Key Points
-
Describes current practice for the prevention and management of caries in children.
-
Highlights a gap between current practice and guidance recommended practice.
-
Adds to the body of evidence that, in addition to the publication of guidance, further intervention is likely to be required to achieve a desired change in practice by health professionals.
Abstract
Aims In April 2010, the Scottish Dental Clinical Effectiveness Programme (SDCEP) published guidance on the Prevention and management of dental caries in children. The aims of this study were to determine if further intervention is required to translate the SDCEP guidance recommendations into practice and to identify salient beliefs associated with recommended practice.
Methods Two postal surveys circulated to two independent random samples of dentists working in general dental practices in Scotland, before and after the publication of the guidance. The questionnaire items assessed current practice and beliefs relating to the prevention and management of dental caries in children.
Results Response rates of 40% (n = 87) and 45% (n = 131) were achieved. The results highlight a gap between current practice and recommended practice. The majority of dentists do not 'always' perform recommended behaviours and many are following treatment strategies specifically not recommended in the guidance. More positive attitude, greater capability and motivation were significantly associated with performing more guidance recommended risk assessment and prevention behaviours.
Conclusions These findings highlight the need for further intervention to translate the SDCEP guidance recommendations into practice and give initial insight into the salient beliefs that may serve as targets for future interventions.
Similar content being viewed by others
Background
In Scotland, tens of thousands of people experience dental caries every year, with both adults and children affected.1,2 Caries is preventable but remains a costly global public health problem that can impact upon quality of life, attendance and productivity in school or work as well as general health.1,3,4,5,6 In Scotland, oral health problems related to caries are the most common reason for elective hospital procedures in children under the age of 18, accounting for approximately 7,000 episodes annually.7
In recent years, significant progress has been made towards improving children's oral health in Scotland. However, figures from the 2012 National Dental Inspection Programme show that one third of Primary 1 (5 year olds) children still have signs of dental caries. In the areas of highest deprivation 49% of children have obvious caries experience compared to only 19% of children in the lowest deprivation areas.8
Traditionally, dental care for children in Scotland has mainly focused on treatment for caries, with children's first dental experience often being for the management of pain or infection associated with this.2 However, the importance of contact with dental services at an early age and an increased emphasis on prevention is now well recognised. This shift towards a preventive paradigm was evident in the 2005 Scottish Government's Action plan for improving oral health and modernising NHS dental services9 which launched Childsmile, a national oral health programme for children10. In 2007, Childsmile was further extended following recommendations outlined in Better Health, Better Care11 and since 2011 all elements of the programme have been delivered in all Health Board areas throughout Scotland.12
Additionally, in April 2010, the Scottish Dental Clinical Effectiveness Programme (SDCEP) published guidance on the Prevention and Management of Dental Caries in Children.2 This guidance was designed to assist and support dental professionals in primary care to improve and maintain the oral health of their child patients. A printed copy was posted to every practicing dentist in Scotland in May 2010. The guidance works alongside the Childsmile programme and presents clear and consistent recommendations for the delivery of preventive care and, when necessary, the management of caries.
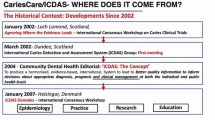
However, it is well documented that the translation of recommendations into practice requires more than the publication of evidence-based clinical guidance and that publication and distribution of guidance alone may not result in improved healthcare or health.13,14,15,16,17 To bridge this gap between dissemination of SDCEP guidance recommendations and their implementation into practice, the Translation research in a dental setting (TRiaDS) programme was established in 2008.18 TRiaDS is a multidisciplinary research collaboration, embedded within the SDCEP guidance development process. Its remit is not only to evaluate the impact of guidance on practice and determine if additional interventions are required for guidance implementation, but also to further an understanding of what underlies changes in clinical practice using theoretical models of behaviour change.18,19
The overall aim of this study was to determine if further intervention is required to translate the SDCEP guidance recommendations for the prevention and management of dental caries in children into practice. A further aim was to identify salient beliefs associated with recommended practice, to serve as possible targets for a theory based intervention, if required.
