Key Points
-
Suggests gingival black triangles are preventable in many situations and manageable in others.
-
Highlights that gingival black triangles can be caused and also treated using restorative and orthodontic procedures.
-
Provides a range of treatment options, most of which are applicable to general practice.
Abstract
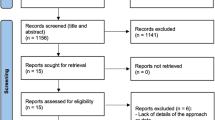
Gingival black triangles (GBTs) are generally considered to be aesthetically unacceptable, have a multifactorial aetiology and a range of treatment options. This review covers the surgical and non-surgical management of GBTs. Surgical methods address recontouring, preserving or reconstructing the soft tissue including the interdental papilla as well as the alveolar bone. Non-surgical approaches include restorative techniques (including the use of prostheses and gingival-coloured materials), orthodontic movement, tissue engineering and tissue volumisers. This review covers the aetiology and management of GBTs, highlighting the importance of considering the options currently available when treating a lost dental papilla. A lack of longitudinal studies investigating the long-term outcomes of the options in management of GBTs presence is identified.
Similar content being viewed by others
Introduction
The interdental papilla is an important component in an aesthetic smile1,2,3,4 and its loss may result in a gingival black triangle (GBT). These spaces can also cause phonation problems as well create space for food and plaque accumulation.5 Kokich et al. demonstrated that patients and dentists found black triangles greater than 3 mm less attractive.6 A recent study assessing 80 randomly selected patients' perceptions of GBTs in terms of number of visible triangles and their severity and showed that patients found presence of GBTs the third most disliked aesthetic problems after caries and crown margins.7 A unilateral papillary height reduction of 2 mm was considered to be unattractive.
Kurth and Kokich sampled 337 patients from 4,500 records of two private orthodontic practices to assess the prevalence of GBTs between maxillary central incisors after orthodontic treatment. The study showed the prevalence of incomplete papillae between maxillary incisors is about one third of the population.8 Another study estimated that 15% of the general adolescent patients who underwent orthodontic treatment for maxillary incisors crowding could expect presence of GBTs after treatment.2
Management techniques to rectify GBTs have been inconsistent among clinicians. Limited blood supply to the papilla is always an issue in the tissue's reaction to any trauma or intervention. Low blood supply to interdental papillae makes them very fragile and sensitive to recession, which makes restoring the receded papillae unpredictable.9,10,11
Aetiology of the presence of GBTs
Studies are well documented that the aetiology of GBTs is multifactorial.1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16 Papillae dimension can be changed due to any of the following reasons:
-
1
Inter-proximal space between teeth
-
2
The distance between inter-proximal contact position to bone crest
-
3
Gingiva biotype
-
4
Patient's age
-
5
Periodontal disease and loss of attachment, resulting in recession
-
6
Diverging roots, which can follow orthodontic treatment
-
7
Tooth morphology and abnormal crown and restoration shape.
Inter-proximal space between teeth
The size of inter-dental width is relevant to the presence of GBTs. While a greater width may enable improved blood supply to papillae tip, which may be helpful to maintain a full papillae, a very wide interdental width increases the risk of the presence of a GBT possibly due to stretching the papilla.3 Tall12 and Heins and Wieder13 stated that a certain lateral bone distance between the roots of two adjacent teeth maintains the integrity status of the inter-dental papilla. Tall suggested maintaining 3 mm inter-dental distance to facilitate the foundation of papillae. Martegani et al.14 studied measurement of interproximal width with periapical radiographs. Their statistical analysis concluded that when inter-radicular distance is more than 2.4 mm the presence of full papillae in maxillary anterior teeth becomes less likely. This is regardless of the bone level distance to contact points. Closer root approximation increases the likelihood of full papillae, while if the interdental distance is more than 4 mm then the presence of full papillae is not expected.3
Chang15 categorised the embrasure morphology into four categories based on the horizontal distance between the adjacent cemento-enamel junction (CEJs) (inter-radicular space) and distance from the crest of bone to contact point. His categories confirmed that the interdental width had more of an influence than height.
