Key Points
-
Discusses the integration of oral and general health.
-
Reports the results of a pilot examining the provision of health screening in dental practices.
-
Discusses the extended role of dental care professionals.
-
Outlines the challenges involved in delivering screening programmes in dental practices.
Abstract
Background Dental surgeries are highlighted in the 2012 NICE guidance Preventing type 2 diabetes: risk identification and interventions for individuals at high risk as a suitable setting in which to encourage people to have a type 2 diabetes risk assessment.
Aim To assess the feasibility of implementing a type 2 diabetes risk screening pathway in dental settings using the NICE guidance tool.
Method The study was carried out over two weeks in June 2013. The validated tool in the NICE guidance was used to determine risk. This included a questionnaire and BMI measurement used to determine a risk score. Patients were rated low, increased, moderate or high risk. All patients were given written advice on healthy lifestyle. Patients who were moderate or high risk were referred to their general medical practitioners for further investigation. Participating dental teams were asked to nominate a member who would be responsible for overseeing the screening and training the other team members.
Results A total of 166 patients took part in the pilot (58% male, 75% aged 49 years or younger and 77% were from BME groups). Twenty-six low risk patients (15.7%), 61 increased risk patients (36.7%), 49 moderate-risk patients (29.5%) and 30 high-risk patients (18.1%) were identified during the pilot. Fifteen of the 49 patients (30.6%) identified as moderate-risk and 6 of the 30 high-risk patients (20%) had visited their GP to discuss their type 2 diabetes risk in response to the screening.
Conclusion The pilot suggests that people at risk of developing type 2 diabetes could be identified in primary, community and secondary dental care settings. The main challenges facing dental staff were time constraints, limited manpower and the low number of patients who visited their GP for further advice.
Similar content being viewed by others
Introduction
In July 2012 the National Institute for Health and Clinical Excellence (NICE) published the guidance Preventing type 2 diabetes: risk identification and interventions for individuals at high risk.1 The guidance highlighted a shift towards identifying at-risk individuals in different settings and supplying lifestyle interventions to reduce the numbers of people developing type 2 diabetes. It suggested that screening would ensure those with undiagnosed type 2 diabetes are made aware of their condition and receive appropriate treatment to help prevent complications. Dental surgeries are highlighted in the guidance as a suitable setting for encouraging people to have a type 2 diabetes risk assessment.1 Dentists have an important role in detecting and preventing oral and systemic diseases both because of their diagnostic and screening abilities and the frequency of patient visits.2 Dentists already offer lifestyle advice to their patients as part of a preventive package of care.3 By extending this to cover general healthy eating and activity advice a broader reach of effect is offered to the patient; thereby addressing not only their oral health but also behaviours which may increase risk of type 2 diabetes and cardiovascular disease through the common risk factor approach.
Dentists are not going to diagnose or treat a systemic disease but early detection will result in better medical and dental outcomes and it is the dentist's role to help reduce the incidence and adverse impact of diabetes.4 Studies assessing dentists' attitudes, willingness and barriers towards screening for medical conditions in a dental practice concluded that dentists considered medical screening to be important and they were willing to incorporate it into their practices. However, they felt that practical implementation strategies and education were needed to overcome perceived barriers,5,6 and that the role of dentists in diabetes screening and support requires further investigation.7
A study in Warwickshire looking at the appropriateness of preventive healthcare in a dental practice investigated a subgroup of patients who attend dental practices regularly but medical practices infrequently. They concluded that the dental team could have an important role to play in general health risk assessment.8
Acceptance by patients of chairside medical screening in a dental practice is crucial for successful implementation.9 A study on patient experience relating to oral health and diabetes in dental practice recommended that written information regarding diabetes and its possible effects on oral health needs to be more readily available.10
The aim of the pilot was to assess the feasibility of implementing a type 2 diabetes risk screening pathway in dental settings using the NICE guidance tool.
