Key Points
-
Discusses the rationale and indications for a combined orthodontic and orthognathic approach, in accordance with the recently introduced assessment of treatment need.
-
Provides a detailed account of the orthognathic patient journey, including the key stages of planning, orthodontic preparation, finishing and surgical approaches.
Abstract
Orthognathic treatment is a process which involves orthodontics and maxillofacial surgery and is used to treat those dento-facial discrepancies which are outside the scope of conventional orthodontic treatment, for example severe Class II or Class III problems, anterior open bites and facial asymmetries. Patients who present with these severe problems may encounter a wide range of different problems ranging from functional problems (for example, difficulties biting and chewing) to self-consciousness in a wide range of work and social situations. This paper discusses the possible indications for orthognathic treatment and looks at the risks and benefits of treatment. The treatment pathway is also described.
Similar content being viewed by others
Introduction
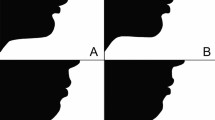
Orthognathic treatment is a treatment process which involves orthodontics and maxillofacial surgery, and it is used to treat those dento-facial discrepancies which are outside the scope of conventional orthodontic treatment. Treatment may be used to correct a wide range of different underlying skeletal discrepancies, including severe Class II or Class III problems, anterior open bites, markedly increased overbites and facial asymmetries (Figs 1,2,3).
The first description of a surgical procedure to correct a malocclusion was in 1849 in the USA1 and significant advances in surgical procedures, fixation, and imaging have led us to the situation we have in 2015 where severe dento-facial problems can be corrected in a relatively safe manner with high quality, stable outcomes. In 1990, Proffit and White2 estimated that there were over a million potential orthognathic patients in the USA and if this figure is extrapolated to the United Kingdom, there may be up to a quarter of a million patients who would benefit from orthognathic treatment.3,4
Indications for orthognathic treatment
The impact of having a dento-facial discrepancy may be considerable; ranging from problems biting and chewing to self-consciousness in a wide range of work and social situations,5 teasing/bullying6,7 and avoidance of situations where the individual may be concerned that any of these effects could occur. The effects may occur throughout life; often starting at school, but continuing into adulthood and adversely affecting many different aspects of life. Qualitative research by Ryan and colleagues5 discussed how patients reported a '...general feeling that life was more difficult and may have turned out differently if they had not been affected in this way, that they had an additional hurdle to jump or a 'millstone' around their neck.'
It is often assumed that the more severe the dento-facial problem, the more severe these associated effects, but this is not necessarily the case. Indeed some researchers noted that individuals who have obvious facial problems tend to be treated with compassion, whereas those with lesser problems (for example, an increased overjet) are more likely to experience negative effects such as teasing.8,9
It therefore possible to see why patients may seek correction of their dento-facial problem and the main motivating factors appear to be aesthetics, function, and psycho-social well-being/quality of life.5,10,11,12,13,14,15
Aesthetics
Recent years have seen advances in our views on dental and facial aesthetics and it is now accepted that individuals may wish to improve aspects of their teeth and face which cause significant concern in a whole range of educational, work, and social situations.
Function
Functional problems, including biting, chewing and the potential risk of future dental problems, motivate many patients to seek orthognathic treatment.16,17,18,19,20 In a systematic review of the literature between 2001 and 2009, 33–60% of individuals reported functional problems as the motivation to undergo treatment.20
There are less common situations, such as the management of obstructive sleep apnoea (OSA), where orthognathic treatment has an important role to play and the benefits of this form of treatment in OSA will be discussed further in the paper. There have also been suggestions that orthognathic treatment may enhance speech or alleviate temporomandibular joint dysfunction; however, there is little evidence that this is the case and patients should be counselled that such effects are unlikely.