Chow et al.10 confirmed Chang's findings for central incisors that wider interdental space results in more papilla recession. However, the papillae between the maxillary central and lateral incisors showed an opposite result where wider interdental spaces were more likely to have full papilla. Chen et al.16 contraindicated the results from Cho et al.10 and Martegani et al.14 finding that height is more influential than width.
Distance between inter-proximal contact positions to alveolar bone crest
The distance between the bone crest (BC) and the contact point (CP) is a frequently discussed factor in aesthetics of natural teeth, restorations and in implantology.17 Tarnow18 examined 288 papillae in 30 patients and gathered data from anterior, premolar and molar papillae, based on periodontal sounding. He concluded that if the distance from BC to CP is 5 mm or less, presence of full papillae is almost expectable (98%). Figure 1 illustrates the relationship between the BC-CP distance and the likelihood of the presence of full papillae. Wu et al.9 reproduced Tarnow's study on 200 sites in 45 randomly selected adults investigating maxillary anterior teeth with similar results. Cho et al.3 measured the distance between contact heights to bone crest of 206 sites in 80 patients during a gingival flap procedure in 2006. The slight variation in the results of this study may be due to the different recording procedure, direct observation rather than by probing, or due to the exclusion of subjects with inflammation, a history of orthodontic treatment and malposition teeth. Chen et al.16 also recorded different results compared to Tarnow and Wu with reduced papillary presence for a given dimension. This study measured the distance from BC to CP radiographically in 102 interdental papillae, between maxillary anterior teeth in 30 patients.
Gingival biotype
Siebert and Lindhe19 classified the biotype into 'thin and scalloped' and 'thick and flat' biotypes. Becker et al.20 classified biotype into three groups: flat, scalloped and pronounced scalloped. Scalloped thin tissue is more likely to react to trauma or inflammation by recession while flat-thick tissue reacts with deeper periodontal pockets.21 Restricted blood supply at the papillae tip can interrupt healing resulting in unpredictable repair, whereas thicker tissues respond more favourably due their increased vascularity, which cope better with the inflammatory response.10 Therefore, flat biotype is considered more favourable to achieve papillae fullness than scalloped. Ahmed22 stated that a pronounced scallop, especially with a thin biotype, predisposes to presentation of GBTs more than other types. Chow et al.10 examined papillae fullness in 672 sites in 96 adult patients, concluding that sites with complete papillae have thicker buccal-palatal tissues.10 However, in contrast a study on 333 papillae found no effect of periodontal biotype on the presence of GBTs.23
Differences may be explained by the methods for qualifying thick or thin periodontium as these are often subjective: a periodontal probe in the sulcus can be used to differentiate between biotypes24 while others concluded that trans-sulcular probing was more accurate compared to visual examinations.23
Patient age
Systemic health such as osteoporosis25 as well as age10,15,26 have been suggested as generalised risk factors for presence of GBTs. Ageing results in thinning oral epithelium and reduced keratinisation, which can result in reduced papillae height.
Van der Velden26 presented the changes in the periodontal tissue due to ageing and concluded there is insufficient evidence for physiological gingival or papillae apical migration during ageing. However, he highlighted that periodontal tissue recession due to plaque, inflammation and trauma increases with age and also suggested that periodontal breakdown develops more rapidly due to a slower rate of wound healing.
Vandana & Savitha27 showed the association of thinner tissue with ageing using trans-gingival probing. They associated the thinning periodontium with the increasing effects of traumatic habits and a diminishing of the keratinised layer through ageing. A retrospective study on 60 subjects found that the incidence of GBTs between mandibular central incisors is higher in older patients.28
Diverging roots and post-orthodontic treatment
Burke et al.30 reviewed 500 orthodontics records and highlighted that orthodontic movement of crowded anterior teeth can separate the roots and stretch the inter-dental papilla, increasing the presence of GBTs between incisors after orthodontic treatment. The authors also raised concern regarding orthodontically moving roots very close to each other, jeopardising the interdental bone and interdental papilla due to lack of embrasure space. This may be a risk with the increasing number of techniques that depend on interdental tooth stripping for space creation during alignment.
