Key Points
-
Highlights that osteoporosis affects the bone mineral density of the mandible and maxilla and has been associated with premature tooth loss.
-
Reports that the most plausible mechanism suggests an increased susceptibility to periodontal disease in osteoporotic patients.
-
Stresses that the full impact of osteoporosis, and its treatment, on oral health remains poorly understood.
Abstract
Background There is evidence to suggest osteoporosis may result in premature tooth loss. The pathology behind this relationship is poorly understood. A correlation with osteoporosis and greater susceptibility to periodontal disease has been suggested.
Objectives To investigate the association between osteoporosis and periodontal disease, accounting for the effect of confounding variables of age, smoking status and oral hygiene.
Setting Three hundred and fifty-nine postmenopausal women aged 45-70 years were recruited from the Greater Manchester area between March 2008 and June 2010.
Subjects and methods Data were collected on osteoporosis status, smoking status, pocket probing depths, suppuration, plaque, bleeding and calculus indices. Dental panoramic tomographs were taken and periodontal bone support assessed on all teeth. Data were analysed using SPSS software (version 20).
Results Complete data were available for 348 patients. Twenty-six percent (91) of individuals were osteoporotic. Logistic regression was used. The relationship between osteoporosis status and moderate to severe periodontal disease of both molar teeth and the whole mouth was not significant (p = 0.088 and p = 0.296 respectively).
Conclusions Osteoporosis is not a causal factor in the development of moderate to severe chronic periodontitis.
Similar content being viewed by others
Introduction
Osteoporosis affects more women than men and is a disease defined by a reduction in bone mineral density of 2.5 standard deviations or more below the mean peak bone mass for young adult women. It is a common disease that increases in prevalence with age. Studies have demonstrated that osteoporosis affects the jaw bones, with cortical thinning and an increasing sparseness of the cancellous bone. There is increasing evidence that such changes in bone micro-architecture may have implications for oral health. Resorption of alveolar bone may be more severe in edentulous individuals with osteoporosis.1,2 Darcey et al. demonstrated that there was an increased risk of molar tooth loss in those with osteoporosis.3 This is supported by previous research that osteoporosis may have an influence on untimely tooth loss.4,5,6,7
As the evidence remains equivocal it has been difficult to demonstrate an aetiological mechanism behind this relationship. Several theories have been postulated focusing upon the interaction with the periodontal disease process. It has been proposed that lower vitamin D and raised RANKL (a factor known to induce osteoclastic action and thus resorption of bone) may be associated with periodontal disease.8 Vitamin D insufficiency and raised RANKL are both intimately related to osteoporosis, with the result that osteoporosis may exacerbate an already present chronic periodontitis.9 The consequence: an elevated resorptive potential of alveolar bone. The use of vitamin D and calcium supplements has been shown to have a positive effect on periodontal health,10 as has hormone replacement therapy.11 It seems plausible that this combination of increased susceptibility to resorption of bone and elevated inflammatory responses in osteoporotic patients may result in an increased progression of periodontal disease. Therefore in patients with osteoporosis and chronic periodontitis one may expect to see an increased mean periodontal attachment loss if both diseases act synergistically.
The primary aim of this study was to assess whether there is a relationship between periodontal disease of molar teeth and osteoporosis status. Oral hygiene, smoking status and age are known to influence the development of periodontal disease and their effect was accounted for in the analysis. The secondary aim was to assess whether there is a relationship between the presence of generalised periodontal disease and osteoporosis status, accounting for the same covariates.
Materials and methods
This was a cross-sectional observational study. The study was approved by the Local Research Ethics Committee. To achieve a power of 80% at the 0.05 significance level 540 patients were required to demonstrate a 10% difference in the prevalence of periodontal disease between the osteoporotic group and non-osteoporotic group. Patients were recruited from Manchester and the surrounding regions between March 2008 and June 2010. To be eligible for inclusion patients must have been aged 45-70 years and undergone dual energy X-ray absorptiometry (DXA) of the proximal femur and lumbar spine within the previous three months. Exclusion criteria were all systemic conditions that may influence periodontal disease progression for example, uncontrolled diabetes and pregnancy. Furthermore, conditions that prevented participants' ability to understand and consent to the study were excluded, including psychiatric disorders. No volunteers presented with such exclusion criteria. Informed consent was taken for all participants. Data collection ended in August 2010. At each stage, only one examiner was used to prevent inter-examiner error and variation in classifying periodontal disease.