Methods
Design and participants
This was a cross-sectional study conducted with dentists working in primary dental care in Scotland. Data collection was by means of two postal surveys; the first conducted pre-guidance publication in April 2010, followed by the second in January 2011, nine months after the publication of the SDCEP guidance. All questionnaires were sent by first class mail with a personalised covering letter and return freepost envelope.
In April 2010 a random sample of 232 dentists (representing 25% of primary care dental practices) received a copy of the questionnaire. The sample was identified from the Management Information and Dental Accounting System database. For the January 2011 survey, a total of 300 questionnaires were distributed. Randomisation for both surveys was a two-step simple randomisation procedure using computer generated random numbering. Step one identified the practices and step two randomly selected one dentist from each practice to receive the survey. A reminder letter with a second copy of the questionnaire was sent to non-responders after two weeks, followed by a postcard reminder at four weeks. Telephone call reminders were also conducted during this stage.
Questionnaire development
In consultation with the Guidance Development Group for the SDCEP guidance and the SDCEP Programme Development Team, key recommendations in relation to the prevention and management of caries and their associated behavioural outcomes were identified. These recommendations informed the development of the questionnaire items measuring current practice.
Beliefs that may be salient to following recommended practice were derived from psychological models encompassed by the Theoretical Domains Framework (TDF). The TDF consolidates and enables application of 33 psychological models of behaviour change to help understand the context and nature of the behaviour(s) to be changed, and to guide identification of the behavioural target(s) and potential interventions for change.20,21,22,23 Questionnaire items assessing attitudinal beliefs (from the TDF domain beliefs about consequences), perceptions of control (from the TDF domain beliefs about capabilities), and motivation (from the TDF domain goals/motivation/intention) were constructed in accordance with TDF operationalisation protocols.19
Measures
Current practice
Dentists were asked to consider their current practice in relation to the prevention and management of caries for their child patients (Table 1), and to indicate how often the behavioural outcomes associated with the key recommendations are conducted, that is, rarely/never, sometimes, usually, always. Responses were scored from one (rarely/never) to four (always).
Totals were created for guidance recommended risk assessment and prevention behaviours. The total risk assessment score was the sum of four behaviour items; currently for my child patients, I: assess caries risk; record caries risk; use caries risk to inform the choice of recall interval; use caries risk to inform the preventive care I provide. For each respondent, possible scores ranged from four to 16, where higher scores reflect greater risk assessment behaviour. The total prevention score was the sum of six behaviour items; in my current practice, to prevent caries in my child patients, I (or a member of my dental team): give toothbrushing advice; demonstrate toothbrushing; give dietary advice; apply fluoride varnish; place preventive fissure sealants; check existing fissure sealants at each recall visit. Possible scores ranged from six to 24, where again higher scores reflect greater prevention behaviour.
Diagnosis and management of caries items reflected the treatment strategies available to dentists detailed in the guidance. In many cases the particular strategy adopted is likely to be dependent upon the given clinical situation. The use of bitewing radiographs to aid diagnosis, however, is recommended practice, while placing glass-ionomer restorations in Class II cavities and doing nothing are strategies specifically not recommended by the SDCEP guidance.
Beliefs
All belief items were measured using a five point Likert scale; from strongly disagree to strongly agree. Beliefs from three domains of the TDF were measured. To assess beliefs about consequences (attitude) dentists were asked if they thought the behaviours were important and effective. Beliefs about capabilities (perceptions of control) and motivation were assessed by asking dentists how difficult the behaviours were to perform and if they were motivated to perform them. Totals (mean scores) were created for beliefs relating to risk assessment and prevention. Possible scores ranged from one to five, where higher scores reflect more positive beliefs.
Demographics
Demographic information relating to the dentist (age, gender, role, patient list size) and their dental practice (whether a Childsmile practice, composition of dental team staff, number of child patients, and if the practice has internet access) was collected. In the January 2011 survey additional questions were asked to measure the level of awareness of the SDCEP guidance among dentists and to determine how useful dentists found it (measured on a five point scale, 1 = not at all useful; 5 = extremely useful).