Psycho-social well-being and quality of life
In today's society, there is little doubt that dento-facial aesthetics matters and that those individuals with dento-facial problems may be perceived differently and experience poorer quality of life (QoL) as a result of this. The World Health Organisation (WHO) constitution defines health as 'A state of complete physical, mental, and social well-being not merely the absence of disease...'. They highlight that the measurement of health and the effects of healthcare must include not only an indication of changes in the frequency and severity of symptoms but also an estimation of well-being and quality of life.21
In view of this, it is not surprising that the orthognathic literature includes a large number of studies describing the negative effects associated with dento-facial discrepancies and the resultant improvement in quality of life and psycho-social factors following treatment.5,14,20,22,23
The orthognathic treatment journey
A multi-disciplinary team approach to care
Successful management of complex dento-facial problems, which are outside the scope of conventional orthodontic treatment, requires a multi-disciplinary team (MDT) approach and the typical patient journey in the United Kingdom commences following the patient's referral to a hospital-based consultant service from either their general dental practitioner or a specialist orthodontist (Fig. 4).
If the initial consultation suggests that an orthognathic approach is appropriate, a preliminary discussion with the patient takes place, records are obtained and patients are provided with the relevant information leaflets. Patients are currently assessed and prioritised for treatment need based on the newly introduced and validated index, the Index of Orthognathic Functional Treatment Need (IOFTN).24
The patient is then subsequently seen on the MDT clinic to determine the most appropriate treatment plan. The main team members are the orthodontist and the oral and maxillofacial Surgeon, with restorative dentists also playing an important role. Supporting access to a psychologist/psychiatrist and speech and language pathologist in specialist centres (for example, cleft or craniofacial teams) is also important. The purpose of this first appointment at the MDT clinic is to allow the patient to discuss their concerns and for the team to present the proposed treatment plan. The details of precisely what the plan will entail, including the risks and benefits, are explained. Specific discussions regarding the following elements of treatment take place:
-
Any dental treatment required before orthognathic treatment can commence for example, restorations, periodontal treatment, orthodontic extractions
-
Pre-surgical orthodontic treatment with an approximate duration of 12–24 months25
-
Need for follow-up MDT clinic attendances
-
Orthognathic surgery, followed by a recuperation period of approximately 4–6 weeks
-
Post-surgical orthodontics with a duration of approximately 5–11 months.26 It is important to ensure that patients are made aware of the timescales involved as some patients find the duration of orthodontic treatment difficult, especially following surgery.27
Patient records
A minimum dataset for orthognathic patients has been jointly agreed between the British Orthodontic Society (BOS) and the British Association of Oral and Maxillofacial Surgeons (BAOMS) to help rationalise which records are needed during orthognathic treatment.28 These include:
-
Study models
-
Standard extra-oral and intra oral photographs
-
Radiographs (panoramic and lateral cephalograph and sometimes a postero-anterior cephalograph if the patient has an asymmetry).
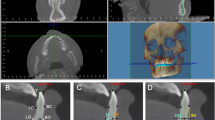
A detailed cephalometric analysis is undertaken to help quantify the extent of the skeletal/jaw discrepancy and the amount of dental tipping which has taken place in an attempt to 'mask' some of the underlying jaw malposition, known as dento-alveolar compensation. Numerous computer analyses are available, to aid decision making and to illustrate treatment options available. The programmes available have advanced significantly in recent years, now also permitting 3-dimensional (3D) imaging analysis. A number of studies have evaluated the accuracy of digitisation and validity of computerised prediction of surgical outcome and found them to be reliable at identifying cephalometric points but caution must be exercised in relation to the actual surgical predictions as there is wide inter-individual variation.29,30,31 Furthermore, in situations involving more complex malocclusion a 3D facial construction model can be utilised to help plan management.
Orthodontic preparation for surgery
The objectives of pre-surgical orthodontic treatment are:
-
1
Dental decompensation: The patient's soft tissues naturally attempt to mask the underlying skeletal discrepancy, through varying degrees of dental tipping, and this can be observed in all three planes of space (in the antero-posterior, transverse and vertical planes). In the antero-posterior plane, the teeth naturally tip towards one another in an attempt to reduce the disrepancy; for example, in a skeletal Class III pattern the lower incisors retrocline, while the upper incisors procline towards one another, thereby reducing the extent of the negative overjet. This is known as dental compensation. Orthodontic decompensation aims to reverse this process and thus involves moving the teeth back to their 'normal' inclination, that is, in the previous Class III skeletal example, proclination of the lower incisors and retraction of the upper incisors moves the teeth into their ideal position and, in turn, increases the reverse overjet (Fig. 5). Similarly, dental compensation can be observed in Class II patients, correction of which is also required during pre-surgical orthodontics (Fig. 6).