Tooth morphology
Ahmed mentioned that although triangular shaped teeth have divergent roots with thicker inter proximal bone, which result in less bone loss compared to square-shaped teeth, the incidence of GBTs in square shaped teeth is less than triangular shaped teeth. This was considered to be due to a shorter inter-proximal distance from the osseous crest to the free gingival margin in square-shaped teeth compared to triangular-shaped teeth.22
The design of the contact area in crowns, bridges and any type of restoration effects the interdental area. Taeki5 emphasised proper width and location of contact area in the facial-lingual dimension. He emphasised that the placement of the contact area is related to the marginal ridge contour and dictates the occlusal facial and lingual embrasure form.
Classification of GBTs
A classification system to identify and describe the severity of papillae loss is useful during the patient examination, recording patient records and facilitates monitoring of papillary augmentation techniques. It also assists in communication about the aesthetic concern but they are rarely used in practice.
Nordland & Tarnow31 introduced a classification for papillae loss with four broad categories based on three identifiable anatomical landmarks:
-
1
The inter-dental contact points (IDCP)
-
2
The facial apical extent of the cemento-enamel junction (CEJ)
-
3
The interproximal coronal extent of the CEJ.
Based on their classification, the papillae was described as:
-
Normal: The tip of papillae extends to the apical of IDCP
-
Class 1: The tip of the papillae presents between IDCP and the most coronal extent of inter proximal CEJ
-
Class 2: The tip of the papillae presents at or apical to the inter proximal CEJ but coronal to the apical extent of the facial CEJ
-
Class 3: The tip of the papillae presents level with or apical to the facial CEJ.
Nemcovsky32 introduced a classification system as a papillae index score (PIS) based on a comparison with adjacent teeth:
-
PIS 0: Presence of no papillae and no soft tissue curvature
-
PIS 1: Present papillae height is less half than the present papillae in adjacent teeth within a convex curvature of the soft tissue
-
PIS 2: Presence of at least half the papilla that was not similar with the inter-dental papillae of the proximal teeth and there is no complete harmony with the interdental papillae of the proximal teeth
-
PIS 3: Papilla completely fills the inter-proximal embrasure to the same level as in the adjacent teeth with a complete harmony with the adjacent papillae.
Cardarpoli et al.33 introduced a scoring system as papillae presence index (PPI) based on the visibility of the CEJ:
-
PPI 1: The papilla is completely present and at the same height of the adjacent tooth
-
PPI 2: The papilla is not completely present but interproximal CEJ is not visible
-
PPI 3: The papilla is not completely present and interproximal CEJ is visible
-
PPI 4: The papilla is not completely present and CEJ is visible from buccal and interproximal.
Figure 2 shows a comparison of the indices.
Management
Surgical approaches
Periodontal plastic surgery has a long history in overcoming unsightly GBTs. However, the papillae's poor blood supply is the main limiting factor in all augmentation and reconstruction surgical approaches. As it is known that damaged inter-dental papilla are difficult and sometimes impossible to repair or regenerate5,19 it is essential to preserve the papilla and minimise trauma during any restorative procedure.
Seibert and Lindhe19 classified papillary surgical techniques into: releasing, reflecting and stabilising the papillae. Over the years there have been a number of techniques including different flap designs, the use of bone augmentation and membranes. More recently modified papilla preservation flap (MPPF) and simplified papilla preservation flap (SPPF) in combination with enamel matrix proteins (EMP) and acellular dermal matrix allografts have been used.34,35 EMPs increase protein production in human periodontal ligament cells and have been reported to be effective when used in combination with surgical approaches. Kotchy & Lacky34 have used preservation papilla flaps (MPPF and SPPF) in combination with EMP (enamel matrix protein).
Tissue engineering
With advanced capabilities in tissue engineering, this approach may be less invasive in rectifying the presence of GBTs. Gerus et al.35 performed a study including a surgical approach in combination with the use of an injectable regenerative acellular dermal matrix into insufficient papillae at the same time as the surgery on 12 patients, mean age 55 years with 38 insufficient papillae being treated. There was a reported highly statistically significant improvement in papilla restoration after 5 months.
