Key Points
-
Highlights the clinical outcomes of patients prescribed bisphosphonates following dento-alveolar procedures.
-
Assesses the parameters and risks of developing a bisphosphonate-related osteonecrosis of the jaws (BRONJ).
-
Compares the risk factors of developing a BRONJ to previously published data.
Abstract
Aim The aim of this retrospective study was to examine the outcome of patients referred to a dedicated clinic for dental extractions while they were prescribed either oral or intra-venous (IV) bisphosphonates (BPs). The following parameters were assessed: mode of BP administration, indication for BP prescription, incidence of BRONJ, concomitant risk factors for development of bisphosphonate-related osteonecrosis of the jaws (BRONJ) and demographic details.
Material and methods The clinical records of 225 patients who underwent dental extraction while receiving oral or intravenous bisphosphonates were reviewed. Their clinical outcome, specifically the development of BRONJ was determined.
Results Of the 225 patients, 202 were prescribed oral and 23 IV BPs. 34.8% (8/23) of patients prescribed IV BPs developed BRONJ following dental extraction, which was a significantly (p <0.001) higher proportion than that of the oral BP group, which was 2.5% (5/202 patients). 12.3% (8/65) patients taking BPs with steroids were at a significantly increased risk of a BRONJ (p <0.003). 12.3% (7/57) males developed a BRONJ compared with 3.6% (6/168) females where p = 0.015. All of the patients who developed a BRONJ as a result of oral BP prescription had been taking this medication for three years or more.
Conclusion In our patient cohort the risk of developing a BRONJ following dental extractions was greatest in those patients receiving IV BPs and those on oral BPs with concomitant steroid medication.
Similar content being viewed by others
Introduction
The cohort of patients prescribed bisphosphonate therapy has increased significantly in the last 15 years. Bisphosphonates (BPs) are potent inhibitors of bone resorption and remodelling. Their action results in a dose dependent apoptosis of osteoclasts with increasing concentration.1 The most common indications for their use are osteoporosis, osteopenia, multiple myeloma, Paget's disease and the presence of skeletal metastases from prostate, breast, renal and lung cancers.
Intravenous and oral bisphosphonates
BPs may be administered orally or intravenously. Oral bisphosphonates are generally prescribed for patients with osteoporosis or osteopenia, although an increasing number of osteoporotic patients are being prescribed an annual infusion of an intravenous bisphosphonate. The intravenous (IV) BPs, zoledronate and pamidronate, are currently used for the management of hypercalcaemia and treatment of symptomatic bone lesions associated with multiple myeloma and metastatic cancers. Clodronate disodium is another IV BP currently used for metastatic lesions although its use is not currently licensed in the UK.
What is BRONJ? (Bisphosphonate-related osteonecrosis of the jaw)
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is the now well recognised complication of bisphosphonate therapy, first described by Marx in 2003.2 BRONJ is diagnosed when the following three criteria are met:3,4
-
1
Exposed bone in the maxillofacial region that is present for eight weeks or more
-
2
Current or previous bisphosphonate use
-
3
No history of radiation therapy to the jaws.
The incidence of BRONJ in patients on oral BPs has been reported to vary from 0.01-0.06%. The previously reported incidence for patients on IV BPs has ranged from 0.8-12%.3,5,6,7
Risk Factors for developing BRONJ
Drug related
-
Bisphosphonate potency – the more potent the bisphosphonate, the higher the risk of BRONJ. BPs with a nitrogen side chain are more potent than those without. The IV BPs with nitrogen side chains used for the treatment of cancers are more potent than oral agents. Zoledronate is more potent than pamidronate3,8,9
-
Duration of therapy – a positive correlation has been shown between the duration of BP therapy and the incidence of BRONJ.3,8,9,10
Local factors
-
Dentoalveolar surgery – extractions, dental implants, periapical surgery, periodontal surgery5,12,13,14
-
Anatomy – prominent tori, mylohyoid ridge
-
Poorly fitting dentures.
Age and race
Age has been shown as a significant risk factor in some studies. Two retrospective studies showed age was an increasing risk.11,12 Race has been reported to be a possible risk factor, with Caucasians being identified as having an increased risk.3
Systemic factors
-
Systemic factors – concomitant diseases such as diabetes, renal dialysis, obesity, hypothyroidism and low haemoglobin increase the risk of BRONJ development3,8,9
-
Medications – chemotherapeutic agents, corticosteroids and immunosuppressants9,13,14,15 have been shown in some, but not all, studies to predispose to an increased incidence of BRONJ.