Figure 5: Class III Pre-surgical orthodontic decompensation. In this Class III patient, the lower incisors were retroclined and the upper incisors proclined initially. Pre-surgical orthodontics has corrected the incisor inclinations, resulting in an increased reverse overjet. This in turn facilitates maximum skeletal correction. [NB Images are not for reproduction.]
Figure 6: Class II Pre-surgical orthodontic decompensation. -
2
Relief of dental crowding and arch alignment: Fixed appliances are required to achieve optimal dental alignment. While dental extractions are often a solution to crowding in non-surgical orthodontic patients, a different and often opposite approach is necessary for patients requiring an orthodontic-surgical approach. This is well illustrated in the comparison of the management of a typical Class III routine orthodontic patient, in whom the planned extraction pattern would often necessitate extractions in the lower arch, to retract the lower labial segment and ideally a non-extraction approach in the upper arch to maintain proclination of the upper incisors. In contrast, in orthognathic treatment, a non-extraction approach is often adopted for the lower arch, allowing maximum decompensation of the lower incisors and an extraction approach in the upper arch to allow retraction of the upper incisors.
-
3
Dental arch coordination: The dental arches should coordinate with one another at the time of surgery, permitting maximum intercuspation post-operatively. Thus, the pre-treatment study models are articulated to identify any need for dental expansion before definitive surgery. The necessary expansion can be undertaken using orthodontic appliances such as the archwires themselves, a quadhelix or rapid maxillary expansion device. Where a significant maxillary transverse discrepancy is present, consideration may need to be given to surgical correction, using either surgically assisted rapid palatal expansion (SARPE) or segmenting and expanding the maxilla at the same time as the Le Fort I osteotomy.32
Pre-surgical MDT clinic review
All patients are reviewed again in the MDT clinic before surgery to assess that the orthodontic preparation has been achieved and to agree the planned surgical correction. This is achieved by reviewing the patient and the records simultaneously:
Orthodontic preparation
Prior to the patient being seen on the pre-surgery MDT clinic, the orthodontist will ensure the planned tooth movements have been achieved and the patient is in final rigid stainless steel archwires (Fig. 7). Most commonly, a number of crimpable hooks are attached to these archwires providing a means of elastic fixation during surgery and also allowing the use of post-surgery guiding elastics. Up-to-date study models are obtained to reflect the pre-surgical tooth positions and a set of study casts is mounted on either a plane or semi-adjustable articulator, depending on whether a mandibular or bimaxillary procedure is to be performed. The latter is facilitated by undertaking a facebow record. For patients requiring mandibular surgery only there is no major perceived benefit in undertaking a facebow record. However, this is necessary for patients planned for maxillary surgery, as autorotation of the mandible will occur and therefore requires either restoration of the occlusal plane in the case of maxillary jaw surgery only or to help establish an intermediate inter-occlusal relationship for bimaxillary procedures. In addition, full photographs and up-to-date radiographs (panoramic and lateral cephalograph) are obtained.
7a (i and ii) Start of treatment. 7b (i and ii) Following completion of pre-surgical orthodontics, the increased reverse overjet is apparent. 7c (i and ii) Post-surgical orthodontics and finishing, with inter-maxillary elastics being utilised for settling and to aid occlusal interdigitation. 7d (i and ii) End of treatment dental views. [NB Images are not for reproduction.]
Surgical planning
The type of surgery required is considered carefully for each individual patient and is dependent on the type and severity of the skeletal discrepancy; the soft tissue 'drape'; and the plane of space affected (that is, antero-posterior, vertical and/or transverse). There is no magic formula to allow the decision to be made. Correction may require a single jaw procedure, where just the maxilla or mandible is moved, or a bimaxillary procedure in which both jaws are moved. In a Class II patient where the problem is primarily mandibular retrognathia, correction will often involve a mandibular advancement only (Fig. 1), provided it is less than 10 mm. Some Class III patients may also be treated with a single jaw procedure (for example, a maxillary advancement); however, many Class III patients require bimaxillary surgery to ensure the best facial balance. Malocclusions where there is an anterior open bite discrepancy also bimaxillary procedures, usually incorporating a differential posterior impaction of the maxilla, to allow closure of the open bite.
