Key Points
-
Provides a historical overview of microscope use in dentistry.
-
Explores the importance of microscopy in dentistry.
-
Highlights the benefits of using a microscope over loupes.
Abstract
The different aspects of treatment of periodontal disease and mucogingival defects all require an accurate diagnosis in addition to good control and precision during therapeutic procedures. Magnification aids and microsurgery, combined with minimally invasive techniques, can best meet these requirements. The suitability of treatment, the healing time, pain levels and postoperative scarring are all improved and the patient benefits.
Similar content being viewed by others
Background
Microscopy (from Greek scopein 'to see' and micro 'small'), is defined as the action of looking at very small objects or entities, using magnification tools, particularly the microscope, invented during the sixteenth century by Galilee Galileo.boxed-text
It was not until the nineteenth century that the first use of microscopy in clinical medicine was reported, and the first microscope-assisted surgery is traditionally attributed to Nylen, for an otologic surgery in 1922.1 Since then, microscope-assisted medicine has experienced an exponential interest, especially in those fields involving the most noble and delicate organs, such as neurovascular surgery, ophthalmic surgery, or ear-nose-throat surgery.
Paradoxically, interest in microscopy took many more decades to reach dental medicine, even though the tininess of the structures to treat, and the degree of precision required for those treatments, seemed to call for immediate awareness of its potential. Many reasons could explain this relative disinterest. The first one would probably be the 'non-essential' aspect of the dental organs, which contributed for a long time to a certain disaffection of the population for treatments considered painful and costly. At a time when extractions were the cure of choice, using a microscope was obviously very remote from the immediate preoccupations of dentists. Thus, it was not before the late 70s, early 80s, that microscopy was used in dentistry.2,3,4
Under the combined thrust of spectacular progress in dental medicine over the last decades, and an increasing media pressure stressing body health and beauty, patients have consented to greater efforts, not only to save teeth they would formerly have allowed to be extracted, but also to improve their smile as much as possible. Dentists have not been let down in this development, finding in this new trend a way to increase their knowledge and professional satisfaction, as well as their income.
'Cosmetic dentistry' becomes a specialty in itself and numerous professional organisations, entirely devoted to that category of elective treatments, have appeared and are thriving. The impact of cosmetic dentistry is so strong that a number of dentists exclusively dedicate their time to it, and it is not uncommon to see treatment plans established only under those considerations, even though the patient does not present with any pathology.
The other side of the coin is the increasing expectations from the patients in terms of outcome: the concept of obligation of means has been replaced by obligation of results, requiring dentists to constantly surpass themselves.
Meanwhile, benefits of minimally invasive surgery are widely advertised by the media. Many articles or documentaries report more and more targeted surgeries, such as laparoscopies or joint surgeries, requiring incision of only a few millimetres, when in the past, scars ten fold bigger where expected.5 Besides the considerable reduction of the aesthetical damage, these techniques allow patients not only to enjoy surgeries with much less post-operative pain and complications, but also a much shorter stay at the hospital, apparently directly proportional to the length of the scar! Thus the thought of going through such surgeries becomes much less worrying, and acceptation of the treatment by the patient is greatly increased.
Simultaneously, access to information has become simpler, and patients do not fail to investigate (though this is often misleading), before they consult a health professional, expecting him to know and use all the latest trends and gimmicks.