Data analysis
Summary descriptives, percentages for each behaviour outcome and demographic characteristics were produced. The measures generated for risk assessment and prevention were tested for internal consistency using Cronbach's alpha. Pearson correlations and linear stepwise regression models were used to examine the relationship between beliefs and current behaviours. Independent t-tests were used to assess differences in behaviour and beliefs over time. Statistical significance was defined as p-value <0.05 and based on two-sided tests.
Ethical considerations
The East of Scotland Research Ethics Service considered this study in April 2010. It was advised the study was service development and full ethical review was not required.
Results
Response rates
Of the 232 questionnaires posted to GDPs in April 2010, 87 were returned completed; 16 were undeliverable (left practice, maternity leave etc), giving an overall response rate of 40% (87/216). A higher response rate of 45% (131/292) was achieved for the post publication survey conducted in January 2011. From the 300 questionnaires posted, 131 were returned completed, eight were undeliverable.
Demographics
In the April 2010 survey, just over half (51%) of respondents were male, with an average age of 41 years (range from 24–67). Three percent of the sample described themselves as salaried, while over half (57%) considered themselves principal dentists and 41% associate dentists. Thirteen percent were vocational trainers. On average, respondents worked eight clinical sessions per week and had an approximate list size of 2000. The percentage of child patients (16 and under) ranged from 2–95%, with an average of 19%. Thirteen percent of practices were single handed and just over a third of respondents (37%) considered their practice to be a Childsmile practice. All practices employed a dental nurse and 60% of practices employed at least one other dental care professional, including hygienist, hygienist therapist and extended duty dental nurse.
Demographic variables were collected to assess the representativeness of the two samples with each other and, where possible, with the general dental population as a whole. There were no statistically significant differences between any demographic variables in the April 2010 survey and the later one conducted in January 2011. Both samples also had a similar demographic profile to the population of general dentists and practices in relation to gender, health board, and average practice size. Ninety one percent (119/131) of dentists in the 2011 survey were aware of the SDCEP guidance and on average found it to be very useful (mean score of four on a five point usefulness scale).
Current practice (Table 1)
Caries risk assessment
The percentage of dentists 'always' conducting risk assessment behaviours ranged from 26–58% pre-guidance publication and from 23–53% post guidance publication. Risk was assessed more often than it was recorded and use caries risk to inform the choice of recall interval was the least performed behaviour. No statistically significant changes in behaviour were identified between respondents across the two surveys.
Caries prevention
The percentage of dentists 'always' performing prevention behaviours ranged from 10–63% pre-guidance publication and from 10–60% post guidance publication. The behaviours being performed the most (check existing fissure sealants at each recall interval and give dietary advice) and least (apply fluoride varnish and demonstrate toothbrushing) were the same at both time points. The percentage of dentists who 'usually' or 'always' place preventive fissure sealants was the same in both surveys (68%). Giving dietary advice was the only behaviour where a significant change across the surveys was observed. In the post guidance publication survey, the percentage of dentists 'always' giving dietary advice had fallen to 44%, compared to 58% in the pre-guidance publication survey.
Diagnosis and management of caries
Approximately half of dentists (45% in April 2010; 48% in January 2011) 'rarely' or 'never' take bitewing radiographs. Two thirds of dentists (67% in April 2010; 64% in January 2011) 'rarely' or 'never' perform the Hall Technique and most (∼90%) 'rarely' or 'never' follow the do not remove caries and place fissure sealants management strategy. In April 2010, 26% of dentists 'usually' placed glass-ionomer restorations in Class II cavities. In the January 2011 survey, this had increased to 36% of dentists. Approximately half of dentists 'sometimes' adopt a do nothing approach to the management of caries in the primary dentition. No significant changes were identified for any behaviour across the two surveys.
Beliefs
With just two exceptions, independent t-tests revealed no significant differences between the two surveys for beliefs related to performing caries risk assessment, prevention and management in children (Tables 2 and 3). Between April 2010 and January 2011, a significantly more positive attitude about the effectiveness of not removing caries and placing fissure sealants was observed and there was a significant increase in motivation to perform extractions when managing caries in primary teeth (Table 3).