All patients received a full oral examination at the University Dental Hospital of Manchester. One operator (HS) undertook the clinical examinations. Full pocket charting was undertaken with a Florida Probe (Florida Probe Corporation, Florida, USA). The presence of bleeding and suppuration was recorded. The FRAX system was used to gather data on risk factors for osteoporosis. This included smoking status, alcohol consumption and the use of hormone replacement therapy (HRT). More information about FRAX and a full description of the study design can be found in our previous publication.3
Plaque and calculus indices were calculated following the system suggested by Green and Vermillion.12 A tooth from each sextant was selected (the first molar and central incisor). The plaque score is classified from zero to three. Zero demonstrates no plaque. A score of 'one' denotes plaque covering no greater than one third of the tooth surface, 'two' plaque greater than one third but less than two thirds of the tooth and 'three' indicates plaque covering greater than two thirds of the tooth. The same scoring system was used to classify the presence of calculus. Each tooth was given a buccal and lingual score. An index for plaque and calculus was calculated as the mean score for all the teeth examined. The Green and Vermillion Oral Hygiene Index (OHI) was calculated for each patient based upon the addition of plaque indices and calculus indices.
A dental panoramic radiograph was taken of each patient using a Planmeca PM2002CC (Planmeca Oy, Helsinki, Finland), Kodak GP Storage Phosphor Screens (Carestream Health Inc, New York, USA) and a Direct View CR850 digital processor (Carestream Health Inc, New York, USA). Patients were radiographed wearing an acrylic stent incorporating a 4 mm diameter steel ball-bearing in the premolar region. One operator (DL) using magnification and illumination assessed the periodontal attachment levels in each radiograph. The distance from the cement-enamel junction (CEJ) to crestal bone height was measured at the mesial and distal sites (interproximal sites) of each tooth. The measurement was then adjusted for magnification using the ball bearing as a reference point.
All interproximal sites were classified as healthy, mild, moderate or severely affected by periodontal disease according to the distance from CEJ to the crestal bone. If greater than 30% of the total sites were graded as moderate to severely affected, the patient was re-classified as having a generalised, severe form of chronic periodontal disease. If greater than 30% of molar sites demonstrated moderate to severe attachment loss, the patient was re-classified as having generalised severe, chronic periodontal disease affecting the molars. Thirty percent of sites affected is a common threshold in the UK for considering periodontal disease to be generalised. A comparison was made between those with no or mild periodontal disease with those with more severely affected teeth using osteoporotic and smoking status, age and oral hygiene as predictive variables.
Impacted teeth, implants, retained roots and edentulous patients were not included in the analysis.
Statistical analysis
The Statistical Package for Social Sciences 20 (SPSS, Chicago, USA) was used to undertake the statistical analyses. Logistic regression was undertaken for both primary and secondary dependent variables (severe periodontal disease affecting molars and generalised periodontal disease). A logistic model was selected as the outcome variables were dichotomous and the data was not normally distributed. Age, smoking status, oral hygiene and osteoporosis status were used as the independent variables in the regression model. The first part of the logistic regression uses Chi-square testing to assess the significance of each variable independently with the presence of periodontal disease. If an independent variable is not significantly correlated to periodontal disease it will not be incorporated into the regression. Following this, a stepwise model was used for theory testing. This sequentially adds the independent variables into the regression. It then removes each variable and observes the effect upon the final model of removing that variable. If the removal of a variable makes a significant difference to how well the model fits the observed data, that variable is kept in the model. The Wald criterion demonstrates the contribution of that variable to the outcome. If the removal of a variable does not change the model, it is removed from the regression model automatically and that variable is not predictive of periodontal disease. Statistical significance was set at p = 0.05. Casewise diagnostics were performed on outliers.
Results
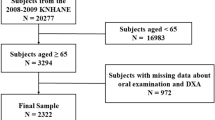
A total of 359 patients were recruited. Of these complete data were available for 348 (Table 1). The bar chart in Figure 1 demonstrates the percentage of total sites with moderate and severe periodontal disease against osteoporosis status.
