Key Points
-
Discusses the correct doses of commonly used local anaesthetics.
-
Provides greater ease in calculating safe doses of local anaesthetics in children.
-
Describes techniques that will make it easy to 'double check' calculations.
Abstract
While local anaesthetic agents are usually safe and are used ubiquitously, inadvertent overdoses may have potentially fatal consequences. Errors in the dosing of local anaesthetics frequently occur due to inherent difficulties in remembering the toxic dosage limits, difficulties in performing the appropriate calculations correctly, and errors in estimating patient weight. We have developed a simple graphical calculation aid (nomogram) to overcome these problems and facilitate rapid cross-checking of the maximum safe dose for a variety of local anaesthetic agents in common use. Standard mathematical techniques were used to draft the nomogram. A randomised blinded study using simulated patient data and Bland-Altman analysis was used to assess the accuracy and precision of the nomogram. The nomogram was found to have a bias of 0.0 ml, with limits of agreement -0.05–0.04 ml. It was found to be easy to use and suitably accurate for clinical use.
Similar content being viewed by others
Background
Local anaesthetics are the most commonly used drugs in dental practice, with approximately 300 million cartridges used annually in the United States alone.1 Surveys estimate that most practising dentists will use between 1,600–1,800 cartridges per year, on average.1,2 Problems related to overdose are rare, but can be fatal.3 It is thus surprising that in clinical practice many dentists do not calculate exact safe doses, but rely instead on estimates.4 This may well be because of the complexity of the calculation: maximum doses must be remembered, and are quoted in mg per kilogram body weight; while for historical reasons, agent concentrations are often given in units of percentage weight-in-volume (% w/v).
Recently, Williams and Walker5 developed a nomogram for calculating dose volumes of local anaesthetics used in a hospital setting. For of a number of reasons this is not suitable for use in dentistry: commonly used dental anaesthetic agents such as articaine are not included; the maximum doses used are appropriate for a hospital setting, whereas dentists tend to use far more conservative values;6,7,8 and finally, the nomogram requires that patient weight is known, which frequently is not available in a dental clinic.4,9,10 We have thus adapted the hospital nomogram for dental use.
Local anaesthetic agents
Williams and Walker demonstrated in their original paper5 that for any particular anaesthetic agent in a given concentration, the dose of anaesthetic allowed per unit weight is a constant. They referred to this as the 'dosage factor', which is calculated as:
Dosage factor (ml/kg) = maximum dose (mg/kg)/concentration (mg/ml)
Application of these dosage factors reduces the steps involved, and hence potential for errors, in calculating the maximum volume of local anaesthetic. We have listed the local anaesthetic agents commonly used in dentistry, with their maximum recommended doses, concentrations in mg per ml, and their dosage factors (Table 1). Some formulations of local anaesthetic include added vasoconstrictors such as adrenaline and felypressin. However these have not been included in our analysis, as for formulations in regular use, the maximum dose of local anaesthetic is reached before the amount of vasoconstrictor approaches toxic levels. Furthermore, in dental practice most authorities do not advocate increasing the maximum allowable dose of local anaesthetic when used in combination with a vasoconstrictor.6,7,8,11
Body weight
The British National Formulary (BNF) recommends that local anaesthetic dose should be based on ideal body weight, rather than actual weight.12 There are many different ways of estimating ideal body weight, ranging from the simple formula used by the Advanced Paediatric Life Support group13 to a variety of more complex techniques;14,15 however the estimates obtained by applying a simple mathematical equation may differ widely from real-life values. We have therefore used the median weight for age from data freely available from the Child Growth Foundation.16 This allows us to have different scales for boys and girls that also take into account the nonlinear weight changes which occur due to teenage growth spurts.
Local anaesthetic volume
As well as indicating the maximum permitted volume of local anaesthetic in millilitres, we have included a scale to indicate the equivalent volume in 'cartridges', as cartridges are commonly used as units of administered volume. Our scale is based on the standard UK cartridge size of 2.2 ml. If smaller cartridge sizes are used (for example, international 1.7 ml cartridges), the same number of cartridges may be administered as indicated by the nomogram, but the calculation will provide an additional margin of safety.