Dentists believed caries risk assessment and prevention behaviours were important, not difficult to do and were motivated to perform them. From a possible score of five, means for risk assessment were 4.0, 3.9 and 3.8 respectively, at both time points. The means for beliefs associated with prevention behaviours ranged from 3.7–3.9 in April 2010 and 3.9–4.0 in January 2011 (Table 2).
Beliefs associated with the diagnosis and management of caries had consistently lower means than beliefs associated with caries risk assessment and prevention behaviours (Table 3). In general, the behaviours that dentists believed were effective, were the behaviours they found difficult and were not motivated to perform (take bitewing radiographs, carry out complete caries removal, perform the Hall Technique, carry out pulp therapy and extract). Dentists believed that do not remove caries and provide prevention and do nothing were not at all difficult, not effective and were not motivated to perform them (Table 3).
Attitude, capability and motivation were all significantly positively correlated with risk assessment and prevention behaviour (Table 2). To further examine the influence of these beliefs on behaviour, each variable was entered into exploratory stepwise multiple regression models with caries risk assessment and prevention behaviour as the independent variables (Table 4). Motivation explained 47% of the variance in caries risk assessment and 22% of the variance in prevention behaviour.
Individual belief items from these variables were then entered into a further exploratory stepwise regression. Three of the four risk assessment items (motivation to assess risk, record risk and use caries risk to inform the choice of recall interval) explained 49% of the variance in performing risk assessment. Three of the six prevention items (motivation to demonstrate toothbrushing, apply fluoride varnish and place preventive fissure sealants) explained 25% of the variance in performing prevention behaviour (Table 4).
Similarly, all variables that were significantly correlated with individual management behaviours (Table 3) were entered into a series of exploratory stepwise regression analyses to identify the main drivers of behaviour (Table 5). Motivation explained significant variance in take bitewing radiographs (31%), do not remove caries and place fissure sealants (8%), place glass-ionomer restorations in Class II cavities (42%), do nothing (11%) and carry out pulp therapy (41%). Motivation combined with capability or attitude explained the variance in carry out complete caries removal (39%), perform the Hall Technique (60%) and extract (19%). Attitude alone explained significant variance (14%) in carry out partial caries removal.
Discussion
The overall aim of this study was to determine if further intervention is required to translate the SDCEP Prevention and management of dental caries in children guidance recommendations into practice. The results show that at the time of the pre-guidance publication survey in April 2010, there was a gap between current and recommended practice. Nine months after the publication of the guidance, there was little difference in reported practice and the gap between current and recommended practice remained.
Caries risk assessment is an important part of the overall assessment of a child patient. It enables the development of an appropriate individualised personal care plan based on a child's susceptibility to disease and helps to identify children who are at an increased risk of developing caries2. However, only half of dentists 'always' assess caries risk and only half of these 'always' record this risk. The guidance recommends that dentists, 'use the caries risk assessment to inform the provision of preventive interventions and frequency of recall'.2 The majority of dentists are not 'always' doing this.
Preventive intervention is recommended practice for all children. Four simple and effective evidence-based interventions are available to the dental team: toothbrushing with fluoride toothpaste, dietary advice, topical fluoride and fissure sealants. Toothbrushing and dietary advice is usually provided, however many participating dentists reported not placing preventive fissure sealants and most did not apply fluoride varnish.
The guidance provides advice on diagnosis and information on a number of management strategies available to the dentist, along with examples and illustrations of the types of lesions for which they can be considered.2 Although in many cases the particular management strategy adopted is likely to be dependent upon the clinical situation, the results again indicate a disparity between current practice and guidance recommendations.