Inter-occlusal wafers
Inter-occlusal wafers are a fundamental part of orthognathic planning and the support of an experienced technician and laboratory are essential to the success of this stage of treatment. The main use of the wafers is to assist the surgeon in accurately placing the teeth and jaws into the planned surgical position. Some clinicians leave the wafers in position at the end of the surgical procedure whereas others clinicians remove them. Wafers may be useful post-operatively in aiding the patient into their new jaw position as they may find it difficult to adapt to the new occlusion as a result of numbness and/or loss of proprioception. The use of elastics, with or without (Fig. 7) the wafer, often helps at this stage.
Post-surgical orthodontics
Immediate post-surgical phase
Jaw fixation following an osteotomy plays a crucial role in promoting the union of the repositioned segments and any movement can impair healing, which may result in a fibrous union, non-union or mal-union. Fixation is usually by direct rigid internal fixation using plates and/or screws (Fig. 8). Inter-maxillary wiring fixation is occasionally still used but necessitates a liquid diet during the healing period.
Fedorowicz et al.33 reported the findings of a Cochrane review showing no statistically significant difference in post-operative discomfort, level of patient dissatisfaction, plate exposure or infection for plate and screw fixation using either titanium or resorbable materials in orthognathic surgery.
Following surgery, the orthodontist may see the patient the following day on the ward and also arranges a series of weekly appointments to closely monitor the occlusion and to provide pastoral care and support to their patient. As stated above, intra oral elastics are often used during this early healing phase to help guide the teeth into the planned occlusion. Their pattern of placement, duration and force levels applied depends very much on clinical need and is assessed on an individual basis.
Finishing orthodontic procedures
The final post-surgical phase of orthodontics is concerned with optimal detailing of the occlusion and most frequently entails the orthodontic closure of lateral open bites. Figure 7 shows the treatment sequence in a patient with a skeletal Class II discrepancy. A number of procedures can be employed to help settle the buccal occlusion including sectioning the working archwire in the buccal segments and application of vertical inter-maxillary elastics to achieve differential extrusion, or the use of a flexible archwire in one arch and a rigid stainless steel wire in the other arch, with vertical inter-arch elastics. While, this phase of treatment should be kept to a minimum timeframe, Luther et al.26 demonstrated that a realistic estimate would be 6–9 months of post-surgical orthodontic treatment before the appliances are removed and retainers placed.
Outcomes of orthognathic treatment – benefits, risks and long-term stability
Measuring outcomes of treatment has become a particularly important aspect of medical care since the publication of the Darzi Report in 2008, with an increasing emphasis on patient reported outcome measures (PROMs) for assessment of quality.34 In a time of limited funds it is also important to consider the benefits of such interventions, for patients themselves and also for whoever is funding the treatment (whether this is a health service/insurance system or whether treatment is self-funded). It is, however, always difficult to undertake research where the treatment is longitudinal and can easily take 2–2.5 years to completion.
Benefits
In terms of benefits, the literature provides evidence of enhanced facial and dental aesthetics, quality of life (QoL), and oral function. Additionally, it is a treatment which is associated with low morbidity and high levels of satisfaction. From a funding viewpoint, the treatment has also been shown to be cost effective with long-term benefits.
Psycho-social changes and quality of life
Psycho-social changes and changes in quality of life are important aspects of orthognathic intervention which accompany improvements in facial/dental aesthetics and function.
A large number of studies have looked at QoL and shown improved oral health related quality of life following orthognathic treatment.35,36,37 There are also several high quality systematic reviews of the literature which illustrate that orthognathic patients experience significant psycho-social benefits following treatment, including improved self-confidence, body image and social adjustment.20,38,39
Function
Changes in function are difficult to measure objectively and are usually assessed using self-report questionnaires. While acknowledging the limitations of this type of research, improved biting and chewing have been reported in the literature. One of the early studies to look at this aspect was that undertaken by Kiyak and colleagues27,40,41 in Seattle who showed that patients reported significantly fewer functional concerns at 24 months post-surgery than before. A more recent study by Øland et al.42 assessed function pre- and one-year-post-surgery in 118 orthognathic patients and 47 matched controls, and found that function was greatly improved following orthognathic treatment. They concluded that orthognathic treatment improves oral function in most cases.