Social factors
Smoking has been shown to cause an increase in the risk of BRONJ, this risk increases with the length of time the patient has been smoking.
Bacterial colonisation
Investigators have observed multiple species of bacteria on biofilms of affected bone within BRONJ. The following bacteria have been identified at such sites: Fusobacterium, Bacillus, Actinomyces, Staphylococcus, Streptococcus, Selemonas, Treponemes and Candida.16 Actinomyces has been reported as the bacteria most commonly found in samples of BRONJ.15 This will influence the type of antimicrobial therapy used to treat BRONJ.
Genetic factors
Studies have shown that gene diversity influences the incidence of BRONJ in multiple myeloma patients. Polymorphisms on CYP2C8 gene can affect the incidence of BRONJ.17
Treatment protocols
There are many international published guidelines on the prevention and management of BRONJ.18 These report a variety of strategies involving conservative treatment, non-surgical treatment and surgical management that may be local or radical.
Purpose of study
The purpose of this study was to assess the following in a cohort of patients attending for dental extractions while on bisphosphonate therapy:
-
Mode of BP administration
-
Indication for BP prescription
-
Incidence of BRONJ
-
Presence of previously recorded risk factors for BRONJ development – type of drug, length of time on drug and systemic factors
-
Gender and age.
Patients and method
This retrospective study examined treatment outcomes for 225 patients referred to the specialist bisphosphonate clinic at King's College Dental Hospital (KCH) from August 2007-January 2011. All patients had been prescribed oral or intravenous bisphosphonates and underwent dental extractions. Data, including incidence of BRONJ, concomitant risk factors for developing a BRONJ and patient demographics were stored and analysed in the computer software SPSS. Chi-square analysis was used to determine whether mode of BP administration, gender and concomitant risk factors: diabetes, steroids and smoking, were significant in the development of BRONJ. The significance of age was examined using a Mann-Whitney test.
Screening protocol
Patients taking BPs were referred by colleagues in other departments within the dental hospital, oncology, rheumatology, orthopaedic outpatient clinics and by general medical and dental practitioners. Patients were initially assessed by a multidisciplinary team including two oral surgeons and two consultants in restorative dentistry. Following clinical and radiographic examination an appropriate treatment plan was formulated. The aim of this was to optimise oral health and restore as much of the dentition as possible, thus avoiding the need for dental extractions, a risk factor for the subsequent development of BRONJ. Any teeth deemed unrestorable were extracted.
Informed consent was obtained from patients before extractions. The aetiology, risks and possible sequelae of developing a BRONJ were discussed at length and documented on the consent form. The patients were informed that if a BRONJ occurred and was symptomatic they may require long-term antimicrobial therapy or further surgery to facilitate the removal of necrotic bone if sequestra were identified.
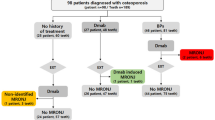
Patients
Dental extractions (single or multiple) were performed in 225 patients. Twenty-three patients were on IV BPs and 202 were taking oral BPs.
Extraction protocol
Patients were managed by the authors of this paper from initial assessment through to follow-up and discharge. The dental extractions were performed under local anaesthesia (LA) or LA supplemented with intravenous sedation. An atraumatic extraction technique with the use of periotomes, luxators and the sectioning of teeth to preserve the socket anatomy and minimise the destruction to the adjacent alveolus was utilised. Sockets were irrigated copiously with saline to ensure elimination of all debris from the sockets.
Postoperatively, patients were prescribed 200 mg metronidazole three times (tds) daily for seven days (patients with known allergy or contraindication to metronidazole were prescribed 500 mg amoxicillin tds daily for seven days). Metronidazole was selected as the antibiotic of choice as current literature suggests gram negative or facultative anaerobes are predominantely found in BRONJ specimens. 0.12% chlorhexidine mouthwash 10 ml four times (qds) daily was supplied for two weeks and analgesics (600 mg ibuprofen, or 1 g paracetemol, qds). If a patient's denture was in contact with the surgical area, they were advised not to wear it until complete healing had occurred.
Review appointments were arranged at two weeks, two months, six months and one year. If the patient was symptomatic or on IV BPs review appointments were arranged more frequently.
Management of cases with BRONJ
Patients presenting with stage 0 or stage 1 disease
Asymptomatic exposed bone was treated with 0.12% chlorhexidine mouthwash qds and reviewed at monthly intervals.
