Key Points
-
Discusses the position of clinical audit within an organisation's overall clinical effectiveness structure.
-
Describes the benefits of clinical audit in achieving long-term improvements in patient safety.
-
Encourages the use of clinical audit as a proven method for improving patient safety.
Abstract
The improvement of patient safety has been a long-term aim of healthcare organisations and following recent negative events within the UK, the focus on safety has rightly increased. For over twenty years, clinical audit has been the tool most frequently used to measure safety-related aspects of healthcare and when done so correctly, can lead to sustained improvements. This paper explains how clinical audit is used as a safety improvement tool in an English dental hospital and gives several examples of projects that have resulted in long-term improvements in secondary dental care.
Similar content being viewed by others
Introduction
For every person who is referred to and attends a dental hospital, their journey through the healthcare system is potentially complex, lengthy and brings them into contact with numerous members of the dental team. This person may receive primary, secondary and tertiary level care, delivered by undergraduate and postgraduate dental students, members of the non-clinical dental team and from qualified dental clinicians, at various stages of their professional development and training, from foundation dentists to specialists and consultants.
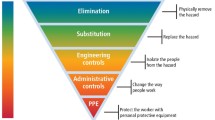
As clinicians, we all recognise the dental care we deliver and the environment we work in have the potential to cause harm to our patients and to our colleagues, either immediately or over a longer period of time. As significant numbers of staff in training and students within the hospital move on and are replaced each year, there is a need to constantly retrain all colleagues in appropriate working methods. Following recognised good practice, working within clear guidelines, adhering to formal policies and taking responsibility as part of the wider dental team will all significantly reduce the risk of harm occurring. These are emphasised as important principles of clinical governance, as defined by the former Chief Medical Officer, Professor Sir Liam Donaldson: 'A framework through which all NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care, by creating an environment in which excellence in clinical care will flourish.'1
Clinical governance reduces the risk of harm. It prevents bad things from happening to anyone. It is the first of two major steps we take to improve patient care. The second step is to strive for a high quality healthcare system that is focused on improvement. The quality approach aims to makes things better for every patient and for each member of the healthcare team.
The term 'clinical effectiveness' brings together clinical governance and quality in healthcare. Modern clinical effectiveness is not something that we only do when we are being supervised. It is not something we 'only do at meetings' or 'on a Thursday morning'. It is woven into every patient contact, every clinical letter, every telephone call, every complaint action plan, every service contract negotiation and every set of performance indicators.
In essence, clinical effectiveness is therefore something that must be central to the culture of every healthcare team, whether in a large dental hospital or a small dental practice.
However, we cannot improve if we do not understand how good or poor we are at present and if we do not have a realistic vision of where we need to reach. This is why clinical audit is the ideal tool for measuring our current position. It allows us to compare ourselves to an ideal 'gold' standard and gives us the information required to make a positive change.
What is clinical audit?
Clinical audit has developed over more than 20 years into the process we use today. The initial inclusion of 'medical audit' within NHS healthcare was in 1989, in the Government White Paper entitled Working for patients.2
In 2002,3 the National Institute for Health and Clinical Excellence (NICE) published the papers: Principles for best practice in clinical audit. In these papers, clinical audit is defined as: 'A quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change. Aspects of the structure, processes, and outcomes of care are selected and systematically evaluated against explicit criteria. Where indicated, changes are implemented at an individual, team or service level and further monitoring is used to confirm improvement in healthcare delivery.'
To simplify this definition, the commonly seen diagram of the 'clinical audit cycle' identified the five stages (Fig. 1):
-
1
Identify the audit topic, based on a clinical problem or issue
-
2
Set the standard, usually based on a previously determined ideal
-
3
Collect the data by observing clinical practice
-
4
Analyse the data and compare it to the standard
-
5
Implement change to clinical practice to allow an improvement.
The concept of the clinical audit cycle (Fig. 2) only truly becomes effective when the process is repeated following the implementation of those changes required to make the improvement. Over a period of time, as the cycle is repeated, the process becomes a 'clinical audit spiral'.