Research has shown that certain malocclusions affect biting and chewing more than others. Hunt and Cunningham16 found that patients with increased vertical facial dimensions had significantly poorer bite forces than normal before treatment and function improved to normal levels following orthognathic treatment. It must, however, be noted that these changes can take a significant period of time, for example, Magalhaes et al.43 found that it could take up to 5 years for the positive effects to occur.
The role of orthognathic treatment in obstructive sleep apnoea/hypopnoea syndrome (OSAHS) was mentioned earlier in the paper. Vicini et al.44 demonstrated significant clinical improvements in the two assessment parameters for OSAHS following orthognathic treatment; and this treatment was also shown to be as effective as continuous positive airway pressure (CPAP), the gold standard treatment modality. A systematic review and meta-analysis of the literature by Holty and Guilleminault45 showed that most patients reported improved quality of life and symptoms following maxillomandibular advancement surgery undertaken to treat sleep apnoea. However, long-term follow-up was lacking.
Satisfaction with treatment
It is perhaps not surprising that orthognathic treatment which changes the structure, function and appearance of the face/mouth and enhances QoL in the majority of patients is associated with high levels of satisfaction. The literature shows that between 92% and 100% of patients are satisfied with the results of orthognathic treatment46,47,48,49 and also highlights that where dissatisfaction does occur it is often related to problems with communication rather than adverse physical treatment outcomes. When patients present initially for treatment, the potential for dissatisfaction with treatment, even when results are technically good, is discussed with them, although fortunately this is not a common occurrence.
The British Orthodontic Society (BOS) and British Association of Oral and Maxillofacial Surgery (BAOMS) work together to ensure outcomes are measured in orthodontic/maxillofacial units throughout the UK and a large number of UK audits have been undertaken, with satisfaction for outcome and process of treatment standing at over 90% in a large number of these audits.
Cost-effectiveness
In any healthcare system, it is important to consider the cost-effectiveness of medical and dental procedures. Cunningham et al.50 undertook a study to assess the cost per quality adjusted life year (QALY) gained and found that treatment provides good outcomes at relatively low cost. The cost per QALY was considerably below the threshold set by the UK National Institute for Clinical Excellence (NICE) as being appropriate for the National Health Service to fund. This may be partly explained by the fact that patients are usually relatively young when they undergo treatment and therefore accrue benefits over a long time period. Interestingly, resource use has been shown to be similar in other studies.51
Risks
There are clearly risks associated with any medical or dental intervention and orthognathic treatment is no different. Risks of treatment include those associated with orthodontic intervention and those associated with the surgery.
Orthodontic risks/disadvantages
There are some associated risks which are inherent in any orthodontic treatment and include, for example, root resorption, decalcification if the oral hygiene is not maintained at optimal levels, and periodontal problems (such as recession).52 Additionally, the need for long-term retention should be clearly explained to patients.
Surgical risks
Surgical risks include those risks associated with general anaesthesia, pain, swelling, infection, and damage to the inferior dental nerve potentially leading to temporary or permanently altered sensation. The incidence of permanently altered sensation due to inferior dental nerve damage is usually quoted around 10%. Recent studies have highlighted the relatively low risk of surgical complications. For example, Sousa and Turrini53 undertook a comprehensive literature review of complications in orthognathic surgery and noted the following complications: nerve sensory changes (12.1%), infection (3.4%), fixation problems (2.5%), TMJ pain (2.1%) and unfavourable direction of fracture (1.8%). Ianetti et al.54 reviewed 3,236 patients and noted reversible sensory lip deficit in 19% of patients but irreversible sensory deficits in only 2% of patients. A similar incidence of infection was noted as in the Sousa and Turrini53 study, at 2%.
Fortunately, serious complications are rare in orthognathic treatment which means that the benefit:risk ratio is high for the majority of patients.