Methods
A pilot study to identify people at risk of developing type 2 diabetes was carried out over two weeks in June 2013. Patients attending for treatment in the dental settings and meeting the eligibility criteria were invited to take part in the pilot. The validated tool in the NICE guidance was used to determine risk. This included a questionnaire and BMI measurement which were used to determine a risk score. Patients were rated low, increased, moderate or high risk. All patients were given written advice on healthy lifestyle. Patients who were moderate or high risk were referred to their general medical practitioners for further investigation. They were contacted after four weeks to ascertain whether they had visited their GP for follow-up and asked about their experience of the screening programme. Feedback from dental teams was obtained through semi-structured interviews. None of the settings were given any funding to carry out this pilot.
Setting
The screening pathway was tested in three dental settings:
-
Two general dental practices
-
A specialist clinic at a dental hospital
-
A dental school outreach clinic.
The two GDP practices were self-selected practices in Newham and Tower Hamlets in East London. The practices had between five and eight dentists working with dentists seeing approximately 25 patients a day. The specialist hospital clinic had five oral medicine specialists receiving patients referred from across London. Patients seen at the dental school clinic in East London were treated by students under supervision in a ten bay clinic.
Training
Participating dental teams were asked to nominate a member who would be responsible for overseeing the screening and training the other team members. This included dental nurses, hygienists, receptionists and dentists. A two hour training session was arranged for nominated staff. The training session which was carried out by a member of the diabetes team covered the risks and effects of type 2 diabetes, how to use the risk assessment tool, how to provide 'brief advice' as set out in the NICE guidelines and how to refer potentially moderate- and high-risk patients to their GP.
Eligibility and consent
All patients aged 25 years or over who had not received a diabetes screening in the previous five years were invited to take part in the pilot. Pregnant patients were excluded. Those who agreed to participate were given an information sheet and asked to give consent.
Questionnaire
The following topics were covered in the questionnaire which was developed by the University of Leicester: age, gender, ethnicity, family history of diabetes and hypertension.
Calculating BMI
The three settings were provided with calibrated weighing scales, height measuring tools, a tape measure and BMI calculators.
Resources provided to practices
Practices were provided with patient information sheets, healthy eating and activity advice sheets, diabetes risk score sheets, letters for GP referrals and a data collection sheet to measure screening activity.
Four week follow-up
A follow-up telephone call was made to all moderate- and high-risk patients four weeks after their diabetes screening to collect information on patient experience of the screening and to ascertain whether they had visited their GP.
Pilot evaluation
The following measurements of activity were recorded:
-
Number of patients offered screening
-
Number of patients who accepted screening
-
Diabetes risk scores of patients (low/increased/moderate/high)
-
Number of lifestyle information sheets delivered
-
Number of patients referred to GP
-
Number of patients who received follow-up phone call four weeks post screening
-
Number of patients who attended their GP or had appointments made.
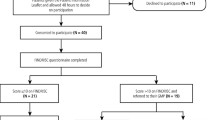
Feedback from the participating practices was obtained using semi-structured telephone interviews. Figure 1 shows the flowchart of the risk assessment pathway
Results
A total of 191 patients were invited to take part in the pilot. Of these 166 (87%) accepted. The main reasons for patients declining were time, previous diagnosis or feeling that they were not at risk of type 2 diabetes. Fifty-eight percent were male, 75% were aged 49 years or younger and 77% were from BME groups (Table 1).
Twenty-six low risk patients (15.7%), 61 increased risk patients (36.7%), 49 moderate-risk patients (29.5%) and 30 high-risk patients (18.1%) were identified during the pilot (Table 1). A similar percentage of low, increased, moderate- and high-risk patients were identified in each setting. High risk patients were more likely to be older, male and from a BME group.
Contact was made with 79.6% of moderate-risk and 63.3% of high-risk patients screened in our four-week post screening telephone follow-up calls (Table 1). Seventy-five percent of moderate-risk patients and 78.4% of high-risk patients were very satisfied or satisfied with the diabetes risk screening they had at the dental practice. Fifteen of the 49 patients (30.6%) identified as moderate-risk and 6 of the 30 high-risk patients (20%) had visited their GP to discuss their type 2 diabetes risk in response to the screening. Reasons for patients not making a GP appointment included misplacing the referral letter, busyness, being abroad, delaying the appointment until after Ramadan and not feeling that the condition was 'serious enough' to visit their GP.