The clinical audit structure within a dental hospital setting
When clinical audit began within the dental hospital, it was sporadic in nature. There was no annual plan and no stated action plans to end each initial audit cycle. It was unclear whether the financial and personal resources involved in audit projects resulted in sustained improvement to patient care. In order to correct this situation, a series of structures and arrangements were developed, in conjunction with similar changes elsewhere in the trust. The University Dental Hospital of Manchester (UDHM) is a division of the Central Manchester University Hospitals NHS Foundation Trust (CMFT). It is closely associated with the School of Dentistry, as part of the University of Manchester.
The CMFT clinical effectiveness structures are also present within each division. Therefore, the clinical audit structures are as follows:
CMFT Clinical Effectiveness Committee
Dental Clinical Effectiveness Committee
CMFT Clinical Audit Committee
Dental Clinical Audit Committee
CMFT Clinical Audit projects
Dental Clinical Audit projects
All clinical audit activity within the dental division is coordinated by the Dental Clinical Audit Committee (DCAC), which has representation from each staff group and from each dental speciality. Members are selected with an emphasis on their ability to be influential among colleagues and to provide continuity over a period of several years. The chairperson of the CMFT Clinical Audit Committee and the clinical audit facilitator are also members. The DCAC meets once a month and each representative will either be present or send a deputy. The chairperson of DCAC represents the dental division on the CMFT Clinical Audit Committee. The chairperson of DCAC also reports on clinical audit to the Dental Clinical Effectiveness Committee, which oversees all clinical ffectiveness issues in the Dental Division and is chaired by the Clinical Head of Division.
Factors in the success of the clinical audit process at UDHM
Clinical audit proposals are discussed either at the DCAC meetings or individually with the chairperson. Those accepted are added to the annual forward plan, with most projects being agreed and added in line with the clinical audit year (in line with the financial year). Accepted projects are clearly focused on the division's clinical effectiveness priorities. They are of interest to the hospital staff and the outcomes are rapidly shared with colleagues. The projects are often reported as an integral part of the hospital's clinical effectiveness dashboard.
Many projects are associated with risk prevention, although when necessary, some projects are used in response to adverse incidents. The quality of accepted projects is more important than the quantity of current projects.
The Clinical Audit Committee and all its activity has a positive long-term momentum, with DCAC members remaining on the committee for several years, projects being re-audited when appropriate and audit project leads always being members of senior staff on long-term contracts.
A strong team approach within the hospital is maintained, with projects being undertaken by colleagues of all professional groups and at all stages of their training and development.
Completed projects are reported at committees, published in the hospital's biannual clinical audit newsletter and a selection presented at the hospital's quarterly 'audit and clinical effectiveness' days (ACE days). These ACE days are protected time when routine clinical activity is cancelled. The days are divided into a session when all hospital personnel gather together to listen and discuss relevant whole hospital clinical effectiveness issues, including clinical audit and a session when each clinical speciality gathers together as a team to discuss issues relevant to their speciality.
All members of staff receive training in clinical audit method, provided by either the facilitator or the experienced clinical audit leads, when they become involved in an audit. In addition to the clinical audit activity of the NHS hospital, the senior student dentists all undertake a clinical audit project, submitted as part of their final BDS examinations. Some of these make a valuable contribution to the DCAC clinical audit activity.
As such, clinical audit is deeply embedded in the structure and functions of the Dental Hospital. It is part of the CMFT and UDHM clinical effectiveness structures. It is also an open and transparent process, involving colleagues of all professional groups.
To provide a systematic approach to reporting the outcomes of each clinical audit project, the hospital uses a standard audit report document. Included in this is the action plan which is recognised as being fundamental to the success of the audit project. The action plan lists each recommendation, a person responsible for implementing the recommended change and a date by which the change will be undertaken.
Monitoring of the progress of each clinical audit project and of each action plan recommendation is the shared responsibility of the project's clinical audit lead and the hospital's clinical audit facilitator.