Long-term stability
Stability following a joint orthodontic-surgical approach depends largely on the surgical technique, fixation, and the amount and direction of movement performed, with a hierarchy of stability reported and usually classified as: <2 mm; 2–4 mm or >4 mm of change.55 The study demonstrated that greater skeletal change than dental change was observed, and that dento-alveolar adaptation takes place to compensate for the skeletal changes. A clinically relevant (>2 mm) post-treatment change was observed between 1 and 5 years to a greater degree in Class II/long face patients compared with Class III patients. Stability is an issue which the MDT discusses carefully with each individual patient, with reference to the potential relapse for that particular malocclusion type. This is an essential part of the pre-treatment informed consent process.
Conclusions
An orthognathic approach for the management of severe dento-facial discrepancies has been shown to be associated with positive effects for the patient in terms of enhanced aesthetics, function and quality of life. However, the treatment process is complex and the importance of the close working relationship between the orthodontist, surgeon and other members of the team in an MDT setting cannot be over-emphasised. By working in such a clinical environment, the likelihood of achieving optimum outcomes is increased.
References
Steinhäuser E W . Historical development of orthognathic surgery. J Cranio-Maxillofac Surg 1996; 24: 195–204.
Proffit W R, White R P Jr . Who needs surgical orthodontic treatment? International J Adult Orthod Orthognath Surg 1990; 5: 81–89.
Sandy J R, Irvine G H, Leach A . Update on orthognathic surgery. Dent Update 2001; 28: 337–345.
Templeton K M, Powell R, Moore M B, Williams A C, Sandy J R . Are the peer assessment rating index and the index of treatment complexity, outcome, and need suitable measures for orthognathic outcomes? Eur J Orthod 2006; 28: 462–466.
Ryan F S, Barnard M, Cunningham S J . Impact of dentofacial deformity and motivation for treatment: a qualitative study. Am J Ortho Dentofac Orthop 2012; 141: 734–742.
Seehra J, Fleming P S, Newton T, DiBiase A T . Bullying in orthodontic patients and its relationship to malocclusion, self-esteem and oral health-related quality of life. J Orthod 2011; 38: 247–256.
Al-Bitar Z B, Al-Omari I K, Sonbol H N, Al-Ahmad H T, Cunningham S J . Bullying among Jordanian schoolchildren, its effects on school performance, and the contribution of general physical and dentofacial features. Am J Orthod Dentofac Orthop 2013; 144: 872–878.
Macgregor F C . Social and psychological implications of dentofacial disfigurement. Angle Orthod 1970; 40: 231–233.
Lansdown R, Lloyd J, Hunter J . Facial deformity in childhood: severity and psychological adjustment. Child: Care Health Dev 1991; 17: 165–171.
Laufer D, Glick D, Gutman D, Sharon A . Patient motivation and response to surgical correction of prognathism. Oral Surg Oral Med Oral Pathol 1976; 41: 309–313.
Jensen S H . The psycho-social dimensions of oral and maxillofacial surgery: a critical review of the literature. J Oral Surg 1978; 36: 447–453.
Heldt L, Haffke E A, Davis L F . The psychological and social aspects of orthognathic treatment. Am J Ortho 1982; 4: 318–328.
Garvill J, Garvill H, Kahnberg KE, Lundgren S . Psychological factors in orthognathic surgery. J Craniomaxillofac Surg 1992; 20: 28–33.
Cunningham S J, Hunt N P, Feinmann C . Perceptions of outcome following orthognathic surgery. Br J Oral Maxillofac Surg 1996; 34: 210–213.
Williams A C, Shah H, Sandy J R, Travess H C . Patients' motivations for treatment and their experiences of orthodontic preparation for orthognathic surgery. J Orthod 2005; 32: 191–202.
Hunt N P, Cunningham S J . The influence of orthognathic surgery on occlusal force in patients with vertical facial deformities. Int J Oral Maxillofac Surg 1997; 26: 87–91.
Stirling J, Latchford G, Morris D O, Kindelan J, Spencer R J, Bekker H L . Elective orthognathic treatment decision making: a survey of patient reasons and experiences. J Orthod 2007; 34: 113–127.