Molar periodontal disease and osteoporosis status
The total number of patients for analysis was 348. The initial chi-square test demonstrated osteoporosis status was not significant (p = 0.088) and thus not used in the regression model. A test of the remaining model against a constant model was statistically significant indicating that the remaining independent variables reliably predict the presence of molar periodontal disease. (Chi-square: 57.34, p <0.001.) The Wald criterion demonstrated smoking status, age and oral hygiene can significantly predict periodontal disease. (Wald values: 7.28 p = 0.007, 28.94 p <0.001 and 12.18 p <0.001) The Hosmer and Lemeshow Test was non-significant (p = 0.190) indicating the regression model fits the data. Prediction success overall was 67%. Casewise diagnostics highlighted three outlying cases not fitting the model. These were checked, found to be accurate and left within the model.
Generalised periodontal disease and osteoporosis status
The total number of patients for analysis was 348. Using the chi-square statistic, all variables (smoking status, age, osteoporotic status and oral hygiene) demonstrated a significant association with periodontal disease and could thus be used in the logistic regression (osteoporosis and periodontal disease p = 0.039). When introduced to the stepwise logistic regression osteoporosis status was no longer significant (p = 0.296). A test of the remaining model against a constant model was statistically significant indicating that the remaining independent variables reliably predict the presence of generalised periodontal disease. (Chi-square: 56.62, p <0.001) The Wald criterion demonstrated smoking status, age and oral hygiene can significantly predict periodontal disease. (Wald values: 9.50 p = 0.002, 22.57 p <0.001 and 15.40 p <0.001) The Hosmer and Lemeshow Test was non-significant (p = 0.136) indicating the regression model fits the data. Prediction success overall was 69.5%. Casewise diagnostics highlighted two cases not fitting the model. These were checked, found to be accurate and left within the model.
Summary
The regression model was good. In both analyses osteoporosis status was not included in the statistical model indicating that it is not a significant predictor of generalised periodontal disease. In both analyses smoking, age and oral hygiene were predictive of the presence of generalised periodontal disease.
Discussion
There is a growing body of evidence to demonstrate the oral impact of reduced bone mineral density. This mostly stems from observational studies on tooth loss and osteoporosis.3,5,6,7,13,14,15,16 In these studies age is often a confounder.5,7 This generates a significant complication: it becomes more difficult to extrapolate the precise cause of tooth loss. Have the teeth been lost through lifestyle choices such as smoking and/or diet or is the cause more intimately related to a systemic predisposition for alveolar bone and attachment loss; osteoporosis?
In this study there was no evidence for an effect of osteoporosis in predicting those affected by periodontal disease; smoking status, age and oral hygiene are the main significant predictor variables. The higher percentage of patients in the osteoporotic group with severe periodontal disease can be explained by these other factors. Thus we can conclude that osteoporosis does not contribute to periodontal disease.
When considering mechanisms behind possible associations, the link between periodontal disease and osteoporosis provides the most rational model. As with this study, assessment of attachment loss radiographically has been performed in several studies. Many have demonstrated correlations between a radiographic reduction in alveolar bone height and osteoporosis.17,18,19,20 Clinical assessment of attachment loss and data on osteoporosis status have yielded mixed results but some have further supported the correlation.14,21,22 There are, however, limitations with many of these studies that must be recognised.
-
Most studies are limited to menopausal women; there is little data on males
-
Very few studies are longitudinal, most are single point cross-sectional surveys studies. Periodontal disease and osteoporosis are both chronic diseases, characterised by slow progression over time. It does not, however, follow that both diseases were present for any length of time before assessment in a longitudinal study. There is some evidence to suggest increased periodontal disease over time in osteoporotic patients but these studies have flaws.23,24 The study by Swoboda et al.24 was limited by a small sample size and the self-reported nature of the patients' osteoporosis status. Yoshihara et al.23 followed a larger sample size but the inclusion criteria were very restrictive, excluding smokers and diabetics. Furthermore, there was no data upon the oral hygiene of the patients
-
It is difficult to control for confounders given the complex, multi-factorial nature of both diseases. As with tooth number, age and smoking are significant confounders. Once controlled for, the results of many studies become insignificant. Most observational studies assessing oral links to the disease exclude patients undergoing treatment for osteoporosis as this confounds any observation between primary disease and clinical outcomes
-
Most are single centre studies thus outcomes may only be applied to that cluster and are not necessarily generalisable to the population as a whole
-
Matching of osteoporotic groups to non-osteoporotic groups is not always undertaken to ensure comparability
-
Differences in methodology between studies precludes direct comparison, which further limits the generalisability of conclusions.