The regular use of the progress chart demonstrates the monthly position of the hospital in terms of its overall progress with the registered clinical audit projects (Fig. 3).
Examples of audits
Audit to assess use of the safer surgery checklist
Taking the wrong tooth out is recognised as a 'never event' – it should never happen. The checklist was introduced as a method to reduce the risk of the wrong tooth being extracted. While the audit results have consistently shown a very high compliance rate with the paper checklist use, the first two years of the audit cycle failed to prevent a small number of incidents occurring. The clinical audit process itself was insufficient to bring about the sustained change in working patterns required. It was only the close collaboration between all clinical and non-clinical members of the dental team that has led to the current excellent clinical outcomes and patient safety levels.
Audit to assess the quality of information in orthodontic extraction letters
It is recognised that the risk of the wrong tooth being extracted increases when more clinicians are involved in the patient's journey (diagnosis, planning and extraction). In response to this, our dental hospital orthodontic colleagues identified a potential patient safety issue for the numerous patients who were returned to their general dental practitioner for extraction of teeth. The first 'extraction letter' audit identified the wide variation in the way that the teeth to be extracted were identified and the potential for confusion and error to occur. Recommendations for improvement were made and the re-audit undertaken one year later. While no incidents of wrong tooth extraction occurred, the second audit unfortunately identified no improvement in the content of the extraction letters.
Wider discussions allowed an understanding of this failure. Colleagues recognised that while the first audit cycle was well designed and completed, as so few orthodontic clinicians were involved in the project, other colleagues did not perceive a strong need for change. Widespread collaboration of clinicians (consultants, specialists, speciality registrars and post-graduate students) and secretaries has allowed unanimous agreement of the need for and method required for accurate communication with general dental practitioner colleagues. The audit was added to the dental hospital patient safety dashboard in 2012. The results of the third audit cycle are expected to show a significant improvement in the content of extraction letters. The need to provide education for new members of staff and post graduate students has been reinforced.
A further benefit of this audit has been on the regional specialist orthodontic services. Many dental hospital orthodontic colleagues also work in other regional hospitals and specialist practices. By implementing similar good processes in those work environments, the risk to other patients is also reduced.
The RATS audit
To assess whether clinicians consistently use good sharp safety techniques; to reduce the risk of a sharp injury from a dental instrument. This project has used the risk assessment tool for sharps (RATS), developed by an undergraduate dental student and the clinical audit lead. Any clinician can use the RATS to assess a clinical area for risks associated with sharp injuries, such as burs left in handpieces, unsheathed needles and untidy clinical areas. The audit initially showed the levels of risk on each clinic, and a two-year programme of education and sharp awareness is now showing a reduction in the sharp risk behaviour and importantly, a reduction in the number of sharp injuries (Table 1). Almost all of those incidents in 2012/13 have occurred when clinicians have not used the recommended sharp safety techniques, highlighting the need for continuing education and training.
Audit to assess the compliance with the hospital's clinical record policy
Regardless of the clinical speciality or level of seniority, one matter remains common to each clinician every day: the correct management and completion of clinical records is essential. This is audited, using the hospital's own policy, in two ways: during the annual CMFT Trust-wide clinical records audit and during the regular dental hospital-wide record keeping audits. The latter is largely undertaken by undergraduate dental students, supervised by senior clinicians. Over one thousand case records have been examined each year since 2008. Steady, impressive and consistent improvements have been achieved in all parameters, including both those relating to the condition and storage of clinical records and to the standards of each clinical entry. The improvements achieved and the recognition of this as a complex and risk-associated area has shaped understanding of the potential benefits of implementing an electronic patient record, which will overcome many of the residual problems associated with traditional paper records.
