in Part 1; this paper describes the clinical survey and findings.
This epidemiology survey should be of interest both to those commissioning and to those providing dental services; the findings provide some indication of both the level of need and the suitability for treatment by specialised and general dental services.
Background
Global demography is changing rapidly, with the world's elderly population now the fastest growing age group in most countries.2 As more people survive into later life, health and social care systems face the challenge of trying to provide appropriate services for this expanding population group. To facilitate the planning and commissioning of services, it is important to have a clear understanding of current health status and need.
The Adult Dental Health Survey (ADHS) has been carried out every 10 years since 1968 to establish the dental health status of the adult population in the UK.3 Epidemiological data provided by the ADHS is invaluable, but with the sampling framework for ADHS based on private households, it does not include residents of care homes.
With limited epidemiological data pertaining to the oral health of care home residents,4,5,6,7 the needs of this potentially vulnerable group of the population are poorly understood.
Aim
To determine the oral health status of a sample of care home residents and provide data to inform local needs assessments and commissioning decisions.
Objectives
-
Develop an appropriate methodology and sampling technique for a clinical epidemiology survey of care home residents
-
Pilot survey methodology and review methodology as appropriate
-
Deliver training for examiners and recorders
-
Sample care home residents in West Midlands and seek consent to participate in clinical survey
-
Conduct clinical examination, collecting data regarding number of natural teeth, condition of natural teeth and surrounding tissue, presence of any acute lesions, and the condition of any dentures
-
Collate and analyse the data
-
Write report and disseminate to relevant bodies and individuals.
Method
Advice was sought from the West Midlands Research Ethics Committee and review under the National Research Ethics Service scheme was deemed unnecessary. The methodology was piloted in a care home in Birmingham and a training day was then held for examiners. The protocol included a short questionnaire and a clinical examination. Only care homes which had responded to the initial questionnaire survey (of care home managers) were included in the sampling framework.
A stratified sampling methodology was designed, similar to that used in the regular surveys of child dental health.8 A power calculation was carried out and a sample size of 150 per upper tier local authority was decided upon. Residents in the sampled care homes were selected at random and invited to participate. Positive consent was required. Only residents able to consent for themselves were able to participate. No data was captured for those unable to consent or those who did not wish to consent; the numbers of those unable to consent were, however, included in the data analysis at a later stage to allow for more meaningful interpretation of the data in relation to service need.
Data was captured on paper forms and then transferred to Dental Survey Plus 2 (DSP2).9
Results
Participation
Fifteen out of 17 PCTs in the region (14 upper tier local authorities) participated. Of 1,832 care homes identified, 1,170 responded to the initial postal survey and were included in the sampling framework for this clinical survey. Sampling of the care homes took place locally according to an agreed protocol; 139 agreed to participate.
Consent
Of 1,761 residents sampled, 815 (46.3%) consented to participate in the clinical examination, 211 (12.0%) did not wish to consent and 702 (39.9%) were unable to consent. A small number of residents wished to participate in just the questionnaire survey (33) and a small number only wanted to participate in the clinical survey (12).
Characteristics of sample
A total of 848 residents (280 male, 568 female) consented to participate in one or both elements of the survey. Mean age was 80 years (range 21 – 103) (median–85, mode–90). Over half the residents (52.5%) were aged 85 and over. The majority (96.3%) were reported to be 'white British'.
Questionnaire results
A total of 836 residents consented to participate in the questionnaire. Just under a third (31.7%) thought they needed to see a dentist. Of the 221 residents who reported having tried to get a dental appointment within the last six months, the majority (87.8%) were successful.
A number of questions were adapted from the Oral Health Impact Profile (OHIP), to measure the extent to which residents felt their oral health had affected their general health and wellbeing over the last 12 months.10,11 The questions were answered as follows (n = 836; answers not mutually exclusive):
-
6.5% reported that they had had trouble pronouncing words because of problems with their teeth, mouth, or dentures.
-
16.9% reported that they had had painful aching in their mouth.
-
12.6% reported that they had found it uncomfortable to eat certain foods because of problems with their teeth, mouth, or dentures.
-
18.1% reported that they had been self-conscious because of their teeth, mouth, or dentures.
-
11.5% reported that they had had to interrupt meals because of problems with their teeth, mouth, or dentures.
Clinical examination results
A total of 815 residents consented to a clinical examination. During the survey, some residents, who had consented to a clinical examination, may have been unable to be examined at a particular stage; throughout this report, figures are therefore given for the number who participated at that stage of the examination. Of those who consented to a clinical examination, 456 (56%) were dentate and 355 (43.6%) edentate; four participants were unable to be examined at this stage. Table 1 displays the proportion of dentate and edentate participants by age band. Examiners were asked to count crowns, implants, bridge abutments and bridge pontics as teeth; a tooth was recorded as being present if any part of it was evident, including a fragment of retained root.