The injection of periodontal cells with pluripotential capabilities has been used, with fibroblasts in particular to treat both oral and skin defects. One randomised, double blind, placebo-controlled study showed considerable improvement in regaining the lost interdental papilla after injecting extracted fibroblasts harvested from the tuberosity.36
Tissue volumising
Hyaluronic acid (HA) is frequently used as a soft tissue volumiser in facial tissue rejuvenation.37 Based on this, Becker et al.38 evaluated the use of HA to reduce or eliminate GBTs adjacent to dental implants and teeth in the aesthetic zone. A total of 14 GBTs were treated by injecting HA gel 2-3 mm apical to the tip of the papilla up to three times at 3 weeks intervals. The results of this study were promising, even after 25 months and no relapse was apparent. An interesting outcome was the high level of patient satisfaction as all subjects found the whole procedure painless.
Reshaping and restoring tooth shape
The contour of a restoration is important and can affect the papillary space. For example a convex crown can affect the biologic and morphologic features of the interdental gingiva and the scalloped outline of the gingival margins. Restorations can often be designed to have broad contact areas positioned correctly in relation to the bone crest to eliminate a GBT. Bichacho39 stated that when the involved teeth are intact, there is no logical reason for macro-mechanical intervention to close the GBTs, presenting cases using direct and laboratory fabricated restorations showed the importance of the cervical contouring concept in six different aesthetic cases.
Modifying the GBTs by direct adhesive restoration is a non-invasive, viable and affordable option. Figure 3 shows an example of pre- and post-op diastema closure. Tooth whitening was carried out to minimse the visibility of the white spots followed by composite recontouring to close the diastema, positioning the contact area 5 mm from the alveolar crestal bone to encourage the papilla to fill the interproximal space and eliminate a potential GBT following diastema closure.
Using pink restorative materials to mask the GBTs
Composite resin is available in pink shades for gingival reproduction (Fig. 4). It can be used on restorations to replace missing soft tissue. It is considered to be more realistic than pink porcelain in similar situations. Although pink porcelain can mask the loss of inter-dental papilla, the shades and optical properties are limited and it is often better to use darker tooth shades instead (Fig. 5).
Gingival veneer
Removable acrylic or silicone can be used as a gingival veneer to mask GBTs (Fig. 6). This removable prosthesis can also be used to cover the exposed root surfaces due to advanced bone loss especially in patients with a high smile line and to prevent food impaction and phonetic disability. Poor oral hygiene and limitation in manual dexterity are the primary contraindications to consider in using this technique.
There are different methods to make this inexpensive and easy to make prosthesis. The important issue is the retention of the removable veneer into inter-proximal areas that can be achieved by using the gaps as retention grooves or incorporating slotted attachments into the prosthesis. Different terminology is used to describe these appliances: flange prosthesis, gingival veneer prosthesis, removable gingival veneer, acrylic gingival veneer, acrylic periodontal veneer, removable gingival extension and gingival mask.40
Orthodontic movement
Orthodontic movement has several applications in reducing the GBTs. Closing the interdental contacts by conventional orthodontic movement with or without inter-dental stripping reduces the BC-CP distance. However the length of treatment, the need for appliances and cost are limiting factors. Salama and Salama41 suggested that paralleling closed roots with orthodontic movements may be beneficial in supporting the inter-dental papillae. Burke et al.2 recommend bringing the roots closer by mesial torquing movement to rectify presence of GBTs. In conjunction with orthodontic treatment, proximal enamel can be recontoured to change the contact area to a broader surface along with relocating the contact more apically.
Based on the data illustrated in Figure 1 the less distance there is between the inter-proximal contact and the bone crest, the less likely will be the presence of a GBT. Extrusive and intrusive tooth movement can maintain the alveolar bone level and reduce GBTs.42
Cardaropoli et al.33 presented a study evaluating a combined approach of orthodontic-periodontal treatment to reconstruct the inter-dental papillae between upper central incisors, demonstrating that the soft tissues adapted to the new emergence profiles during intrusion of the teeth as the inter-proximal spaces were reduced.