Audit of the standard of patient referral letters
This has been the longest running clinical audit project, with ten years of data. The initial audit cycles gave an understanding of the content and preferred style of referral letters. These were used in the development and production of referral guidelines and a standard referral form.4 The effect of these changes led to a dramatic improvement in the content of referral letters and therefore, the number of patient referrals accepted. For example, by advising that an endodontic referral required inclusion of a recent, high quality peri-apical radiograph, the proportion of referrals returned to general practitioner colleagues changed from 72% to 8% in two years. The audit has also identified a progressive increase in the number of referrals made to the dental hospital over this time period, the change in complexity of the clinical cases and the continued preference of many practitioners to refer directly to the dental hospital, rather than via a third party referral management centre. All of these have contributed to the development of a larger endodontic clinical team within the dental hospital and to more integrated service delivery between primary and secondary care.
Audit to assess the answering of telephone contacts
Any busy organisation, such as a large dental hospital, will have regular telephone enquiries and managing these alongside all the other responsibilities of the administrative team is a constant challenge. This audit has been regularly repeated and despite the efforts to improve matters, complaints regarding telephone contact to the dental hospital, continue to be received by the Clinical Effectiveness Committee. The outcome of the audits and responding to these complaints has provided support for the purchase of a semi-automatic call management system, similar to those used very successfully in other industries.
Audit to assess use of the hospital consent forms
The hospital uses four different consent forms, depending on the age and ability of the patient and the complexity of their care. By regular auditing of the consent process, the forms themselves have been redesigned to facilitate and strengthen the consent process. Procedure specific consent forms for endodontic treatment and for surgical removal of wisdom teeth have been developed. As the consent audit cycle has been repeated, sustained improvements have been achieved and areas for further education and development have been identified.
Audit to assess the outcomes of endodontic surgery
A senior clinician identified the unsatisfactory outcomes of endodontic surgery as an area requiring improvement. By using the clinical audit method, a satisfactory outcome from treatment was shown to improve from 47% to 81% in one year. These success rates have been maintained for five further cycles and continuing improvements have been achieved as better case selection, clinical techniques and materials have been introduced.
Audit of the accuracy of dental implant placement
The dental hospital has a busy dental implant service, with over 60 staff members, of all professional groups, closely involved in providing care for these patients. The surgical placement of each implant of the correct dimension, at the correct position, angulation, depth and separation is very likely to lead to a satisfactory treatment outcome. Unfortunately, such a positive outcome has not always been achieved and the inappropriate selection and positioning of dental implants that cannot subsequently be restored has occurred. Such an occurrence is now considered as a 'never event'. If three-way planning of treatment between restorative dentist, dental technologist and oral surgeon is carried out, the risk of harm to the patient is lessened.
In response to a reported incident of incorrect implant placement, a subsequent audit has highlighted the need for closer collaboration between colleagues. Rather than blame the surgeon for poor surgery, the restorative dentist for poor planning and prescription of treatment, or the dental technologist for poor laboratory techniques, the audit clearly highlighted that the involvement of all three parties is required if the patient is to have safe surgery, leading to a high quality outcome. Changes introduced to the process of providing such complex, multidisciplinary care has led to improvements in the proportion of implants that are placed in the ideal position, reduced the duration of the patient journey through treatment and for three years, has prevented the placement of implants that cannot be restored.
Audit of the correct use of selection criteria for dental implant funding applications
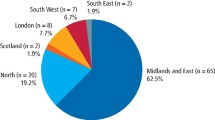
Dental implant treatment is relatively expensive, when compared to many other dental treatments. Significant variations exist between the availability of such treatment across England. The treatment is not usually part of the NHS commissioned services in a dental hospital and applications, on a patient-by-patient basis are required. Therefore, in 2012, a list of clinical conditions that can be managed by dental implant treatment has been included in a guidance document by the Royal College of Surgeons of England.5
In response to suggestion by local NHS commissioners that the funding for dental implant treatment was to be reviewed, the results of audits completed at the dental hospital clearly demonstrated that only those patients who fit within the selection criteria were offered treatment and that we had used clinical audit to ensure an improvement in the quality and safety of patient care. Subsequent closer working with the NHS commissioners and consultants in dental public health has led to the rapid development and implementation of selection criteria, closely based on the RCS document, and a new dental implant funding application form. Clinicians can now give their patients a clearer understanding of whether an application can be made and commissioners have confidence that the funding is only being used for appropriate cases.