Patients presenting with stage 2 or 3 (no pathologic fractures/oro-cutaneous fistulae/bone sequestra present)
Patients were prescribed the following:
-
0.12% chlorhexidine mouthwash, qds
-
Metronidazole 400 mg, tds, seven days then Augmentin 625 mg, tds seven days or Augmentin 625 mg, tds, 14 days.
If patients were still symptomatic after 14 days then they were prescribed:
-
0.12% chlorhexidine mouthwash, qds
-
Doxycycline 100 mg, od, (can be taken long term) or Levofloxacin 500 mg, od, during symptomatic phases.
In patients with persistent evidence of infection, radiographs and cone beam CT (CBCT) were performed to confirm the presence of bone sequestra and assess the size, position of necrotic bone and the proximity to adjacent structures.
Patients were reviewed at two weekly intervals until symptoms resolved.
Patients with stage 2 or 3 disease with bone sequestra
Patients were managed as above but surgical intervention was required to remove the sequestra. Mucoperiosteal flaps were reflected, to allow sequestrectomy and debridement. Primary closure was achieved. Specimens were sent for histopathological examination to confirm the presenting diagnosis and exclude malignancy. A specimen was also sent for microbiological investigation. Postoperatively, 0.12% chlorhexidine mouthwash qds and antibiotics were prescribed according to the previous regimen. The patient was reviewed two weeks following the surgical procedure and at this appointment histopathology and microbiology results were reviewed. The progress of soft tissue healing at the surgical site was assessed and then reviewed on a monthly basis, unless acute symptoms necessitated more frequent visits.
Results
Two hundred and twenty-five patients seen on the bisphosphonate clinic underwent dental extractions.
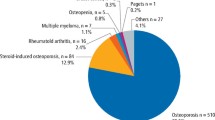
Mode of administration and indication for BP prescription
Two hundred and two patients were on oral BPs and 23 patients were on IV BPs.
Of the 202 patients on oral BPs, 193 (95.5%) were prescribed this for osteoporosis, 2 (1%) for the management of metastatic disease, 5 (2.5%) patients were undergoing treatment for multiple myeloma, 1 (0.5%) for Paget's disease and 1 (0.5%) for ankylosing spondylitis.
Of the 23 patients on intravenous bisphosphonates, nine (39.1%) were prescribed this for osteoporosis, ten (43.5%) for the management of metastatic disease, two (8.7%) for Paget's disease and two (8.7%) for ankylosing spondylitis.
Incidence of BRONJ
Chi-square analysis showed a highly significant difference for the development of a BRONJ between patients on IV BPs and those on oral BPs, p <0.001 (Table 1).
Risk factors
-
In our patient cohort there was no significant increase in the risk of developing a BRONJ in patients with diabetes or those who smoked (Table 2)
-
Chi-square analysis demonstrated a significantly increased risk of developing a BRONJ in patients prescribed both steroids and BPs (Table 2)
-
The duration of oral BP therapy exceeded three years in all five patients who developed a BRONJ while taking this medication (Table 3).
Gender
Male patients were at a significantly increased risk of developing a BRONJ compared to the female cohort, p <0.015 (Table 4).
Age
Age was not a significant factor in the development of BRONJ. The Mann-Whitney test was used due to the small number of patients with BRONJ below the age of 65 years, p = 0.0677 (Table 5).
Discussion
The purpose of this study was to examine the factors predisposing a cohort of patients in our clinic to developing a BRONJ and to compare this with previously documented data.
Mode of administration and indication for bisphosphonate prescription
The most common reason for patients being prescribed BPs was osteoporosis. Two hundred and two of the 225 (89.8%) patients studied were prescribed bisphosphonates for this purpose. Of these, 193 (95.5%) were on oral medication while 9 patients (4.5%) had received an annual intravenous infusion. It was noted that patients receiving IV BPs for osteoporosis were encountered more frequently during the last 18 months of the study. In 2007 the FDA approved the use of an annual infusion of zoledronate for osteoporosis. The increased prescription of a single annual infusion is associated with reduced oesophageal irritation, which may limit the use of oral BPs and is less reliant on patient compliance.
Zoledronate was the most commonly prescribed IV BP in the patient cohort reported here. This is the most potent of all the BPs, but only one of the nine patients on IV BPs for the treatment of osteoporosis developed a BRONJ after extraction. This patient had also been on oral bisphosphonates for three years before the introduction of the annual infusion of zoledronate.