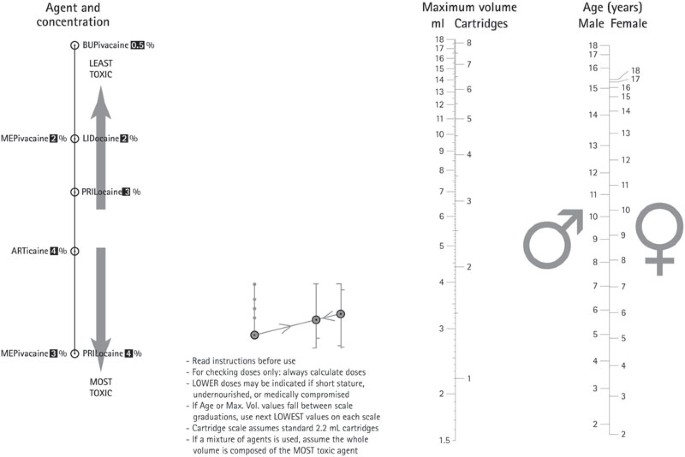
The nomogram (Fig. 1) was designed and drafted using the methods previously described.5,17,18 This involves rewriting the earlier equation as a 'determinant matrix', a mathematical construct which encodes the equation in a manner from which the axes of the nomogram can then be drafted.17,18 Open source software was used to aid drafting of the nomogram (Pynomo), and further detail was added using a commercial graphics package (Rhinoceros 3D).
To calculate the maximum volume allowed for a given local anaesthetic, a straight line is drawn from the appropriate type and concentration of local anaesthetic on the left-hand axis to the child's age and gender on the right hand axis. The maximum safe volume (in ml and number of cartridges) is read where the line intersects the middle axis. The use of a logarithmic scale for this axis ensures greater accuracy at more clinically significant lower body weights. If the line falls between scale gradations, it is recommended that the next lower gradation is used in order to provide an extra margin of safety.
We assessed the accuracy of the nomogram using Bland-Altman analysis.19 A Microsoft Excel spreadsheet was used to generate 140 sets of simulated patient data, each with randomised values for age, gender, and formulation (that is, agent and concentration) of local anaesthetic. The nomogram and spreadsheet were then used to calculate for the maximum safe dose of local anaesthetic in each case, and the results of the two methods of calculation were compared using Bland-Altman analysis. The maximum safe volume of local anaesthetic for each patient was calculated using the nomogram independently by two of the authors (DW and JW), both of whom were blinded to the 'correct' value. It was decided a priori that the results obtained by DW would be used for accuracy calculation and those by JW for precision.
Results
One hundred and forty sets of simulated patient data were generated. The maximum safe volume of local anaesthetic was calculated three times for each set of data: by spreadsheet, and by both authors independently – that is, 420 calculations in total.
Bland-Altman analysis showed that the nomogram has a bias of 0.0 ml, with limits of agreement -0.05–0.04 ml. This means that 95% of the readings fall within this range. A variation in administered volume of -0.05–0.04 ml is of no clinical significance, and therefore it was considered that accuracy of the nomogram is within a clinically acceptable range. The repeatability coefficient was 0.9%, which means that independent clinicians using the nomogram would expect to obtain a result within 0.9% of each other on 95 out of 100 occasions. Thus the accuracy and repeatability of the nomogram are suitable for clinical use.
Discussion
A nomogram (or 'alignment chart') is a low cost graphical calculation aid which expresses a specific mathematical relationship, and allows calculations to be rapidly performed to typical accuracy of three significant figures, which is acceptable for most clinical applications. Prior to the introduction of electronic calculators in the 1970s, nomograms were widely used in engineering, medicine, statistics, and accounting. Despite the subsequent proliferation of computers and smart phone apps, nomograms have a number of advantages over electronic devices: they are simple to use, extremely low cost and robust, and the user does not need to remember any formulae or toxic dosage limits. If the nomogram is printed on sheets of paper, drawing a line across the axes simultaneously performs the calculation and provides a permanent record for filing in patient notes.
The recommended maximum doses listed in Table 1 are those recommended by the American Academy of Paediatric Dentistry (AAPD),7 but are also reflected by other sources.6,8 As discussed above, these are lower, more conservative doses than would normally be used by some other medical professionals,5,20 and this possibly reflects the fact that much dental work is undertaken in a community setting where facilities to manage overdoses are not readily available. Furthermore, in medical practice vasoconstrictors are often used to facilitate administration of higher doses of local anaesthetic.12 However for reasons of safety, many dental authorities do not recommend this practice:7,8,21,22 instead they restrict indications for vasoconstrictors to increasing the duration of action of local anaesthesia, and for haemostasis. These guidelines originate from the Council of Dental Therapeutics of the American Dental Association, based on the increased risk of anaesthetic absorption from intra-oral injections.21 In spite of this, some sources quote higher doses (although in an adult context);1 the issue is further confused by the fact that the BNF does not quote maximum doses for dental anaesthetic agents at all, but instead advises reference to 'specialist dental literature'.12 In the absence of a suitable British equivalent to the AAPD guidance, the authors have adopted the latter more conservative, and therefore safer, guidelines to inform drafting of the nomogram.