The mean number of teeth among all examined dentate residents was 16 (SD 8) (range 1–32). Analysis by age band showed that dentate participants aged 85 and over had on average 14.1 teeth whereas those aged 65–84 had an average of 14.5 teeth and those aged 64 and younger had 21.5 teeth on average.
Just over a third (33.8%) of examined dentate residents had 21 or more teeth.
Caries
Of 456 dentate residents, three were unable to be examined for caries. 253 of 453 examined dentate individuals (55.8%) had one or more carious teeth; 200 (44.2%) were reported to be caries free. Those with carious lesions had a mean of 3.6 teeth (SD 3.3) affected (range 1–18). Of the 253 residents who had carious teeth, 124 (49%) had just one or two carious teeth.
Gingival condition
Gingival condition was recorded as 'pink and healthy' in 172 (37.9%) of the 454 dentate residents who participated in this examination; it was recorded as 'red' in 234 residents (51.5%) and 'red with obvious bleeding' in 48 individuals (10.6%).
Dentures
Just over half (51.3%) of the 813 residents who participated in this part of the examination wore dentures. 277 residents (34.1%) wore upper and lower dentures, 132 residents (16.2%) wore just an upper denture and eight residents (1%) wore just a lower denture.
Pain/problems
A proportion of residents (10.8%) reported pain or problems in their mouth, but the majority said they were not experiencing any discomfort.
PUFA
PUFA provides a measure of diseased and broken down teeth which have been affected by caries and are causing significant problems.3 A positive PUFA score, usually indicative of untreated sepsis, was recorded in 69 (15.2%) of the 454 dentate residents examined.
Treatment need
Examiners were asked to assess treatment need objectively, without taking into account the resident's suitability for treatment; they were then asked to decide what treatment they felt it might actually be appropriate to provide for this particular individual, in the context of their general health and the likely difficulty of providing dental treatment.
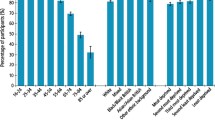
The treatment perceived to be most needed was denture work, reportedly required by almost half (49.6%) of examined residents. Periodontal treatment was said to be required by 34.9% of residents, restorative work by 21.3% of residents and oral surgery treatment by 21.3% of residents.
Table 2 displays the proportions of residents in need of treatment and Table 3 shows the proportion of those in need of treatment for whom treatment may be appropriate.
Just over half (52.7%) of the 799 residents, for whom this question was fully answered, were reported to be in need of some form of treatment and potentially suitable for treatment.
Communication and cooperation
A modified version of the British Dental Association (BDA) case mix tool was used to assess each resident in terms of their ability to communicate and cooperate in order to provide some indication of the likely difficulty of treating this population group.12
Residents were categorised as shown in Table 4. The table has been annotated to indicate the varying levels of cooperation and communication.
Just over half of examined residents (51%) were reported to be capable of free communication with adequate understanding between resident and examiner. In terms of levels of cooperation, the majority of residents (60.5%) were able to cooperate fully and allow an examination to take place without significant restriction. A small percentage (3.8%) displayed severely restricted communication skills and/or were unable to cooperate.
Oral risk factors
Reported frequency of tooth-brushing is detailed in Table 5.
The majority (76.1%) of survey participants were reported to be brushing their teeth once or twice a day; 18.9% reported less frequent brushing.
Mobility status of residents
Residents were asked if they normally walked unaided, used a stick/zimmer frame, required assistance from others, used a wheelchair or were confined to bed. Two thirds of the participants (67%) were recorded as being able to walk unaided or using a stick/zimmer frame.
Need for domiciliary care
Just under 40% of participants in the clinical examination were reported by examiners to require domiciliary services, if care was needed. Common reasons given included 'severe medical problems', 'significant difficulties with mobility' and 'very confused and distressed'.
Additional reasons given for residents requiring domiciliary care included 'difficulty in finding a surgery with wheelchair access', 'unavailability of staff/family to escort to clinic' and 'need a hoist'. These issues relate to availability of services (or perceived lack of availability) rather than the patient's own need for domiciliary care. They are included here for completeness, but do not reflect a true need for domiciliary care.
Discussion
This study describes the oral health status of a sample of West Midlands care home residents and, in conjunction with the postal questionnaire survey of care home managers, provides valuable data to help inform local commissioning decisions.
Just under half (48.2%) of those sampled consented to participate in one or both elements of the survey, with 815 individuals consenting to the clinical examination. It is important to note, however, that a further 39.9% were unable to consent for reasons of capacity as defined by the Mental Capacity Act – this issue (highlighted in another survey undertaken at the same time13) is an indicator of the potential difficulties of providing care for this population group.
