Key Points
-
Suggests that clinical investigation of the oral cavity and collection of saliva is indicated for diagnosis of oral dryness.
-
Stresses it does not seem possible to diagnose oral dryness by mere visual inspection of photographed tongues.
-
Informs dentists are as good as non-dentists in judging intraoral pictures of the tongue. Therefore more insight in aspects of judging oral dryness by visual inspection is needed.
Abstract
Background Oral dryness or hyposalivation is a major clinical problem. Several chairside tests or visual inspections of the oral cavity have been proposed for the assessment.
Objective To identify whether photographs of the tongue could be used to identify oral dryness.
Material and methods Twenty-five dentists and 25 individuals with another academic background were recruited. They assessed the severity of the oral dryness of 50 patients, based on an intraoral picture of each patient. The oral dryness was quantified with a five-point Likert scale and the scores were subsequently compared with the salivary flow rate and the level of xerostomia of these patients.
Results No relation was found between the unstimulated salivary flow rate of a patient and the average oral dryness score, determined by dentists (p = 0.260) as well as non-dentists (p = 0.806). Also no relation was found between the self-reported xerostomia level of the patient and the average dryness score assessed by the dentists (p = 0.171) or non-dentists (p = 0.477).
Conclusion It does not seem possible to diagnose oral dryness by mere visual inspection of photographed tongues. Thus, for correct diagnosis of oral dryness further clinical investigation of the oral cavity and collection of saliva is indicated.
Similar content being viewed by others
Introduction
Saliva is of vital importance to maintain oral health. A lack of saliva may cause severe feelings of oral dryness and increases risk of developing caries and oral inflammation. In addition, problems with eating, speech and swallowing may occur.1 The main causes of oral dryness are the use of medication, systemic disorders such as Sjögren's syndrome, and head and neck radiotherapy.2,3,4
Xerostomia is the subjective feeling of a dry mouth experienced by the patient5 and can be assessed either by asking the patient or by using dry mouth questionnaires such as the xerostomia inventory (XI).6 Hyposalivation can be defined as the objective measurement of reduced salivary flow rates. Patients with a reduced saliva secretion rate do not necessarily suffer from xerostomia.7
Quantification of the unstimulated, chewing stimulated and citric acid stimulated saliva secretion rates is hardly ever done in the dental practice, as many dentists consider it as time consuming and disturbing the daily routine.
Therefore, several chairside tests have been developed to assess a dry mouth in a clinical setting more quickly. For example, the amount of saliva on the oral mucosa can be measured with the moisture checker for mucus, a device that measures the weight percent of water content in the oral mucosal epithelium. Another device to measure the wetness of the mucosa is the L-Salivo wetness tester.8,9 Another option to measure the amount of saliva in the mouth is the candy weight loss test. This test measures the weight of a candy before and after placing in the mouth.10 Also the Schirmer test, normally used to test dryness of the eyes by paper strips, can be used to measure the absorption of oral fluid with paper strips.11 More recently, a new test has been proposed to access oral dryness by a clinical and visual inspection of the oral cavity, which includes the presence of frothy saliva, the dryness of the oral mucosa or lips and stickiness of the dental mirror to the tongue or the buccal fold.12 However, it remains unclear whether a visual photographic and clinical inspection of the oral cavity could potentially identify dryness of the mouth. Therefore, the aim of this study was to identify whether a visual assessment of the tongue by means of photographs could be potentially useful to diagnose oral dryness.
Material and methods
Twenty-five dentists were recruited using a snowball sampling procedure, in which dentists recruited future subjects among their dental colleagues. Oral-maxillofacial surgeons were not included in the study. As a control group, 25 subjects with an academic degree other than dentistry or medicine were recruited among relatives of staff members of the Academic Centre for Dentistry Amsterdam (Table 1).