Feedback from staff involved in the pilot
Practice staff commented on the high quality of the pre-pilot diabetes training session provided by the designated diabetes educator. All staff involved were very satisfied or satisfied with the content of the training. They felt that the training session had improved their knowledge and understanding of type 2 diabetes and felt confident about using the diabetes risk score tool and equipment after the training session.
Practice staff had positive experiences communicating with patients throughout the screening programme. They were happy explaining the purpose of the screening and were able to address patient queries about why the dental practice was offering diabetes screening. They commented on how easy it was to follow the screening flowchart and felt that the standard diabetes risk score form helped them to tailor their brief advice based on the risk factors highlighted on the forms. They felt that the screening programme had highlighted the links between general and oral health, and had enabled them to communicate this relationship to patients. However, they noted that the screening had added 20 minutes to appointments. Some patients were unable to stay the extra time and the pilot caused disruption of the normal running of the practice.
Dental practice owners felt that the screening had not only had a positive impact on the whole practice but also provided tangible benefits by equipping their DCPs with new skills.
Dentists and staff commented that in order to carry out this screening programme long term in a dental practice a dedicated member of staff would be needed to coordinate and carry out the screening. This would have obvious cost implications.
Discussion
Successful implementation of a type 2 diabetes risk screening programme in a dental setting is dependent on the willingness of patients to undergo the screening, the attitudes and willingness of the dental teams to provide the screening programme, overcoming the barriers to practical implementation and the effectiveness of the screening programme.
Willingness by patients to undergo a medical screening in a dental setting is crucial to the implementation of a screening programme.6 In this pilot 87% of those invited agreed to be screened. This is in keeping with the findings of other studies8,9 showing that most patients are willing to have dental teams screen for diabetes. Written information regarding diabetes should be readily available.9 In this pilot all patients were given brief advice on healthy eating and physical activity which included written information.
Dental teams were willing to conduct the screening and felt that the screening programme had a positive impact on the whole practice and equipped the dental care professional with new skills. This is supported by previous studies.6 One study however found that dentists were less willing to carry out height and weight measurements.6
The pilot identified that of those screened 47.6% (29.5% moderate and 18.1% high) were at risk of developing type 2 diabetes. Despite positive feedback from patients about the screening programme only 30% of moderate risk and 20% of high risk visited their GP in follow up to the risk screening. This is consistent with other studies on diabetes screening uptake where patients suggested that lack of perceived severity and time were key barriers preventing them from visiting their GP.11 More work is needed to develop strategies to improve the follow-up at GP practices for moderate- and high-risk patients.
The main barriers identified in this pilot were similar to those found in previous studies.6 These included time and costs. The screening in this pilot added 20 minutes to the appointment and some patients were unable to stay the extra time particularly after a lengthy dental appointment. The limited number of staff carrying out the screening meant that some patients had to wait to be screened particularly during busy surgery times. Another barrier we identified in this study was that some female patients were uncomfortable with having male dental staff carry out the waist circumference measurement. The area where the pilot was conducted has a large proportion of Muslims and this may explain their reluctance due to religious reasons. It was interesting to note that the issues raised by staff were the same in all three settings.
While the dentists were happy to divert staff from other duties and accept some disruption of practice for this two week pilot they felt that any long-term programme would need dedicated staff and would have to be properly costed and funded. Additional education and practical implementation strategies are necessary to address these barriers.5
As the pilot was only carried out over a two week period the findings should be interpreted with caution. The limitations of this pilot are the short duration, low numbers of participants and low number of general dental practices and limited geographical range. The pilot did not quantify the financial impact on practices in delivering the screening pathway. More work is needed on extending the length of the pilot, including more practices (particularly in areas with high diabetes prevalence) and ensuring that moderate- and high-risk patients' follow-up on their screening results. Improving communication between GP and dental practices is needed to ensure that moderate- and high-risk patients are followed up and have appropriate care. This is in keeping with the findings of a recent publication about collaboration between medicine and dentistry in relation to diabetes management.12
Conclusion
This pilot study suggests that people at risk of developing type 2 diabetes could be identified in primary, community and secondary dental care settings. Dental care professionals were able to effectively deliver recommended, brief, lifestyle advice to patients related to physical activity and healthy eating. Patient and dental staff feedback about the risk screening pathway was highly positive. The main challenges were time constraints, limited manpower and the low number of moderate- and high-risk patients who visited their GP for further advice and a diagnostic blood test as advised after the screening. This pilot study highlights the potential for dental practices to offer type 2 diabetes risk screening and other general health screening programmes in dental practices. This would ideally need to be separately commissioned as an enhanced service.