In addition, there is a body of evidence that would refute any association (though it must be acknowledged these studies suffer the same methodological limitations).25,26,27
This data further supports the outcome of these studies that demonstrate no correlation between periodontal disease and osteoporosis. Furthermore, this model would not appear to explain the findings of our earlier study that demonstrated a greater number of molar tooth loss in osteoporotic patients. This study has strengths: although single centre, the recruitment covered a large geographic area of the North West of England. A larger number were recruited than other comparable studies.18,19,25,26,28,29,30 Both osteoporosis status data and periodontal disease data were robust. In the latter both clinical and radiographic data were used including a broad range of indices. There are, however, limitations of this study that may increase the likelihood of a type II error: falsely accepting that osteoporosis is not correlated to periodontal disease. The most notable of which is the power of the study. This study is known to be underpowered. Other limitations of the study can be found in a previous paper.3
The logistic regression model presents results in a classification table. This estimates what percentage of outcomes is explained by the model used. A 100% outcome would suggest the model completely predicts the outcome. In this study the classification table results were 67% for molar periodontal disease and 69.5% for generalised periodontal disease. This would indicate the models are reasonable but do not fully explain the outcomes of periodontal disease found. It is essential when constructing any regression model that all known covariates are included. Without such input, though, the influence of known variables may be assessed, but only limited conclusions may be drawn about the relationship. The covariates of periodontal disease risk used in this model were limited. Diabetes status, genetic influences, stress and specific bacterial composition have all been demonstrated as integral to periodontal disease progression.31,32,33 Furthermore, there exists multiple local factors such as imbrication, furcational exposure and overhanging restorations that have all been shown to influence localised inflammatory responses. In this study only smoking status, oral hygiene, age and osteoporosis status were included in the regression model. Thus it must be acknowledged that some known covariates were not included in the regression.
Using this model and data set there is no correlation between periodontal disease, either generalised of the entire dentition or localised to the molar teeth and osteoporosis status. The significance of the chi-square in the initial generalised disease modeling should not be overlooked. This indicates that osteoporosis may have an influence upon periodontal disease. Were this not to be the case it would not have been significant at this stage of the model and so rejected from inclusion into the regression. It may be reasoned that the correlation of the other variables: smoking, age and oral hygiene are so dominant in the regression that osteoporosis status is 'pushed out'.
Conclusion
In this study, osteoporosis was not a causal factor for generalised moderate to severe periodontal disease.
Implications for research: evidence for a correlation between osteoporosis and periodontal disease remains equivocal. Further multi-centre, prospective, longitudinal studies are required to assess the impact of osteoporosis upon oral health and investigate further the biological mechanisms underlying any associations.
Implications for practice: clinicians should continue to follow standard protocols for the management of periodontal disease in patients with osteoporosis. Consideration must be given to more intensive supportive periodontal therapy where there is evidence of more advanced disease.
References
Klemetti E, Vainio P . Effect of bone mineral density in skeleton and mandible extraction of teeth and clinical alveolar height. J Prosthet Dent 1993; 69: 21–25.
Bays R A, Weinstein R S . Systemic bone disease in patients with mandibular atrophy. J Oral Maxillofac Surg 1982; 40: 270–272.
Darcey J, Horner K, Walsh T, Southern H, Marjanovic E J, Devlin H . Tooth loss and osteoporosis: to assess the association between osteoporosis status and tooth number. Br Dent J 2013; 214: E10.
Aström J, Bäckström C, Thidevall G . Tooth loss and hip fractures in the elderly. J Bone Joint Surg Br 1990; 72: 324–325.
Drozdzowska B, Pluskiewicz W, Michno M . Tooth count in elderly women in relation to their skeletal status. Maturitas 2006; 55: 126–131.