Conclusion
This review highlights the aetiology and management of GBTs adjacent to natural teeth. GBTs are caused by lack of presence of the inter-dental papillae, which is multifactorial including the position of the alveolar crest and the teeth. Orthodontics can both cause and be used to treat GBTs. The presence of a GBT can have a negative impact on dental aesthetics as well as impact on the health of the gingiva and phonation. Recognising the early signs of papilla loss and its monitoring by the dental practitioner and the application of preventive measures can be part of the good clinical practice. Management should be considered with every proximal restoration and can include non-invasive tooth recontouring. Novel approaches including the use of HA need further investigation.
References
Takei H, Yamada H, Hau T . Maxillary anterior aesthetics. Preservation of the inter-dental papillae. Dent Clin North Am 1989; 33: 263–273.
Burke S, Burch J, Tetz J . Incidence and size of pretreatment overlap and post-treatment gingival embrasure space between maxillary central incisors. Am J Orthod Dentofacial Orthop 1994; 105: 506–511.
Cho H S, Jang H S, Kim D K et al. The effect of inter-proximal distance between roots on the existence of interdental papillae according to the distance from the contact point to the alveolar crest. J Periodontol 2006; 77: 1651–1657.
Gonzalez M, Almeida A, Greghi S, Mondelli J, Moreno T . Interdental papillary house; a new concept and guide for clinicians. Int J Periodontics Restorative Dent 2011; 31: 6: e87–e93.
Takei H . The interdental space. Dent Clin North Am 1980; 24: 169–176.
Kokich V, Kiyak A, Shapiro P . Comparing the perception of dentists and lay people to altered dental aesthetics. J Esthet Dent 2005; 1: 311–324.
Cunliffe J, Pretty I . Patient's ranking of interdental “black triangles” against other common aesthetic problems. Eur J Prosthodont Restor Dent 2009; 17: 177–181.
Kurt J, Kokich V G . Open gingival embrasures after orthodontic treatment in adults: prevalence and aetiology. Am J Orthod Dentofacial Orthop 2001; 120: 116–123.
Wu Y J, Tu Y K, Huang S M, Chang C P . The influence of the distance from the contact point to the crest of bone on the presence of the interproximal dental papilla. Chang Gung Med J 2003; 26: 822–828.
Chow Y C, Eber R M, Tsao Y P, Shotwell J L, Wang H L . Factors associated with the appearance of gingival papillae. J Clin Periodontol 2010; 37: 719–727.
Sharma A A, Park J H . Esthetic considerations in interdental papilla: remediation and regeneration. J Esthetic Restor Dent 2010; 22: 18–28.
Tal H . Relationship between the interproximal distance of roots and the prevalence of bony pockets. J Periodontol 1984; 55: 604–607.
Heins P J, Wieder S M . A histologic study of the width and nature of inter-radicular spaces in human adult pre-molars and molars. J Dent Res 1986; 65: 948–951.
Martegani P, Silvestri M, Mascarello F et al. Morphometric study of the interproximal unit in the esthetic region to correlate anatomic variables affecting the aspect of soft tissue embrasure space. J Periodontal 2007; 12: 2260–2265.
Chang L C . The association between embrasure morphology and central papilla recession. J Clin Periodontol 2007; 34: 432–436.
Chen M C, Liao Y F, Chan C P, Ku Y C, Pan W L, Tu Y K . Factors influencing the presence of interproximal dental papillae between maxillary anterior teeth. J Periodontol 2010; 81: 318–324.
Palmer R M, Farkondeh N, Palmer P J, Wilson R F . Astra Tech single-tooth implants: an audit of patient satisfaction and soft tissue form. J Clin Periodontol 2007; 34: 633–638.
Tarnow D P, Magner A W, Fletcher P . The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol 1992; 63: 995–996.
Seibert J, Lindhe J . Esthetics and periodontal therapy: textbook of clinical periodontology. 2nd ed. Copenhagen: Munksgaard, 1989.
Becker W, Ochsenbein C, Tibbetts L, Becker B E . Alveolar bone anatomic profiles as measured from dry skulls. Clinical ramifications. J Clin Periodontol 1997: 24: 727–731.
Kao R T, Fagan M C, Conte G J . Thick vs. thin gingival biotypes: A key determinant in treatment planning for dental implants. J Calif Dent Assoc 2008; 36: 193–198.