Oral health status
Of those who consented to having a clinical examination, 43.6% were edentate. This is considerably higher than the figure of six percent reported for the general adult population in the 2009 ADHS, however, given the age of this sample, this is unsurprising. The recent Welsh survey reported that 58% of care home residents examined were edentate.14 However, the Welsh survey included residents without the capacity to consent and it may be assumed that these individuals will face further barriers to good oral health. The proportion of edentate adults in our sample increased with age; 13.1% of those aged 64 and younger were edentate compared to 53.4% of those aged 85 and over. The results of the ADHS survey demonstrate a similar trend with 47% of adults aged 85 and over edentate. With increasing proportions of younger adults now retaining their teeth, it is important to remember that the next generation of care home residents may display different patterns of disease experience. Prevention will become increasingly important as the number of dentate older adults increases. Furthermore, there will be an ongoing need to maintain complex dentitions.
The mean number of teeth among dentate residents in this survey was 16 compared to 25.7 in the ADHS.3 Age specific analysis shows greater similarity; in the 85 and over age group, dentate care home residents had 14.1 teeth on average compared to a mean of 14 in the general population. It is important to note that in this survey, examiners were asked to count crowns, implants, bridge abutments and bridge pontics as teeth whereas the ADHS results reflect the number of 'natural teeth'.3
Over half (55.8%) of the examined dentate individuals had one or more carious teeth; those with carious lesions had on average 3.6 teeth affected. By comparison, the ADHS reported that 31% of adults had obvious caries and those with caries had 2.7 teeth affected on average.3
In our survey, a positive PUFA score was recorded in 15.2% of examined dentate residents compared to seven percent of dentate adults among the general population.3 This may well reflect the higher prevalence of caries in the care home residents.
Treatment need
A proportion of residents 'objectively' assessed as being in need of treatment were reported not to be suitable for treatment. A total of 421 residents (52.7% of 799) were thought to be in need of some form of treatment and potentially suitable for it. The limitations of this assessment of treatment need must be acknowledged. As no medical history details were collected by the examiners, thorough consideration of suitability for treatment was not possible. For the purposes of service planning, however, this crude assessment of suitability gives an indication of the proportion of this population who may feasibly undergo treatment. It is worth noting that normative need was reported to be higher than residents' perceived need – in the questionnaire part of this survey just 31.7% of residents reported that they thought they needed to see a dentist. This is an important factor to be considered alongside service provision for this particular patient group; strategies to encourage dental attendance may be needed.
Access to dental services
The vast majority (87.8%) of those who had tried to get a dental appointment in the last six months had been successful. The question did not differentiate between domiciliary appointments and appointments in a clinic; it is therefore possible that some of those who reported that they were unsuccessful in getting an appointment may have expected a domiciliary visit and were unable to arrange one.
While some care home residents may require domiciliary visits, it is often more appropriate for individuals to be seen in a dental clinic, if at all possible. It is important that this is clearly communicated to care home residents and staff. It should be particularly noted that 67% of the residents asked reported being able to walk unaided or using a stick/zimmer frame; however, just under 40% of participants in the clinical examination were reported by examiners to require domiciliary services, if care was needed. This discrepancy between residents' reporting and examiner assessment should be investigated further in future research.
Risk factors
In the 2009 ADHS, 75% of adults were reported to be cleaning their teeth twice a day and a further 23% cleaning their teeth once a day. Care home residents fare less favourably with just under 40% of dentate residents reportedly brushing their teeth twice a day, and a similar proportion brushing once a day. Department of Health guidelines recommend twice daily brushing for effective caries prevention.15 This suggests there is a need for evidence-based oral hygiene advice to be provided to care home residents and staff. In addition, with relatively high-sugar diets common among care home residents, advice about healthy eating, including the need to restrict the frequency of sugar intake, may be particularly beneficial.
Communication and cooperation
This survey aimed to gather data to inform local commissioning decisions. While the oral health epidemiology data is important, it alone is not sufficient. To help determine appropriate service provision for this particular population group, it is essential to have an understanding of their capacity to communicate and cooperate with treatment. Many (44%) of those who participated in the clinical examination were reported to be able to communicate freely and cooperate fully. The remaining participants were recorded as having difficulty with communication and/or cooperation to varying degrees. It is important to remember that many, if not all, those residents who were unable to consent to participate in the survey are likely to fall into this category of being unable to cooperate and/or showing severely restricted communication skills.