In many fields where calculations are critical, the practice of independent checking is mandatory.5 The speed and simplicity of the nomogram makes it ideal as a method for cross-checking a calculation that has been carried out by conventional methods. We recommend the following procedure: the dentist will declare a maximum number of cartridges of a particular agent he or she would intend to use; the assistant would then use the nomogram and confirm that this number of catridges is safe. If the volume indicated by the nomogram differs markedly from the volume intended, then the calculation is rechecked by both the dentist and the assistant. Once the maximum allowable volume has been calculated and cross-checked, the dentist knows that he or she can administer volumes up to this amount with minimal risk of side effects or overdosage.
Our nomogram calculates ideal body weight based on UK growth chart medians, and uses these to calculate the maximum permissible volume of local anaesthetic. For most cases this is valid; however the calculation should be modified for patients with malnutrition or short stature to take into account the child's actual weight. In such circumstances, multiplying the weight by the appropriate dosage factor listed in Table 1 is a simpler method than the traditional multi-step process, and is thus less likely to result in error.
Similarly it should be remembered that the maximum recommended doses and volumes quoted above, and used in construction of our nomogram, are based on fit and healthy patients. Regardless of the method of calculation, the maximum recommended doses and volumes should be modified appropriately for patients who are medically compromised.
References
Haas D A . An update on local anesthetics in dentistry. J Can Dent Assoc 2002; 68: 546–551.
Gaffen A S, Haas D A . Survey of local anesthetic use by Ontario dentists. J Can Dent Assoc 2009; 75: 649.
Hersh E V, Helpin M L, Evans O B . Local anesthetic mortality: report of case. J Dent Child 1991; 58: 489–491.
Kohli K, Ngan P, Crout R, Linscott C C . A survey of local and topical anesthesia use by pediatric dentists in the United States. Pediatr Dent 2001; 23: 265–269.
Williams D J, Walker J D . A nomogram for calculating the maximum dose of local anaesthetic. Anaesthesia 2014; 69: 847–853.
Adewale L . Anaesthesia for paediatric dentistry. Contin Educ Anaesth Crit Care 2012; 12: 288–294.
American Academy of Pediatric Dentistry. Guideline on appropriate use of local anesthesia for pediatric dental patients. Pediatr Dent 2009; 30: 134–139.
Malamed S . Systemic complications. In Malamed S Handbook of local anesthesia. 5th ed. pp 312. St Louis, MO: Mosby, 2004.
Yuan J C-C, Lee D J, Afshari F S, Galang M T S, Sukotjo C . Dentistry and obesity: a review and current status in U S. predoctoral dental education. J Dent Educ 2012; 76: 1129–1136.
D'Mello G, Chia L, Hamilton S D, Thomson W M, Drummon B K . Childhood obesity and dental caries among paediatric dental clinic attenders. Int J Paediatr Dent 2011; 21: 217–222.
Adams V, Marley J, McCarroll C . Prilocaine induced methaemoglobinaemia in a medically compromised patient. Was this an inevitable consequence of the dose administered? Br Dent J 2007; 203: 585–587.
Joint Formulary Committee. British national formulary. 68th ed. London: The British Medical Association and Royal Pharmaceutical Society of Great Britain, 2014.
Advanced Life Support Group. Advanced paediatric life support. 4th ed. Oxford: Blackwell Publishing Ltd, 2004.
Phillips S, Edlbeck A, Kirby M, Goday P . Ideal body weight in children. Nutr Clin Pract 2007; 22: 240–245.
Callaghan L C, Walker J D . An aid to drug dosing safety in obese children: development of a new nomogram and comparison with existing methods for estimation of ideal body weight and lean body mass. Anaesthesia 2014; 70: 176–182.
Cole T J, Freeman J V, Preece M A . Body mass index reference curves for the UK, 1990. Arch Dis Child 1995; 73: 25–29.
Williams D J, Walker J D . A nomogram to calculate the physiological and operative severity score for the enumeration of mortality and morbidity (POSSUM). Br J Surg 2014; 101: 239–245.
Levens A S . Nomography. 2nd ed. New York: Wiley & Sons; London: Chapman & Hall, 1959.
Bland J M, Altman D . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 327: 307–310.
Allman K . Oxford handbook of anaesthesia. 3rd ed. Oxford, New York: Oxford University Press, 2011.
Mehra P, Caiazzo A, Maloney P . Lidocaine toxicity. Anesth Prog 1998; 3006: 38–41.
Malamed S . Pharmacology of vasoconstrictors. In Malamed S Handbook of local anesthesia. 5th ed. pp 41–54. St. Louis, Mo: Mosby, 2004.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Walker, J., Summers, A. & Williams, D. A nomogram to calculate the maximum dose of local anaesthetic in a paediatric dental setting. Br Dent J 218, 469–471 (2015). https://doi.org/10.1038/sj.bdj.2015.297
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.297
This article is cited by
-
Techniques for effective local anaesthetic administration for the paediatric patient
British Dental Journal (2020)