The combined effect of those changes and the will of a few pioneers to improve their treatments, such as Noah Chivian, or Dennis Shanelec, led to the birth of microdentistry in the 80s/90s. It was mostly in endodontics, under the initial thrust of Noah Chivian, and later Gary Carr, that this technique emerged; probably because vision in the root canals, remarkably small and poorly lit, was virtually impossible and everything was traditionally done under tactile control, which more than often would deceive the operator. Moreover, the endodontist works generally on only one tooth and under only one axis for a given treatment, and just occasionally needs to move the patient or the microscope, considerably simplifying the use of the latter. Thus, this magnification tool has been relatively easily adopted in practices specialising in endodontic treatments. Learning how to use it has incidentally been made mandatory by the American Association of Endodontists in speciality programmes in the US since 1998.6 Many research articles have shown the advantages of using a microscope during endodontic treatments, in particular when it comes to discovering and locating canals, previously considered supernumerary (MB2) and regarded today as being the norm.7,8,9
Apart from in endodontics, more than 30 years after its first use in dentistry microscopy has still not established a firm toehold in our therapeutic arsenal. Only a few practitioners use it in periodontal mucogingival surgery, and even less in restorative dentistry. It was not until 2010, in North America, that the first accredited pre-graduated course of microdentistry appeared, created at the University of Montreal by the first author of this article, and even then only accessible to a few hand-picked students (Fig. 1).
The possible reasons for this relative disaffection are probably the steep learning curve of the technique and the acquisition cost of the microscope, an investment that does not directly generate an increase of income. In addition, the lack of serious scientific publications (except in endodontics) whether for the patient or for the dentist confirming the advantages of using a microscope, does not contribute to promoting this tool. Indeed, the majority of the articles in professional journals are anecdotal in nature, and the few research articles available present major bias, making any interpretation of the results sensitive.10,11,12 But the main reason for the limited development of a technique otherwise fiercely supported by its users is probably a lack of information at the practitioners' level. The purpose of this article is precisely and emphasise the advantages the dentists can get from magnification in general, and from the microscope in particular.
The necessity of magnification in odontology
The structures the dentists have to work on, teeth or periodontium, are exceedingly small. Moreover, the causal agents of the main buccal pathologies (caries and periodontal disease) are bacteria, only a few micrometres large.
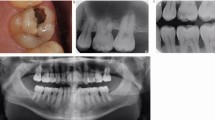
Diagnosis of periodontal disease, or caries, is essentially carried out by vision, assisted or not by examination of radiographs. As a matter of fact, it has been demonstrated that tactile sense does not significantly influence the precision of the diagnosis of carious lesions.13,14 These lesions should be treated at a very early stage, ideally even before a cavity appears.15 Such timely treatments require the use of remineralisation techniques, avoiding any unnecessary sacrifice of tooth substance. In addition, evaluation of the activity of the carious lesion is also done using visual criteria; it is a decisive aspect of the diagnosis, when choosing the best therapeutic option. Increasing the visual capacity of the operator should therefore potentially reduce the number of operative treatments (Figs 2a and b). At higher magnification, many signs of inactivity of the lesion (dark colour, shininess, no retention of dental plaque) encourage postponement of such operative treatment, as long as the caries risk does not change. On the other hand, some studies have demonstrated an inclination of certain operators toward over-zealous treatment when high magnification is used.16,17,18 Thus, a specific education in diagnostics under magnification seems to be indicated.
If a treatment is nevertheless required, using burs of extremely small size and adhesive material can limit the extent of the intervention as much as possible. That is if the diagnosis has been done in time, and if the operator masters the exacting bonding techniques and knows how to control those sensitive instruments. Incidentally, a crack or a root fracture can greatly influence the choice of such treatment.19 Here again, vision is the primary mean to assess the presence and the span of those defects, which can lead to the very loss of the tooth (Fig. 3). It is thus reasonable to infer that improving vision would allow for a more refined diagnosis and better control of those sensitive procedures.
In spite of its exceedingly small size, a craze line at the cervical level was immediately detected when observed under high magnification, even before removing the prosthetic crown. It is the torque applied during the extraction that opened the crack, to a point that the tooth separated in two halves
For prosthetic treatments, if the susceptibility of the host is not taken into account, it seems that a marginal gap of no more than 40 to 100 micrometers between the tooth and the restoration should be achieved to be clinically acceptable for the periodontium and to prevent secondary caries (Fig. 4).20 Even more, the proprioception of the teeth and the tongue allow to perceive differences in thickness or rough spots greatly under 20 μm.21,22 Thus, a refined preparation, an accurate occlusal adjustment and a high degree of polish are essential for the dental health and the comfort of the patient. Here again, the degree of precision required immediately calls for magnification.