Metastatic disease was the second most common reason that patients were prescribed BPs and the majority of patients in this group received this intravenously. This finding correlates with other published data about the use of BPs and their clinical efficacy, which is well established in the treatment of bone metastases and hypercalcaemia.
Incidence of BRONJ
The incidence of BRONJ for patients on oral BPs has varied in published reports from 0.01-0.06%.3 Within our cohort of patients this rate was found to be considerably higher with 5 of the 202 (2.5%) patients developing a BRONJ. All the patients who developed a BRONJ while taking oral BPs in our study also had other risk factors (duration of treatment exceeding three years or concomitant steroids) known to increase the risk of developing BRONJ (see Table 3). It is unclear in other published literature whether the reported incidence of BRONJ relates to a cohort of patients who had other contributing risk factors. In this study all five patients who developed BRONJ were on corticosteroids for many years and had also been on BPs for three years or more. Our findings are consistent with studies demonstrating a positive correlation between the incidence of BRONJ and duration of BP therapy.5,12,13,14,16,17,18 The use of concomitant steroids has been documented to increase the incidence of BRONJ although some studies have not supported this. In the current study there was a significant correlation between steroid use and development of a BRONJ, p = 0.003 (Table 2).
The development of a BRONJ in patients treated with IV BPs in previous studies has varied between 0.8%-12%.5 Eight of the 25 patients (34.8%) on IV BP treatment in our cohort developed a BRONJ, a significantly higher rate than those on oral BPs, p <0.001. This corresponds with previous findings that the IV BPs are more potent and cause a significantly greater increase in BRONJ development than oral agents. All the patients in our series who had metastatic bone disease had also been exposed to chemotherapeutic agents. Previous studies have indicated that patients who have been treated with such drugs are at greater risk of developing a BRONJ, although others have failed to demonstrate such an effect. Further investigation is required to determine whether this is a significant factor in the development of BRONJ for patients with metastatic disease. The reported incidence of BRONJ in our cohort was significantly higher than reported in previous studies, but previous studies have been estimates of the cumulative incidences of BRONJ taken from case series, case controlled and cohort studies. The patients in our cohort had been prescribed concomitant chemotherapeutic agents and doses varied from 5-60 infusions, whereas in previous studies no other risk factors were mentioned.
Risk factors
In this study diabetic patients did not appear to be at a significantly increased risk of developing a BRONJ, which contradicts findings reported by other authors.3,8,9
In our group, patients prescribed steroid medication and a BP were at a significantly greater risk of developing a BRONJ than those who were not on steroids. Smoking has previously been reported as a risk factor in the development of a BRONJ. We found no significant difference in the incidence of BRONJ between smokers and non-smokers.
Gender
In this sample a significantly greater proportion of male patients developed a BRONJ when compared to the incidence in females. Five of the seven males who developed a BRONJ were on IV BPs for prostate cancer, one for renal cell carcinoma and one had been prescribed oral BPs to manage a steroid induced osteoporosis for ten years. Of the 23 patients in our group on IV BPs 14 were male. Previous studies5 found that gender was not a significant factor in the development of BRONJ and it may be that in our study it was the route of administration and reason for prescription, that is, mainly IV BPs for metastatic prostate cancer, which was more of a determinant of a BRONJ development than gender. This finding, however, was only significant when comparing this single factor and the sample was not big enough to allow for multifactorial analysis. In future studies with larger numbers of patients it may be possible to investigate whether males on IV BPs are more likely to develop BRONJ than females on a similar regimen.
Age
In our study increasing age did not appear to be a significant factor in the development of a BRONJ.
Conclusion
This study showed a highly significant risk of developing a BRONJ for patients on IV BPs undergoing dental extractions. Further studies are required with a larger sample size so that the other significant factors can be identified and multifactorial analysis can be carried out, to analyse the other significant factors, which together can contribute to developing a BRONJ.
Screening strategies are increasingly being publicised in the medical field on prevention of BRONJ. Patients for whom BP therapy is being considered should be sent for a dental examination and those requiring treatment should ideally have surgical intervention before starting treatment.
References
Assael L A . Oral bisphosphonates as a cause of bisphosphonate-related osteonecrosis of the jaws: clinical findings, assessment of risks, and oreventative strategies. J Oral Maxillofac Surg 2009; 67(Suppl 5): 35–43.
Marx R E . Pamidronate (Aredia) and zoledronate (Zometa) induced vascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 2003; 61: 1115–1117.