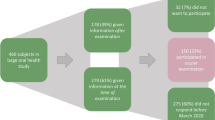
For this study we used data of patients on haemodialysis, previously collected during a research project on oral health and saliva in chronic renal failure. In total 50 photographs of tongues were randomly selected out of the original data set (n = 94) and displayed in a random order.13,14,15 During that study, unstimulated whole saliva was collected using the spitting method over a 5 minute period during which all the saliva was spat out every 30 seconds into a cup. The unstimulated salivary flow rate (USFR) was determined gravimetrically (assuming 1 g = 1 ml). Perceived xerostomia was assessed using the xerostomia inventory (XI).16 This questionnaire contains 11 questions regarding dry mouth and uses a five-point Likert scale. Examples of items from the xerostomia inventory are 'My mouth feels dry', 'I have difficulty in eating dry foods' and 'I sip liquids to aid in swallowing food'. Individual answers to the 11 questions were computed and used to create an individual XI-score varying from 11 (no dry mouth) to 55 (extreme dry mouth). In addition, intraoral pictures were taken of each patient under standardised circumstances and camera-settings.
Randomly selected intraoral pictures of 50 different patients (Fig. 1 demonstrates for two typical examples) were sent to the participants as a PowerPoint presentation on a CD-ROM. Two different versions of the CD-ROM were made, with the same set of pictures but in different sequence. The participants were instructed to view each picture for 10 to 15 seconds before judging the oral dryness on a five-point Likert scale (one = very dry; two = relatively dry; three = not dry, not wet, four = quite wet; five = very wet). After assessment of the 50 intraoral pictures, the participants were asked whether they had paid special attention to specific aspects of the tongue to quantify the level of oral dryness (Table 2). Finally, the subjects were asked whether they think it is possible to determine oral dryness by judging photographs of the tongue.
The data are presented as mean ± SD or percentages and were analysed with IBM SPSS Statistics for Windows, version 20.0 (IBM Corp, Armonk NY, USA) using Mann Whitney U test, Wilcoxon tests and chi square tests. Potential associations between the estimated oral dryness, unstimulated saliva flow rate (UFSR) and xerostomia index score were explored with Spearman's rank order correlation coefficients. P-values <0.05 were considered statistically significant.
Results
Twenty-five dentists (mean age 37.4 ± 11.6 years) and 25 controls with a non-medical academic degree (mean age 41.7 ± 11.0 years) participated. The dentists group consisted of 10 males and 15 females; the control group consisted of 15 males and 10 females. No statistical significant differences were found for gender or age between the two experimental groups.
The average clinical experience of the dentists was 12.3 ± 11.6 years (range 1–44 years), and their average number of clinical hours was 27.7 ± 9.6 hours per week. Thirty-two percent of all recruited dentists (n = 8) had followed a post-academic course on saliva.
The average USFR of the 50 patients, whose tongue pictures were used in the study, was 0.32 ± 0.24 ml/min (range 0.04–1.42 ml/min) and the average XI-score of the patients was 24.2 ± 9.5 (range 11-51). The overall average of the mean scores of oral dryness based on each intraoral picture was 2.89 ± 0.45 (range 1.94–3.78). The average scores of the extent of oral dryness as determined by dentists (2.85 ± 0.41) were not significantly different from the scores by controls (2.93 ± 0.57, Wilcoxon test p = 0.333). A significant correlation was found between the mean scores of the 50 intraoral pictures as determined by dentists and non-dentists (r = 0.647; p <0.005).
No significant differences in scores were observed between intraoral pictures of the patients with hyposalivation (USFR ≤0.10 ml/min, n = 12) and those with a normal USFR (USFR ≥0.50 ml/min, n = 10), (2.79 ± 0.48 versus 2.80 ± 0.56, Mann Whitney U test, p = 0.869). No significant relationship was found between a patient's USFR and his/her average oral dryness score as determined by either dentists or non-dentists (p = 0.260 and p = 0.806, respectively) (Fig. 2). Similarly, no significant relationship was found between a patient's self-reported xerostomia score and his/her average oral dryness score as determined by either dentists or non-dentists (p = 0.171 and p = 0.477, respectively) (Fig. 3).