In periodontics, the importance of the initial phase of the treatment has been emphasised many times,23,24 but it also has been demonstrated that, regardless of the efforts of the operator, the complete elimination of the calculus in the pockets is not possible, especially when done without surgical access.25 If a surgical access is managed, vision of the surfaces needing to be cleaned is improved, and so is the elimination of the calculus deposits, even though it is not yet totally satisfactory.26 The improvement of results under surgical access can be chiefly attributed to better visibility, making it tempting to suggest that enhancing vision even further would lead to still better results.27,28,29
Periodontal mucogingival surgery has evolved tremendously over the last two decades, sanctioned by increasingly spectacular aesthetic outcomes.30 More and more case reports where microsurgical techniques were used, show success in procedures which were until then highly unpredictable, such as recreating gingival papillae with a graft procedure.31 These procedures are performed using instruments and sutures of extremely small size, as well as gestures of a span of only a few tenths of a millimetre. A few operators even choose to carry out procedures as common as a connective tissue graft with the same kind of instruments, and close their incision lines with 7-0 or 8-0 sutures, sometimes 9-0, while conventional techniques and 4-0 or 5-0 Vicryl is still the standard for many. Further examples of such microsurgeries will appear later in this series, when looking at the contribution of the microscope to periodontics.
Preserving healthy dental tissues during our actions is an unavoidable prerequisite of primum non nocere. Damaging the dentine, the cement, or the epithelial attachment during an intra-sulcular preparation (which willingly becomes subgingival), or during a surfacing, are collateral damages just too easily accepted by the dentists. Similarly, numerous studies have shown an alarming rate of 60–100% of adjacent teeth damaged throughout preparations including a proximal surface.32,33,34 During sinus-lift procedure by lateral approach (Caldwell-Luc), studies report tears of the Scheiderian membrane in 30% of the cases, not considering tears that might have been left undetected but could nonetheless compromise the success of the graft.35,36
Rather than leniency of the health professional, one can possibly blame poor visibility for such unsatisfactory results. In fact, the theoretical visual acuity of the human eye is about 70 μm, but vision taking place in a gaseous environment (the air), diffraction and refraction reduce it to about 150-200 μm. In dentistry, these values can be compromised even further by the low luminosity in the buccal cavity. Moreover, the diopter of the eye (corresponding to the power of the corneal lens) decreases as the operator gets older. The operator then needs to increase the distance between them and the object they are looking at, thus reducing visual acuity.37,38 Even if the operator could manage to see from a close distance, this would be done to the detriment of working-posture and vision, for they would have to lean over the patient and inflict an important accommodation strain to the eyes (Fig. 5). It is incidentally a recurrent problem within the profession, where musculoskeletal and eye problems are more frequent than average.39,40,41
Loupes, thanks to their magnification factor, allow reducing this detrimental pattern. But this magnification factor being limited, and the look still being aimed at the operating field, the operator nonetheless presents non-physiological curves in the spine, specially at the cervical level, and needs to activate many paravertebral muscles to maintain this posture, with his or her head leaning forward. With the microscope, the dentist can assume a completely physiological posture, the head vertical to the spine, allowing for an optimal comfort. A high-quality operating seat with armrests (not available for that photography), would improve comfort even further
Considering all the examples above, underlining the importance of good vision and the necessity of controlling procedures down to a scale of a few micrometres, it is obvious that a visual acuity of about 200 μm is not sufficient to achieve the required degree of precision. Magnification tools thus have great potential and their increasingly frequent use (loupes) by dentists makes them ipso facto a new standard of care. Of course, it is not enough for the dentist to use a magnification tool to claim that he or she is practising microdentistry. Microdentistry can exist only if both concepts of minimally invasive and minimally interventionist dentistry coexist with such use. It would be fanciful to believe that we are micro-surgeons if the necessity of the procedure itself has not been established, or if the span of the intervention, because of inappropriate concepts or technical skills, extends beyond what is required in terms of histopathology and biomechanics. Other articles in this series extensively present those concepts.