Despite the guidance recommending that, 'after clinical examination, for a child who is aged four or above, if no previous radiographs have been taken or are available, take bitewing radiographs to enable accurate caries diagnosis',2 almost half of dentists surveyed 'rarely' or 'never' take them. Placing glass-ionomer restorations in Class II cavities is something that the guidance recommends should not be done. However, in the April 2010 survey, a quarter of dentists 'usually' performed this. At the time of the second survey, the number of dentists 'usually' doing this had increased. Approximately half of dentists 'sometimes' choose to do nothing, again another strategy specifically not recommended in the guidance.2
These results, combined with evidence of little difference in practice following the publication of the guidance, support the need for further intervention. It also adds to the body of evidence that publication of guidance alone is unlikely to achieve a desired change in practice by health professionals.
A further aim of this study was to identify if beliefs derived from a theoretical framework, (the TDF) were associated with the assessment, prevention and management of dental caries in children. This could then inform the development of a tailored, theory based intervention, if required. The regression analyses revealed that the most salient domain was motivation that is, the more motivated dentists were to perform behaviours, the more likely they were to do them.
There are evidence-based psychological techniques that can be used to influence motivation and provide a framework for intervention design.24 For example, encouraging dentists to set a specific goal about taking bitewings when doing all risk assessments would be one method to encourage motivation to perform diagnostics in an evidence-based way. Another strategy for encouraging motivation is to provide information about how others (colleagues, patients, professional bodies) feel about what you are doing, or what should be done. For example, training courses could specifically focus on the evidential support for partial caries removal and the lack of support for placing glass-ionomer restorations. A letter from the Chief Dental Officer might be circulated to all dentists to provide general encouragement for the provision of detailed tooth brushing advice to all patients.
This study presents findings from two snapshots in time, therefore limiting the possibility to accurately measure change or attribute any change to the publication of guidance alone. However, this snapshot approach was a pragmatic way of identifying current practice and beliefs from a greater number of dentists in a relatively small study population. Having two random independent samples increases the representation of participants and provides validation of consistently emerging results. The lack of significant differences between samples in all demographic variables and reported behaviour and beliefs provides evidence to support this.
Another potential limitation is response bias due to the self-report nature of the study. However, result bias is usually toward the desired behaviour that is, compliance with guidance recommendations. Even if self-report artificially inflated compliance levels, this does not impact on the validity of these results, which strongly suggest further intervention is still required to encourage compliance. Nevertheless, this is an important methodological issue. Like most studies of this nature, self-report behaviour was used to proxy objective data, which can be prohibitively resource intensive to obtain on a national scale. In future investigations, we will be specifically exploring the relationship between self-reported behaviour and routinely collected data from dental accounting systems, where available.
Despite the limitations, this study provides intelligence on how caries is being managed in children in primary care in Scotland. While the results show that dentists believe caries risk assessment and prevention behaviours are important, not difficult to do and are motivated to perform them, the frequency at which they are being carried out in practice falls short of guidance recommendations. This highlights the need for further intervention in this area and for additional work to better understand the factors influencing behaviour. The results also demonstrate the possibility of applying a theoretical framework to inform intervention design.
The findings from this study have been made available for consideration in the review to update the SDCEP Prevention and management of dental caries in children guidance. Furthermore, the results will inform current TRiaDS investigations into policy and patient factors which may also be influencing caries prevention in primary dental care across Scotland.
References
Petersen P E . The World Oral Health Report 2003: continuous improvement of oral health in the 21st century - the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2003; 31 Suppl 1: 3–23.
Scottish Dental Clinical Effectiveness Programme. Prevention and management of dental caries in children: dental clinical guidline. Dundee: Scottish Dental Clinical Effectiveness Programme, 2010.
Bagramian R A, Garcia-Godoy F, Volpe A R . The global increase in dental caries. A pending public health crisis. Am J Dent 2009; 22: 3–8.
Nuttall N M, Steele J G, Evans D, Chadwick B, Morris A J, Hill K . The reported impact of oral condition on children in the United Kingdom. Br Dent J 2006; 200: 551–555.
Sheiham A . Dental caries affects body weight, growth and quality of life in pre-school children. Br Dent J 2006; 201: 625–626.
Locker D, Jokovic A, Stephens M, Kenny D, Tompson B, Guyatt G . Family impact of child oral and oro-facial conditions. Community Dent Oral Epidemiol 2002; 30: 438–448.