Forssell H, Finne K, Forssell K, Panula K, Blinnikka L M . Expectations and perceptions regarding treatment: a prospective study of patients undergoing orthognathic surgery. Int J Adult Orthodon Orthognath Surg 1998; 13: 107–113.
Proothi M, Drew S J, Sachs S A . Motivating factors for patients undergoing orthognathic surgery evaluation. J Oral Maxillofac Surg 2010; 68: 1555–1559.
Alanko O M, Svedström-Oristo A L, Tuomisto M T . Patients' perceptions of orthognathic treatment, well-being, and psychological or psychiatric status: a systematic review. Acta Odontol Scand 2010; 68: 249–260.
World Health Organization. WHOQOL; Measuring quality of life. 1997. Available online at: http://www.who.int/mental_health/media/68.pdf (accessed 19 January 2015).
Lee S, McGrath C, Samman N . Quality of life in patients with dentofacial deformity: a comparison of measurement approaches. Int J Oral Maxillofac Surg 2007; 36: 488–492.
Rusanen J, Lahti S, Tolvanen M, Pirttiniemi P . Quality of life in patients with severe malocclusion before treatment. Eur J Orthod 2010; 32: 43–48.
Ireland A J, Cunningham S J, Petrie A et al. An index of orthognathic functional treatment need (IOFTN). J Orthod 2014; 41: 77–83.
Luther F, Morris D O, Hart C . Orthodontic preparation for orthognathic surgery: how long does it take and why? A retrospective study. Brit J Oral Maxillofac Surg 2003; 41: 401–406.
Luther F, Morris D, Karnezi K . Orthodontic treatment following orthognathic surgery: How long does it take and why? A retrospective study. J Oral Maxillofac Surg 2007; 65: 1969–1976.
Kiyak H A, West R A, Hohl T, McNeill R W . The psychological impact of orthognathic surgery: a 9-month follow-up. Am J Orthod 1982; 81: 404–412.
Morris D O . Improving standards in orthognathic care: the bigger picture (a national and international perspective). J Orthod 2006; 33: 149–151.
Loh S, Yow M . Computer prediction of hard tissue profiles in orthognathic surgery. Int J Adult Orthod Orthognath Surg 2002; 17: 342–347.
Power G, Breckon J, Sherriff M, McDonald F . Dolphin Imaging Software: An analysis of the accuracy of cephalometric digitization and orthognathic prediction. Int J Oral Maxillofac Surg 2005; 34: 619–626.
Jones R M, Khambay B S, McHugh S, Ayoub A F . The validity of a computer-assisted simulation system for orthognathic surgery (CASSOS) for planning the surgical correction of class III skeletal deformities: single-jaw versus bimaxillary surgery. Int J Oral Maxillofac Surg 2007; 36: 900–908.
Suri L, Taneja P . Surgically assisted rapid palatal expansion: A literature review. Am J Orthodont Dentofac Orthoped 2008; 133: 290–302.
Fedorowicz Z, Nasser M, Newton J T, Oliver R J . Resorbable versus titanium plates for orthognathic surgery. Cochrane Database Syst Rev 2007; CD006204.
Department of Health. High Quality of Care for all. NHS Next Stage Review Final Report. London: The Stationery Office, 2008.
Cunningham S J, Garratt A M, Hunt N P . Development of a condition-specific quality of life measure for patients with dentofacial deformity: II. Validity and responsiveness testing. Community Dent Oral Epidemiol 2002; 30: 81–90.
Esperão P T, de Oliveira B H, de Oliveira Almeida M A, Kiyak H A, Miguel J A . Oral health-related quality of life in orthognathic surgery patients. Am J Orthod Dentofacial Orthop 2010; 137: 790–795.
Murphy C, Kearns G, Sleeman D, Cronin M, Allen P F . The clinical relevance of orthognathic surgery on quality of life. Int J Oral Maxillofac Surg 2011; 40: 926–30.
Hunt O T, Johnston C D, Hepper P G, Burden D J . The psychosocial impact of orthognathic surgery: a systematic review. Am J Orthod Dentofacial Orthop 2001; 120: 490–497.