As a matter of fact, magnification tools will definitely not compensate for insufficient knowledge or inappropriate technique of the operator. On the contrary, the additional training required to work under magnification can accentuate those weaknesses. Under magnification an over-zealous treatment is also a risk for operators believing that anything deviating from the norm should be treated, even if those deviations would have no or only little effect on the patient's health.16,17,18 A few articles actually demonstrate the tendency of their very authors to lean toward such failing.42
It is nonetheless true that making vision better, by the mean of magnification tools, seems to improve both diagnostics and execution of the procedure. Enhancing diagnostics directly favours the concept of minimally interventionist dentistry, as enhancing the design and execution of the procedure allows for minimally invasive dentistry. That is, if the operator has a clear mental grasp on the objectives of the procedure and the means to carry it out. Moreover, besides improving vision, working under magnification also increases the neuro-muscular control of the operator.43,44
Comparison between loupes and microscopes
Based on the need for magnification, loupes are increasingly frequently used by dentists, to a point that they are becoming a standard of care. In a poll from the Clinical Research Association in 2006, 86% of the dentists claimed they were using loupes on a regular basis. Indeed, using loupes has even been made mandatory in certain colleges of dentistry in North America and probably elsewhere. The description of the different types of loupes (simple, Galilean, or Keplerian) is beyond the scope of this article, but the reader can refer to an excellent review of Dr D. Shanelec45 for more details. It is sufficient to say that those three types of loupes share common features, such as a single degree of magnification, a binocular vision with optics converging toward the focal length, and the necessity for the eyes of the operator to converge and accommodate (Fig. 6). Their main advantages are a reasonable cost, a relatively flat learning curve and manoeuvrability, yet all these advantages decrease when the quality of the loupes and the level of magnification increase. In fact, the advantages of the loupes are directly linked to their very shortcomings.
As for microscopes, if they are more cumbersome, more expensive and more difficult to use, (Fig. 7) they are more precise and thus these qualities make them superior to loupes in virtually all situations.
It can be mounted on a wheelbase (as in this photography), or preferably hung to the ceiling like the operating light, or attached to the wall. Here, the ProErgo model, from Zeiss, presents advanced features, making its use more practical (variable focal length, electromagnetic brakes controlled by a simple finger pressure to assist the motion of the head, high intensity Xenon light, etc)
Optical advantages
Thus, microscopes offer a magnification ranging from 3× to 20× or more depending on the model. Despite being associated with a heavier and more expensive optical system, this versatility enables work with the optimal degree of magnification, depending on the type or the stage of the procedure. It is erroneous to think that the higher the magnification, the better. In fact, the higher it is, the less depth of field, field of vision, and luminosity are available for the operator. It is therefore preferable to work with the smallest magnification possible, which still authorises complete control of the gesture. For instance, a very high magnification would not be adapted to a long sulcular incision, because of the associated lack of depth of field, and restricted field of vision, making framing and focusing a difficult, if not impossible task. By the same token, securing a subpapilla graft with a 9-0 suture could hardly be done with only 2.5× magnification. Accordingly, the dentist working with loupes would need to change them many times throughout a procedure according to his/her needs, with all related problems in terms of fluidity of work, ergonomics, asepsis, and increased cost for the many pairs of loupes and lighting systems required.
The optics of the microscope are larger, thus heavier and more expensive that loupes, but also of better quality. At the same magnification, a microscope provides a better image than loupes: increased depth of field, field of vision, luminosity, resolution and sharpness, decreased distortions and spherical and chromatic aberrations.