NHS National Services Scotland. Operations and procedures. Information Services Division. Online information available at http://www.isdscotland.org/Health-Topics/Hospital-Care/Operations-and-Procedures/ (accessed December 2014).
Macpherson L M D, Ball G, Conway D I et al. Report of the 2012 detailed national dental inspection programme for primary 1 children and the basic inspection of primary 1 and primary 7 children. Information Services Division, NHS National Services Scotland. 2012. Online information available at http://www.isdscotland.org/Health-Topics/Dental-Care/Publications (accessed December 2014).
Scottish Executive. An action plan for improving oral health and modernising NHS dental services in Scotland. 2005. Online information available at http://www.scotland.gov.uk/Publications/2005/03/20871/54813 (accessed December 2014).
Macpherson L M D, Ball G E, Brewster L et al. Childsmile: the national child oral health improvement programme in Scotland. Part 1: establishment and development. Br Dent J 2010; 209: 73–78.
Scottish Government. Better health, better care: action plan. 2007 Online information available at http://www.scotland.gov.uk/Publications/2007/12/11103453/0 (accessed December 2014).
NHS Health Scotland. About Childsmile. Online information available at http://www.child-smile.org.uk/professionals/about-childsmile.aspx (accessed December 2014).
Seddon M E, Marshall M N, Campbell S M, Roland M O . Systematic review of studies of quality of clinical care in general practice in the UK, Australia and New Zealand. Qual Health Care 2001; 10: 152–158.
Schuster M A, McGlynn E A, Brook R H . How good is the quality of health care in the United States? Milbank Q 1998; 76: 517–563: 509.
Grol R . Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care 2001; 39 Suppl 2: 46–54.
Clarkson J E, Turner S, Grimshaw J M et al. Changing clinicians' behaviour: a randomised controlled trial of fees and education. J Dent Res 2008; 87: 640–644.
Grimshaw J M, Thomas R E, MacLennan G et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess 2004; 8: 1–72.
Clarkson J E, Ramsay C R, Eccles M P et al. The translation research in a dental setting (TRiaDS) programme protocol. Implement Sci 2010; 5: 57.
Michie S, Johnston M, Abraham C et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005; 14: 26–33.
Cane J, O'Connor D, Michie S . Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012; 7: 37.
Francis J J, Stockton C, Eccles M P et al. Evidence-based selection of theories for designing behaviour change interventions: using methods based on theoretical construct domains to understand clinicians' blood transfusion behaviour. Br J Health Psychol 2009; 14 Pt 4: 625–646.
French S D, Green SE, O'Connor D A et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci 2012; 7: 38.
Francis J J, O'Connor D, Curran J . Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the theoretical domains framework. Implement Sci 2012; 7: 35.
Abraham C, Michie S . A taxonomy of behaviour change techniques used in interventions. Health Psychology 2008; 27: 379–387.
Acknowledgements
This study was conducted as part of the TRiaDS programme of research and was funded by NHS Education for Scotland. We would like to thank the TRiaDS Research Methodology Group and all participating dentists.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Elouafkaoui, P., Bonetti, D., Clarkson, J. et al. Is further intervention required to translate caries prevention and management recommendations into practice?. Br Dent J 218, E1 (2015). https://doi.org/10.1038/sj.bdj.2014.1141
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.1141
This article is cited by
-
A scoping review of dental practitioners’ perspectives on perceived barriers and facilitators to preventive oral health care in general dental practice
BMC Oral Health (2024)
-
Factors perceived by health professionals to be barriers or facilitators to caries prevention in children: a systematic review
BMC Oral Health (2023)
-
NHS general dental practitioner claims in the South West for provision of topical fluoride, fissure sealants, radiographs, fillings and extractions for children born in 2009: an analysis of a five-year period
British Dental Journal (2022)
-
The effect of introducing a financial incentive to promote application of fluoride varnish in dental practice in Scotland: a natural experiment
Implementation Science (2018)
-
Guidelines relevant to paediatric dentistry – do foundation dentists and general dental practitioners follow them? Part 1: diagnosis and prevention
British Dental Journal (2018)