References
National Institute for Clinical Care and Excellence. Preventing type 2 diabetes: risk identification and interventions for individuals at high risk 2012. NICE public health guidance 38. Manchester: NICE, 2012. Online information available at: www.nice.org.uk/nicemedia/live/13791/59951/59951.pdf (accessed January 2014).
Tavares M, Dewundara A, Goodson J M . Obesity prevention and intervention in dental practice. Dent Clin North Am 2012; 56: 831–846.
Department of Health. Delivering better oral health: an evidence based toolkit for intervention 2009. 2nd ed. London: DH, 2009. Online information available at: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets /documents/digitalasset/dh_102982.pdf (accessed January 2014).
Ali D, Kunzel C . Diabetes mellitus: update and relevance for dentistry. Dent Today 2011; 30: 48–50.
Greenberg B L, Glick M, Frantsve-Hawley J, Kantor M L . Dentists' attitudes towards chairside screening for medical conditions. J Am Dent Assoc 2010; 141: 52–62.
Laurence B . Dentists consider medical screening important and are willing to incorporate screening procedures into dental practice. J Evid Based Dent Pract 2012; 12 (Suppl): 32–33.
Bowyer V, Sutcliffe P, Ireland R et al. Oral health awareness in adult patients with diabetes: a questionnaire study. Br Dent J 2011; 211: E12. DOI:10.1038/sj.bdj.2011.769.
Ireland R S, Bower V, Ireland A, Sutcliffe P . The medical and dental attendance pattern of patients attending general dental practices in Warwickshire and their general health risk assessment. Br Dent J 2012; 212: E12. DOI:10.1038/sj.bdj.2012.313.
Greenberg B L, Kantor M L, Jiang S S, Glick M . Patients' attitudes towards screening for medical conditions in a dental setting. J Public Health Dent 2012; 72: 28–35.
Lindenmeyer A, Bowyer V, Roscoe J, Dale J, Sutcliffe P . Oral health awareness and care preferences in patients with diabetes: a qualitative study. Fam Practice 2013; 30: 113–118.
Eborall H, Stone M, Aujla N, Taub N, Davies M, Khunti K . Influences on the uptake of diabetes screening: a qualitative study in primary care. Br J Gen Pract 2012; 62: e204–211. DOI:10.3399/bjgp12X630106.
Bissett S M, Stone K M, Rapley T, Preshaw P M . An exploratory qualitative interview study about collaboration between medicine and dentistry in relation to diabetes management. BMJ Open 2013; 3: e002192. DOI:10.1136/bmjopen-2012-002192.
Acknowledgements
We would like to acknowledge the support of the Diabetes Educator in providing the training and the dental teams in all three settings for their considerable cooperation and support in the conduct of this pilot.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Wright, D., Muirhead, V., Weston-Price, S. et al. Type 2 diabetes risk screening in dental practice settings: a pilot study. Br Dent J 216, E15 (2014). https://doi.org/10.1038/sj.bdj.2014.250
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.250
This article is cited by
-
Opportunistic health screening for cardiovascular and diabetes risk factors in primary care dental practices: experiences from a service evaluation and a call to action
British Dental Journal (2023)
-
Oral health professionals screening for undiagnosed type-2 diabetes and prediabetes: the iDENTify study
BMC Endocrine Disorders (2022)
-
The prevalence of potentially undiagnosed type II diabetes in patients with chronic periodontitis attending a general dental practice in London - a feasibility study
British Dental Journal (2021)
-
A modern approach to periodontal management
BDJ Student (2021)
-
Periodontitis and diabetes
BDJ Team (2020)