Because of the reflection of light at the lenses level and the smaller aperture required for magnification, the latter is associated with a loss of luminosity approximately proportional to its square (if one accepts some rough simplifications). Thus, for a 6× magnification, it takes 36 times more light to illuminate the object properly. Otherwise magnification, rather than improving vision, would reduce it! Loupes can supply such light only if they are complemented by an illumination system. This increases their cost as well as their weight, reducing the comfort of the operator, even more so since the light is often connected to the frame of the loupes with an offset axle. This leverage is directly supported by the bridge of the nose, which becomes readily tender at the end of the day. Helmets have been proposed to overcome this problem, but the system becomes more cumbersome, losing part of its appeal (Fig. 8). In the case of the microscope, the light generator is built-in. Its variable intensity covers the different light requirement as magnification varies from low to high. For the most advanced microscopes (Fig. 7), a powerful xenon light is available, with its intensity varying automatically with the magnification used.
Nevertheless, working under high magnification in those conditions is made difficult by the restricted field of vision, and depth of field. The slightest motion of the head of the operator will throw him out of focus or out of frame (whereas for the microscope, the optics are not connected to the head, and hence, micromotions of the latter have no impact on vision). Moreover, with loupes, the eyes endure a constant strain because they still need to converge and to accommodate
Ergonomic advantage
Because of its more static design, the microscope deters the operator or the patient from constant positions shifts, and thus forces the dentist into better management of the ergonomic sequencing of their work. But ergonomics are improved by two fundamental aspects:
-
When working under microscope the dentist looks right in front of him/her, and not at the operating field, and can thus keep an upright position, getting rid of all non-physiological curves of his or her spine (Figs 1 and 5). Certain high-end microscopes (Fig. 7) even propose a variable focal length, allowing the operator to assume an ideal posture for the entire duration of the procedure without having to worry about keeping the operating field (and thus the patient) at a specific distance from the lens. Given the high prevalence of back pain among the profession, this argument alone would justify using the microscope on a regular basis.
-
Secondly, and chiefly, unlike loupes with their converging optics, the optics of a microscope are parallel, aligned with the axis of vision at infinity (Fig. 9). The eyes of the operator do not need to converge or to accommodate; which completely removes any strain from them, even when using the highest magnification. Where loupes eventually generate eye fatigue, sometimes even headaches, especially for the most powerful of them, microscopes can take the dentist to the end of the day with perfectly relaxed eyes, while offering the best vision possible in a comfortable posture, favouring quality of care and pleasure at work.
Practical advantage
Another advantage of the microscope over loupes is its capacity to easily generate a pre-, per-, and post-operative iconography of the treatments. In fact, most models can be equipped with either a camera or a video camera of standard or high definition. These tools allow the dentist to gather images, with no interruption in the ergonomic stream of their work (Figs 1 and 10) With the increasing importance of imagery in dentistry for medico-legal, as well as pedagogical reasons, but also as a communication tool with patients, colleagues, or laboratory technicians, being able to collect those images without interrupting the work flow is an obvious financial and ergonomic advantage.
Advantage in terms of impact at patient level
Even though the microscope is more expensive than loupes, it has an important psychological impact on the patients, who associate it with greater competence, quality of care and trust in their dentist (Table 1). Therefore, it carries a marketing value that will help promote the practice, thus indirectly compensating for its cost.
Conclusion
The rational for the need of magnification in dentistry now seems well understood by dentists. Not only does magnification potentially improve ergonomics and diagnostics, but also endows the operator with enhanced vision, allowing him or her to use smaller instruments and much less invasive procedures. This contributes to less morbidity and more comfort for the patient. Magnification even makes it possible to consider certain treatment options that would otherwise not have been feasible. If loupes are still the magnification tool most frequently used by dentists, the numerous advantages of the much more powerful and versatile microscope are worth the time and energy required to master new techniques and any practitioner will surely wonder how they worked without it before!
References
Dohlman G F . Carl Olof Nylen and the birth of the otomicroscope and microsurgery. Arch Otolaryngol 1969; 90: 813–817.
Apotheker H . The applications of the dental microscope: preliminary report. J Microsurg 1981; 3: 103–106.
Apotheker H, Jako G J . A microscope for use in dentistry. J Microsurg 1981; 3: 7–10.