Table 4 (Results section) has been annotated to demonstrate the varying levels of cooperation and communication. In broad terms, the different annotations in this table may correlate with the type of dental services required. Those residents represented by annotation a may be suitable for treatment by GDPs, whereas residents represented by annotation c are likely to require the services of those with greater expertise in special care dentistry. If those residents who were unable to consent are considered with those who participated in the survey, the proportion of residents represented by annotation c rises to 48.4% (734/1,517) with 15.5% represented by annotation b (235/1,517) and 36.1% (548/1,517) represented by annotation a.
Although every attempt has been made to collect and analyse data in a valid and meaningful way, caution must be exercised in interpreting the findings. Above all, it is essential to remember that the clinical results presented above relate only to those who were able to give consent and chose to do so. Therefore, a large proportion of the sample was excluded from the clinical examination.
Conclusion
These findings document the current state of oral health of a sample of care home residents in the West Midlands and provide valuable data to help inform local needs assessments and commissioning decisions. Unmet need among care home residents has been demonstrated by a caries prevalence of 55.8%. A considerable number of these individuals were deemed to have the capacity to communicate and cooperate readily with treatment and were not necessarily in need of specialised services. However, the oral health needs of those who did not have capacity to consent may well be different. The particular oral health needs of this population group must be considered by those with responsibility for commissioning dental services.
References
Rooney E, Perkins C . NHS dental epidemiology programme for England. Report June 2010. NHS, 2010. Available online at http://www.nwph.net/dentalhealth/reports/NHS_Dental_Epidemiology_Programme_for_England_Report_June_2010.pdf (accessed September 2015).
World Health Organization. 10 facts on ageing and the life course. Available online at http://www.who.int/features/factfiles/ageing/ageing_facts/en/index.html (accessed September 2015).
The Health and Social Care Information Centre. Adult Dental Health Survey 2009. Available online at http://www.ic.nhs.uk/statistics-and-data-collections/primary-care/dentistry/adult-dental-health-survey-2009--summary-report-and-thematic-series (accessed September 2015).
Sweeney M P, Williams C, Kennedy C, Macpherson L M, Turner S, Bagg J . Oral health care and status of elderly care home residents in Glasgow. Community Dent Health 2007; 24: 37–42.
Ghezzi E M, Ship J A . Systemic diseases and their treatments in the elderly: impact on oral health. J Public Health Dent 2000; 60: 289–296.
Ferro R, Besostri A, Strohmenger L et al. Oral health problems and needs in nursing home residents in Northern Italy. Community Dent Health 2008; 25: 231–236.
Samson H, Strand G V, Haugejorden O . Change in oral health status among the institutionalized Norwegian elderly over a period of 16 years. Acta Odontol Scand 2008; 66: 368–373.
Pine C, Pitts, N B, Nugent Z J . (1997) British Association for the Study of Community Dentistry (BASCD) guidance on sampling for surveys of child dental health. A BASCD coordinated dental epidemiology programme quality standard. Community Dent Health 1997; 14 (Suppl. 1): 10–17.
University of Dundee Applied Computing, Dental Survey Plus Version 2. University of Dundee, Dundee. Computer Software.
Slade D G, Spencer A J . Development and evaluation of the Oral Health Impact Profile. Community Dent Health 1994; 11: 3–11.
Locker D, Allen F . What do measures of 'oral health-related quality of life' measure? Community Dent Oral Epidemiol 2007; 35: 401–411.
Bateman P, Arnold C, Brown R et al. BDA special care case mix model. Br Dent J 2010; 208: 291–296.
Shah K K, Tabari E D . Challenges encountered when conducting a dental health needs assessment of older people resident in care homes: experiences from England. Community Dent Health 2013 30: 6–9.
Johnson I, Morgan M Z, Monaghan N P, Karki A J . Does dental disease presence equate to treatment need among care home residents? J Dent 2014; 42: 929–937.
Public Health England (2014). Delivering Better Oral Health - an evidence-based toolkit for prevention - third edition. Available online from https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention#history (accessed September 2015).
Acknowledgements
The authors would like to thank the West Midlands care home residents, managers and staff who participated in the survey, the West Midlands dental epidemiology leads who carried out the survey, Janet Clarke MBE, Clinical Director, Birmingham Community Healthcare NHS Trust, Rebecca Willis, Senior Community Dentist in Special Care Dentistry, Birmingham and the West Midlands consultants in dental public health for their valuable expertise in developing the survey.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Tomson, M., Watson, F., Taylor-Weetman, K. et al. West Midlands Care Home Dental Survey 2011: Part 2. Results of clinical survey of care home residents. Br Dent J 219, 349–353 (2015). https://doi.org/10.1038/sj.bdj.2015.758
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.758
This article is cited by
-
The prevalence of denture loss within community residential settings
British Dental Journal (2024)
-
uSing rolE-substitutioN In care homes to improve ORal health (SENIOR): a study protocol
Trials (2022)