Ahmed I . Anterior dental aesthetics: gingival perspective. Br Dent J 2005; 199: 195–202.
Rafiee R M, Melamed S, Chao J . Predicting black triangles. part ii interdental width. J West Soc Periodontol Periodontal 2012; 60: 3–5.
Kan J Y, Rungcharassaeng K, Morimoto T, Lozada J . Facial gingival tissue stability after connective tissue graft with single immediate tooth replacement in the esthetic zone: Consecutive case report. J Oral Maxillofac Surg 2009; 67: 40–48.
Shum I, Leung P C, Kwok A et al. Periodontal conditions in elderly men with and without osteoporosis or osteopenia. J Periodontol 2010; 81: 1396–1402.
Van der Velden U . Effect of age on the periodontium. J Clin Periodontol 1984; 11: 281–294.
Vanadana K L, Savitha B . Thickness of gingival in association with age, gender and dental arch location. J Clin Periodontol 2005; 32: 828–830.
Ikeda T, Yamaguchi M, Meguro D, Kasai K . Prediction and causes of open gingival embrasure spaces between the mandibular central incisors following orthodontic treatment. Aust Orthod J 2004; 20: 87–92.
Novak M J, Albather H M, Close J M . Redefining the biologic width in severe, generalized, chronic periodontitis: implications for therapy. J Periodontol 2008; 79: 1864–1869.
Burke S, Burch J, Tetz J . Incidence and size of pretreatment overlap and post-treatment gingival embrasure space between maxillary central incisors. Am J Orthod Dentofacial Orthop 1994; 105: 506–511.
Nordland W P, Tarnow DP . A classification system for loss of papillary height. J Periodontol 1998; 69: 1124–1126.
Nemcovsky C . Interproximal papilla augmentation procedure: A novel surgical approach and clinical evaluation of 10 consecutive procedures. Int J Periodontics Restorative Dent 2001; 21: 553–559.
Cardaropoli D, Stefania Re, Corrente G . The papilla index (PPI): A new system to assess interproximal papillary levels. Int J Periodontics Restorative Dent 2004; 24: 488–492.
Kotschy P, Laky M . Reconstruction of supracrestal alveolar bone lost as a result of severe chronic periodontitis. Five year outcome: case report. Int J Periodontics Restorative Dent 2006; 26: 424–431.
Gerus N, Romanos A, Vassilopoulos P, Reddy M . Dermal graft for use in inter-proximal papilla regeneration. Int J Periodontics Restorative Dent 2012; 32: 49–58.
McGuire K, Scheyer E T . A randomized, double-blind, placebo-controlled study to determine the safety and efficacy of cultured and expanded autologous fibroblast injections for the treatment of interdental papillary insufficiency associated with the priming procedure. J Periodontol 2007; 78: 4–17.
Rohrich Rod J, Ghavami A, Crosby M A . The role of hyaluronic acid fillers (restylane) in facial cosmetic surgery: review and technical consideration. Plast Reconstr Surg 2007; 120: 41S–54S.
Becker W, Gabitov I, Stepanov M, Kois J, Smidt A, Becker B . Minimally invasive treatment for papillae deficiencies in the aesthetic zone: a pilot study. Clin Implant Dent Relat Res 2010; 12: 1–8.
Bichacho N . Papilla regeneration by noninvasive prosthodontic treatment: segmental proximal restorations. Pract Periodontics Aesthet Dent 1998; 10: 75, 77–78.
Alani A, Maglad A, Nohl F . The prosthetic management of gingival aesthetics. Br Dent J 2011; 210: 63–69.
Salama H, Salama M . The role of orthodontic extrusive remodelling in the enhancement of soft and hard tissue profiles before implant placement: a systematic approach to the management of extraction site defects. Int J Periodontics Restorative Dent 1993; 13: 312–333.
Thailander B . Infrabony pockets and reduced alveolar bone height in relation to orthodontic therapy. Semin Orthod 1996; 2: 55–61.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Ziahosseini, P., Hussain, F. & Millar, B. Management of gingival black triangles. Br Dent J 217, 559–563 (2014). https://doi.org/10.1038/sj.bdj.2014.1004
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.1004