Ducamin J P, Boussens J . Surgical microscope (SM) in dentistry. Rev Odontostomatol 1979; 8: 293–298.
Way L W . Changing therapy for gallstone disease. N Engl J Med 1990; 323: 1273–1274.
Association CODAAD. Standards for advanced speciality educations programs in endodontics. Implementation Date: January 1st, 1998, Chicago/1996. p. 26.
Buhrley L J, Barrows M J, BeGole E A, Wenckus C S . Effect of magnification on locating the MB2 canal in maxillary molars. J Endod 2002; 28: 324–327.
Hartwell G, Appelstein C M, Lyons W W, Guzek M E . The incidence of four canals in maxillary first molars: a clinical determination. J Am Dent Assoc 2007; 138: 1344–1346.
Yoshioka T, Kikuchi I, Fukumoto Y, Kobayashi C, Suda H . Detection of the second mesiobuccal canal in mesiobuccal roots of maxillary molar teeth ex vivo. Int Endod J 2005; 38: 124–128.
Cairo F, Carnevale G, Billi M, Prato G P . Fibre retention and papilla preservation technique in the treatment of infrabony defects: a microsurgical approach. Int J Periodontics Restorative Dent 2008; 28: 257–263.
Cortellini P, Tonetti M S . Microsurgical approach to periodontal regeneration. Initial evaluation in a case cohort. J Periodontol 2001; 72: 559–569.
Francetti L, Del Fabbro M, Calace S, Testori T, Weinstein R L . Microsurgical treatment of gingival recession: a controlled clinical study. Int J Periodontics Restorative Dent 2005; 25: 181–188.
McComb D, Tam L E . Diagnosis of occlusal caries: Part I. Conventional methods. J Can Dent Assoc 2001; 67: 454–457.
Newbrun E . Problems in caries diagnosis. Int Dent J 1993; 43: 133–142.
Tyas M J, Anusavice K J, Frencken J E, Mount G J . Minimal intervention dentistry-a review. FDI Commission Project 1–97. Int Dent J 2000; 50: 1–12.
Akarslan Z Z, Erten H . The use of a microscope for restorative treatment decision-making on occlusal surfaces. Oper Dent 2009; 34: 83–86.
Erten H, Uctasli M B, Akarslan Z Z, Uzun O, Semiz M . Restorative treatment decision making with unaided visual examination, intraoral camera and operating microscope. Oper Dent 2006; 31: 55–59.
Whitehead S A, Wilson N H . Restorative decision-making behaviour with magnification. Quintessence Int 1992; 23: 667–671.
Bader J D, Shugars D A, Martin J A . Risk indicators for posterior tooth fracture. J Am Dent Assoc 2004; 135: 883–892.
Kern M, Schaller H G, Strub J R . Marginal fit of restorations before and after cementation in vivo. Int J Prosthodont 1993; 6: 585–591.
Jones C S, Billington R W, Pearson G J . The in vivo perception of roughness of restorations. Br Dent J 2004; 196: 42–45.
Van Noort R . Controversial aspects of composite resin restorative materials. Br Dent J 1983; 155: 380–385.
Lindhe J, Nyman S . Long-term maintenance of patients treated for advanced periodontal disease. J Clin Periodontol 1984; 11: 504–514.
Lindhe J, Westfelt E, Nyman S, Socransky S S, Haffajee A D . Long-term effect of surgical/non-surgical treatment of periodontal disease. J Clin Periodontol 1984; 11: 448–458.
Kepic TJ, O'Leary T J, Kafrawy A H . Total calculus removal: an attainable objective? J Periodontol 1990; 61: 16–20.
Wylam J M, Mealey B L, Mills M P, Waldrop T C, Moskowicz D C . The clinical effectiveness of open versus closed scaling and root planing on multi-rooted teeth. J Periodontol 1993; 64: 1023–1028.
Belcher J M . A perspective on periodontal microsurgery. Int J Periodontics Restorative Dent 2001; 21: 191–196.