Audit to assess compliance with a checklist for patients presenting with trismus to the temporomandibular disorders (TMD) clinic
Most of the clinical audit activity is focused on dentally-related subjects. The dental hospital is also involved in diagnosis and management of other conditions presenting in the head and neck region. Two patients presented with trismus to the TMD clinic, where malignancy was the underlying cause but where there was a delay in diagnosis.
In response to these incidents, all colleagues involved in the TMD clinic worked together to develop a 'trismus checklist', which would be used as part of the initial assessment of each referral to help highlight non-TMD causes as the underlying reason for presenting with trismus. Three audits cycles have shown consistently high compliance rates with the use of the trismus checklist.
Audit to assess compliance with NICE guidelines for wisdom tooth extraction
Although this guidance has recently come under question,6 this is a long running, annual clinical audit to assess compliance with some of the earliest NICE guidance, from March 2000.7 The audit process benefits from having a nationally agreed standard to which our clinical practice can be compared. The guidance is now well ingrained in oral surgery clinical practice and the dental hospital consistently shows very good levels of compliance.
Conclusions
Clinical audit is undertaken across the NHS and within our dental hospital. It is an important part of our patient safety and quality improvement processes. It helps to prevent bad things happening to patients who attend our hospital and helps to improve matters for all our patients, staff and students.
However, over the last ten years, we have learned several important lessons on how to get to the best from this valuable tool, as even a well-conducted audit cycle does not necessarily lead to lasting improvements. Therefore, we recommend:
-
A formal structure is required. This should constitute individuals and groups of colleagues in key positions within the organisation who have the ability to be influential among their own teams and are expected to remain in post for a number of years, to provide continuity. The structure needs a regular timetable of meetings and events and allow direct communication upwards within the hospital and the trust and sideways to colleagues of all professional groups and grades.
-
Repeated training and education is required to ensure involvement of the significant numbers of staff members and students who are replaced each year.
-
Clinical audit proposals are accepted as part of the annual forward plan, if they are in keeping with local, trust or national patient safety and quality improvement priorities.
-
The progression of each clinical audit project is closely monitored through the stages of registration, data collection, data analysis, draft report and completed report.
-
The timely completion of each recommendation in the action plan is closely monitored before the next audit cycle is performed.
References
Scally G, Donaldson L J . Clinical governance and the drive for quality improvement in the new NHS in England. BMJ 1998; 317: 61–65.
Department of Health. Working for patients. London: The Stationery Office, 1989. (Cm 555).
National Institute for Clinical Excellence. Principles of best practice in clinical audit 2002. Abingdon, Oxon: Radcliffe Medical Press, 2002.
Central Manchester University Hospitals. Referral Information for Dental Practitioners. Online information available at http://www.cmft.nhs.uk/dental/for-professionals (accessed September 2014).
Alani A, Bishop K, Djemal S, Renton T . Guidelines for selecting appropriate patients to receive treatment with dental implants: priorities for the NHS. RCS England Clinical Guidelines, 2012.
Mansoor J, Jowett, A, Coulthard P. NICE or not so NICE?. Br Dent J 2013; 215: 209–212.
National Institute for Health and Care Excellence. Technology Appraisal TA1: Wisdom Teeth – removal: guidance. Online information available at http://www.nice.org.uk/guidance/ta1 (accessed September 2014).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Ashley, M., Pemberton, M., Saksena, A. et al. Improving patient safety in a UK dental hospital: long-term use of clinical audit. Br Dent J 217, 369–373 (2014). https://doi.org/10.1038/sj.bdj.2014.861
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.861
This article is cited by
-
The development of a restorative Managed Clinical Network within the defence primary healthcare organisation
British Dental Journal (2021)
-
Dentists' perceptions of smart phone use in the clinical environment
British Dental Journal (2018)
-
Improving patient safety through a clinical audit spiral: prevention of wrong tooth extraction in orthodontics
British Dental Journal (2017)
-
Review of never and serious events related to dentistry 2005–2014
British Dental Journal (2016)