No significant difference was found in the scoring of the intraoral pictures between dentists that had followed a course on saliva and those who had not (2.90 ± 0.55 versus 2.83 ± 0.40 respectively, Wilcoxon test p = 0.176). Dentist with more than 8 years of clinical experience (n = 12) ranked the intraoral pictures, on average, with slightly higher scores than dentists with less than 8 years of clinical experience (n = 13) (2.89 ± 0.37 versus 2.82 ± 0.48, Wilcoxon test p = 0.04).
No significant differences were found between the dentists and non-dentists with regard to the criteria used to assess oral dryness, such as fissures, colour, brilliance, tongue coating and tongue impression (Table 2). All dentists used the brilliance of the tongue as an indication to assess oral dryness. Spontaneously reported additional criteria for determining oral dryness were: wetness, appearance of saliva, frothy saliva, presence of papillae, swelling or impairment of the tongue, a hairy tongue.
Most dentists reported that they perform a general inspection of the mucosa of the tongue during each dental check-up (84%, n = 21). Fifty-two percent of the dentists (n = 13) assess oral dryness during a regular dental check-up, and of those, two dentists (15%) reported that they looked at the tongue to assess oral dryness.
Discussion
To our knowledge, this is the first study to investigate the value of visual inspection of photographs of tongues to assess oral dryness. No correlation existed among a patient's USFR, the self-reported level of xerostomia, and the oral dryness score as determined by visual assessment of photographs. There was also no difference between the scores as determined by either dentists or non-dentists.
The years of clinical experience of dentists could potentially play a role in their ability to assess the oral dryness of the tongue. Crespo et al.17 found in 2004 that recently graduated clinicians needed additional information in the determination of a diagnosis such as dental radiographs or laboratory test results to draw the same conclusions as capable, experienced dentists. In the present study, however, no relation was observed between the years of clinical experience and the correct assessment of oral dryness after looking at the picture of the tongue.
Dentists who reported to inspect the tongue of patients during dental check-ups on a regular basis did not perform better than the other dentists. These results are in accordance with an earlier investigation in which pictures of the tongues of twins had to be matched. In that study also no difference was found among experienced dentists, less-experienced dentists, and tongue experts compared to individuals not affiliated with any biomedical institution.18
In our study, the observers mentioned several aspects and criteria related to the tongue that aid in the diagnosis, such as humidity and amount of saliva. Glossiness and reflections of the tongue could have given the observers the impression that saliva was present in the oral cavity. Although the intraoral pictures in our research were taken under standard conditions it is still possible that differences in reflections may have affected the oral dryness score of the observers.
In the present study, the intraoral pictures were not assessed under standard conditions as all observers looked at the pictures at their own computer. The light and colour adjustments could have been different between the observers.
Another limitation of our study is that we only used intraoral pictures of chronic renal failure patients treated with haemodialysis. However, previously we have reported that the oral health of these dialysis patients is comparable to that of healthy controls. Therefore, these pictures may be representative for the general population.13
A relatively large proportion of the participating dentists (32%) had followed a post-academic course in saliva and salivary disorders. This might implicate that some participants in the present investigation had a greater interest in salivary disorders and oral dryness. Nevertheless, no relationship was found in the scoring of the intraoral pictures and whether or not a dentist had taken continuing education courses related to saliva.
In the present study, we used a five-point Likert scale to score the severity of the dryness of the tongue. An advantage of this scale is that it is easy to understand. A disadvantage of a five-point Likert scale is that it has a tendency for scores towards the middle instead of scores at the extremes. It has been advocated that visual analogue scales (VAS) are better able to detect small differences.19
Despite these limitations, our data suggest that an intraoral picture of the tongue cannot be used as the sole basis on which to assess the severity of oral dryness. The majority of the participants mentioned that additional information about the surrounding tissues of the oral cavity is needed for a correct diagnosis. It is conceivable that the additional information may be provided through the use of the recently developed Clinical Oral Dryness Index12 that includes several other clinical aspects of oral dryness such as stickiness of a dental mirror to the tongue or cheek and glossiness of the tongue.