Hegde R, Sumanth S, Padhye A . Microscope-enhanced periodontal therapy: a review and report of four cases. J Contemp Dent Pract 2009; 10: E088–E096.
Kwan J Y . Enhanced periodontal debridement with the use of micro ultrasonic, periodontal endoscopy. J Calif Dent Assoc 2005; 33: 241–248.
Shanelec DA . Anterior esthetic implants: microsurgical placement in extraction sockets with immediate plovisionals. J Calif Dent Assoc 2005; 33: 233–240.
Nordland W P, Sandhu H S, Perio C . Microsurgical technique for augmentation of the interdental papilla: three case reports. Int J Periodontics Restorative Dent 2008; 28: 543–549.
Lussi A, Gygax M . Iatrogenic damage to adjacent teeth during classical approximal box preparation. J Dent 1998; 26: 435–441.
Medeiros V A, Seddon R P . Iatrogenic damage to approximal surfaces in contact with Class II restorations. J Dent 2000; 28: 103–110.
Qvist V, Johannessen L, Bruun M . Progression of approximal caries in relation to iatrogenic preparation damage. J Dent Res 1992; 71: 1370–1373.
Cho S C, Wallace S S, Froum S J, Tarnow D P . Influence of anatomy on Schneiderian membrane perforations during sinus elevation surgery: three-dimensional analysis. Pract Proced Aesthet Dent 2001; 13: 160–163.
Zijderveld S A, van den Bergh J P, Schulten E A, ten Bruggenkate C M . Anatomical and surgical findings and complications in 100 consecutive maxillary sinus floor elevation procedures. J Oral Maxillofac Surg 2008; 66: 1426–1438.
Haegerstrom-Portnoy G, Schneck M E, Brabyn J A . Seeing into old age: vision function beyond acuity. Optom Vis Sci 1999; 76: 141–158.
Werner J S, Peterzell D H, Scheetz A J . Light, vision, and aging. Optom Vis Sci 1990; 67: 214–229.
Dajpratham P, Ploypetch T, Kiattavorncharoen S, Boonsiriseth K . Prevalence and associated factors of musculoskeletal pain among the dental personnel in a dental school. J Med Assoc Thai 2010; 93: 714–721.
Hayes M, Cockrell D, Smith D R . A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg 2009; 7: 159–165.
Rundcrantz B L, Johnsson B, Moritz U . Cervical pain and discomfort among dentists. Epidemiological, clinical and therapeutic aspects. Part 1. A survey of pain and discomfort. Swed Dent J 1990; 14: 71–80.
Perrin P J D, Hotz P . Das Operationsmikroskop in der zahnärtzlichen Praxis: minimalinvasive Füllungen. Schweiz Monatsschr Zahnmed 2002; 112: 723–732.
Leknius C, Geissberger M . The effect of magnification on the performance of fixed prosthodontic procedures. J Calif Dent Assoc 1995; 23: 66–70.
Strassler H E . Magnification systems improve quality and posture. J Esthet Dent 1990; 2: 183–184.
Shanelec D A . Optical principles of loupes. J Calif Dent Assoc 1992; 20: 25–32.
Acknowledgements
The authors would like to thank Claudie Damour-Terrasson, publishing director of the Groupe Information Dentaire, Paris, France, for the authorisation of the translation and publication of the series in the BDJ, as well as Avijit Banerjee for his support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Sitbon, Y., Attathom, T. & St-Georges, A. Minimal intervention dentistry II: part 1. Contribution of the operating microscope to dentistry. Br Dent J 216, 125–130 (2014). https://doi.org/10.1038/sj.bdj.2014.48
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.48
This article is cited by
-
Experts consensus on the procedure of dental operative microscope in endodontics and operative dentistry
International Journal of Oral Science (2023)
-
Efficacy of microsurgery and comparison to macrosurgery for gingival recession treatment: a systematic review with meta-analysis
Clinical Oral Investigations (2021)
-
Minimal invasive microscopic tooth preparation in esthetic restoration: a specialist consensus
International Journal of Oral Science (2019)