Soh C L, Narayanan V . Quality of life assessment in patients with dentofacial deformity undergoing orthognathic surgerya systematic review. Int J Oral Maxillofac Surg 2013; 42: 974–980.
Kiyak H A, McNeill R W, West R A, Hohl T, Bucher F, Sherrick P . Predicting psychologic responses to orthognathic surgery. J Oral Maxillofac Surg 1982; 40: 150–155.
Kiyak H A, Hohl T, West R A, McNeill R W . Psychologic changes in orthognathic surgery patients: a 24-month follow up. J Oral Maxillofac Surg 1984; 42: 506–512.
Øland J, Jensen J, Melsen B . Factors of importance for the functional outcome in orthognathic surgery patients: a prospective study of 118 patients. J Oral Maxillofac Surg 2010; 68: 2221–2231.
Magalhães I B, Pereira L J, Marques L S, Gameiro G H . The influence of malocclusion on masticatory performance. A systematic review. Angle Orthod 2010; 80: 981–987.
Vicini C, Dallan I, Campanini A et al. Surgery vs ventilation in adult severe obstructive sleep apnea syndrome. Am J Otolaryngol 2010; 31: 14–20.
Holty J-E C, Guilleminault C . Maxillomandibular advancement for the treatment of obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev 2010; 14: 287–297.
Flanary C M, Alexander J M . Patient responses to the orthognathic surgical experience: factors leading to dissatisfaction. J Oral Maxillofac Surg 1983; 41: 770–774.
Flanary C M, Barnwell G M Jr, Alexander J M . Patient perceptions of orthognathic surgery. Am J Orthod 1985; 88: 137–145.
Cunningham S J, Hunt N P, Feinmann C . Psychological aspects of orthognathic surgery: a review of the literature. Int J Adult Orthodon Orthognath Surg 1995; 10: 159–172.
Chen B, Zhang Z K, Wang X . Factors influencing postoperative satisfaction of orthognathic surgery patients. Int J Adult Orthodon Orthognath Surg 2002; 17: 217–222.
Cunningham S J, Sculpher M, Sassi F, Manca A . A cost-utility analysis of patients undergoing orthognathic treatment for the management of dentofacial disharmony. Br J Oral Maxillofac Surg 2003; 41: 32–35.
Panula K, Keski-Nisula L, Keski-Nisula K, Oikarinen K, Keski-Nisula S . Costs of surgical-orthodontic treatment in community hospital care: an analysis of the different phases of treatment. Int J Adult Orthodon Orthognath Surg. 2002; 17: 297–306.
Travess H, Roberts-Harry D, Sandy J . Orthodontics. Part 6: Risks in orthodontic treatment Br Dent J 2004; 196: 71–77.
Sousa C S, Turrini R N . Complications in orthognathic surgery: A comprehensive review. J Oral Maxillofac Surg Med Pathol 2012; 24: 67–74.
Iannetti G, Fadda T M, Riccardi E, Mitro V, Filiaci F . Our experience in complications of orthognathic surgery: a retrospective study on 3: 236 patients. Eur Rev Med Pharmacol Sci. 2013; 17: 379–384.
Proffit W R, Turvey T A, Phillips C . The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med 2007; 3: 21–32.
Acknowledgements
Many thanks to the patients who allowed their photographs to be used in this publication. Thank you to: Mr Tim Lloyd (Maxillofacial Surgeon, Eastman Dental Hospital, UCLH Foundation Trust) who undertook the surgery for the patients whose photographs are shown in Figures 1, 2, 3, 7 and 8, and also to Mr Neil Patel for the photographs in Figure 2 and Mr Tom McDonald for the photographs in Figure 5.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Cunningham, S., Johal, A. Orthognathic correction of dento-facial discrepancies. Br Dent J 218, 167–175 (2015). https://doi.org/10.1038/sj.bdj.2015.49
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.49
This article is cited by
-
Long-term effectiveness of non-surgical open-bite treatment: a systematic review and meta-analysis
Progress in Orthodontics (2023)
-
Aktueller Stand und Entwicklung in der Dysgnathietherapie
Der MKG-Chirurg (2022)