Ruggiero S L, Dodson T B, Assael L A et al. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaw - 2009 update. J Oral Maxillofac Surg 2009; 67(Suppl 5): 2–12.
Khosla S, Burr D, Cauley J et al. Bisphosphonate-associated osteonecrosis of the jaws: a report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2007; 22: 1479–1491.
Lo J C, O'Ryan F S, Gordon N P et al. Prevalence of osteonecrosis of the jaw in patients with oral bisphosphonate exposure. J Oral Maxillofac Surg 2010; 68: 243–253.
Rogers S N, Hung J, Barber A J, Lowe D . A survey of consultant members of the British Association of Oral and Maxillofacial Surgeons regarding bisphosphonate-induced osteonecrosis of the jaws. Br J Oral Maxillofac Surg 2009; 47: 598–601.
Mavrokokki T, Cheng A, Stein B, Goss A . Nature and frequency of bisphosphonate-associated osteonecrosis of the jaws in Australia. J Oral Maxillofac Surg 2007; 65: 415–423.
Dodson T B . Intravenous bisphosphonate therapy and bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg 2009; 67: 44–52.
Madrid C, Bouferrache K, Abarca M, Jaques B, Broome M . Bisphosphonate-related osteonecrosis of the jaws: how to manage cancer patients. Oral Oncol 2010; 46: 468–470.
Wessel J H, Dodson T B, Zavras A I . Zoledronate, Smoking and obesity are strong risk factors for osteonecrosis of the jaws: a case-control study. J Oral Maxillofac Surg 2008; 66: 625–631.
Badros A, Weikel D, Salama A et al. Osteonecrosis of the jaw in multiple myeloma patients: clinical features and risk factors. J Clin Oncol 2006; 24: 945–952.
Jadu F, Lee L, Pharoah M, Reece D, Wang L . A retrospective study assessing the incidence, risk factors and comorbidities of pamidronate-related necrosis of the jaws in multiple myeloma patients. Ann Oncol 2007; 18: 2015–2019.
Chiu C T, Chiang W F, Chuang C Y, Chang S W . Resolution of oral bisphosphonate and steroid-related osteonecrosis of the jaw - a serial case analysis. J Oral Maxillofac Surg 2010; 68: 1055–1063.
Oliver R . Bisphosphonates and oral surgery. Oral Surg 2009; 2: 56–53.
Kos M, Kuebler J F, Luczak K, Engelke W . Bisphosphonate-related osteonecrosis of the jaws: a review of 34 cases and evaluation of risk. J Craniomaxillofac Surg 2010; 38: 255–259.
Sedghizadeh P P, Kumar S K, Gorur A, Schaudinn C, Shuler C F, Costerton J W . Identification of microbial biofilms in osteonecrosis of the jaws secondary to bisphosphonate therapy. J Oral Maxillofac Surg 2008; 66: 767–775.
Sarasquete M E, González M, San Miguel J F, García-Sanz R . Bisphosphonate-related osteonecrosis: genetic and acquired risk factors. Oral Dis 2009; 15: 382–387.
McLeod N M, Patel V, Kusanale A, Rogers S N, Brennan P A . Bisphosphonate osteonecrosis of the jaw: a literature review of UK policies versus international policies on the management of bisphosphonate osteonecrosis of the jaw. Br J Oral Maxillofac Surg 2011; 49: 335–342.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Taylor, T., Bryant, C. & Popat, S. A study of 225 patients on bisphosphonates presenting to the bisphosphonate clinic at King's College Hospital. Br Dent J 214, E18 (2013). https://doi.org/10.1038/sj.bdj.2013.327
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2013.327
This article is cited by
-
Electron microscopic analysis of necrotic bone and failed implant surface in a patient with medication-related osteonecrosis of the jaw
Maxillofacial Plastic and Reconstructive Surgery (2023)
-
Efficacy of hyaluronic acid, absorbable collagen sponge, and their combination in minimizing bisphosphonate-related osteonecrosis of the jaws (BRONJ) after dental extraction: a preliminary animal histomorphometric study
Maxillofacial Plastic and Reconstructive Surgery (2022)
-
Considerations for restorative dentistry secondary care referrals - part 1: defining strategic importance
British Dental Journal (2022)
-
Significance of medication discontinuation on bisphosphonate-related jaw osteonecrosis in a rat model
Scientific Reports (2022)
-
The incidence of medication-related osteonecrosis of the jaw following tooth extraction in patients prescribed oral bisphosphonates
British Dental Journal (2021)