In conclusion, our study suggests that a general practitioner is not able to diagnose a dry mouth by mere visual inspection of a photograph alone. To diagnose hyposalivation objectively further clinical investigation of the oral cavity and collection of both unstimulated and stimulated saliva is indicated.
References
Amerongen A V, Veerman E C . Saliva-the defender of the oral cavity. Oral Dis 2002; 8: 12–22.
Karlsson G . The relative change in saliva secretion in relation to the exposed area of the salivary glands after radiotherapy of head and neck region. Swed Dent J 1987; 11: 189–194.
Vissink A, Spijkervet F K, Kalk W W, van Nieuw Amerongen A, Bootsma H, Kallenberg C G . Sjögren's syndrome. Consequences for oral health. Ned Tijdschr Tandheelkd 1997; 104: 458–462.
Vissink A, Kalk W W, Mansour K et al. Comparison of lacrimal and salivary gland involvement in Sjögren's syndrome. Arch Otolaryngol Head Neck Surg 2003; 129: 966–971.
Sreebny L M . Saliva in health and disease: an appraisal and update. Int Dent J 2000; 50: 140–161.
Sreebny L M, Vissink A . Dry mouth. The malevolent symptom: a clinical guide. Ames: Wiley-Blackwell, 2010.
Márton K, Madléna M, Bánóczy J et al. Unstimulated whole saliva flow rate in relation to sicca symptoms in Hungary. Oral Dis 2008; 14: 472–477.
Yamada H, Nakagawa Y, Nomura Y et al. Preliminary results of moisture checker for Mucus in diagnosing dry mouth. Oral Dis 2005; 11: 405–407.
Kakinoki Y, Nishihara T, Arita M, Shibuya K, Ishikawa M . Usefulness of new wetness tester for diagnosis of dry mouth in disabled patients. Gerodontology 2004; 21: 229–231.
Yamamoto K, Matsusue Y, Komatsu Y, Kurihara M, Nakagawa Y, Kirita T . Association of candy weight loss rate with whole saliva flow rates. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011; 112: 10–14.
Chen A, Wai Y, Lee L, Lake S, Woo S . Using the modified Schirmer test to measure mouth dryness: a preliminary study. J Am Dent Assoc 2005; 136: 164–170.
Osailan S M, Pramanik R, Shirlaw P, Proctor G B, Challacombe S J . Clinical assessment of oral dryness: development of a scoring system related to salivary flow and mucosal wetness. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 114: 597–603.
Bots C P, Poorterman J H, Brand H S et al. The oral health status of dentate patients with chronic renal failure undergoing dialysis therapy. Oral Dis 2006; 12: 176–180.
Bots C P, Brand H S, Poorterman J H et al. Oral and salivary changes in patients withend stage renal disease (ESRD): a two year follow-up study. Br Dent J 2007; 27: 202.
Bots C P, Brand H S, Veerman E C et al. Acute effects of haemodialysis on salivary flow rate and composition. Clin Nephrol 2007; 67: 25–31.
Thomson W M, Chalmers J M, Spencer A J, Williams S M . The Xerostomia Inventory: a multi-item approach to measuring dry mouth. Community Dent Health 1999; 16: 12–17.
Crespo K E, Torres J E, Recio M E . Reasoning process characteristics in the diagnostic skills of beginner, competent, and expert dentists. J Dent Educ 2004; 68: 1235–1244.
Spielman A I, Brand J G, Buischi Y, Bretz W A . Resemblance of tongue anatomy in twins. Twin Res Hum Genet 2011; 14: 277–282.
du Toit R, Pritchard N, Heffernan S, Simpson T, Fonn D . A comparison of three different scales for rating contact lens handling. Optom Vis Sci 2002; 79: 313–320.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bots, C., Beest, A. & Brand, H. The assessment of oral dryness by photographic appearance of the tongue. Br Dent J 217, E3 (2014). https://doi.org/10.1038/sj.bdj.2014.597
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.597
This article is cited by
-
Oral micro-electronic platform for temperature and humidity monitoring
Scientific Reports (2023)
-
Clinical assessment
British Dental Journal (2014)