May H, Reader R, Murphy S, Khaw K T . Self-reported tooth loss and bone mineral density in older men and women. Age Ageing 1995; 24: 217–221.
Nicopoulou-Karayianni K, Tzoutzoukos P, Mitsea A et al. Tooth loss and osteoporosis: the osteodent study. J Clin Periodontal 2009; 36: 190–197.
Jabbar S, Drury J, Fordham J, Datta H K, Francis R M, Tuck S P . Plasma vitamin D and cytokines in periodontal disease and postmenopausal osteoporosis. J Periodontal Res 2011; 46: 97–104.
Hildebolt C F, Pilgram T K, Dotson M et al. Estrogen and/or calcium plus vitamin D increase mandibular bone mass. J Periodontal 2004; 75: 811–816.
Miley D D, Garcia M N, Hildebolt C F et al. Cross-sectional study of vitamin D and calcium supplementation effects on chronic periodontitis. J Periodontal 2009; 80: 1433–1439.
Hildebolt C, Pilgram T, Yokoyama-Crothers N et al. The pattern of alveolar crest heigh change in healthy postmenopausal women after 3 years of hormone/oestrogen replacement therapy. J Periodontal 2002; 73: 1279–1284.
Greene J, Vermillion J . The oral hygiene index: a method of classifying oral hygiene status. J Am Dent Assoc 1960; 61: 10.
Gur A, Nas K, Kayhan O et al. The relation between tooth loss and bone mass in postmenopausal osteoporotic women in Turkey: a multicentre study. J Bone Miner Metab 21: 43–47.
Inagaki K, Kurosu Y, Kamiya T et al. Low metacarpal bone density, tooth loss, and periodontal disease in Japanese women. J Dent Res 2001; 80: 1818–1222.
Krall E, Garcia R, Dawson-Hughes B. Increased risk of tooth loss is related to bone loss at the whole body, hip, and spine. Calcif Tissue Int 1996; 59: 433–437.
Taguchi A, Tanimoto K, Suei Y, Wada T . Tooth loss and mandibular osteopenia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 79: 127–132.
Erdogan O, Incki K K, Benlidayi M E, Seydaoglu G, Kelekci S . Dental and radiographic findings as predictors of osteoporosis in postmenopausal women. Geriatr Gerontol Int 2009; 9: 155–164.
Payne J, Reinhardt R, Nummikoski P, Patil K . Longitudinal alveolar bone loss in postmenopausal osteoporotic/osteopenic women. Osteoporosis Int 1999; 10: 34–40.
Tezal M, Wactawski-Wende J, Grossi S, Ho A, Dunford R, Genco R . The relationship between bone mineral density and periodontitis in postmenopausal women. J Periodontal 2000; 71: 1492–1498.
Brennan-Calanan R, Genco R, Wilding G, Hovey K, Trevisan M, Wactawski-Wende J. Osteoporosis and oral infection: independent risk factors for oral bone loss. J Dent Res 2008; 87: 323–327.
Brennan R, Genco R, Hovey K, Trevisan M, Wactawski-Wende J. Clinical attachment loss, systemic bone density, and subgingival calculus in postmenopausal qomen. J Periodontal 2007; 78: 2104–2111.
Ronderos M, Jacobs D R, Himes J H, Pihlstrom B L . Associations of periodontal disease with femoral bone mineral density and oestrogen replacement therapy: cross-sectional evaluation of US adults from NHANES III. J Clin Periodontal 2000; 27: 778–786.
Yoshihara A, Seida Y, Hanada N, Miyazaki H . A longitudinal study of the relationship between periodontal disease and bone mineral density in community-dwelling older adults. J Clin Periodontal 2004; 31: 680–684.
Swoboda J R, Kiyak H A, Darveau R, Persson G R . Correlates of periodontal decline and biologic markers in older adults. J Periodontal 2008; 79: 1920–1926.
Lundstrom A, Jendle J, Setenstrom B, Toss G, Ravald N . Periodontal conditions in 70-year-old women with osteoporosis. Swed Dent J 2001; 25: 89–96.
Weyant R, Pearlstein M, Churak A, Forrest K, Famili P, Cauley J . Effect of postmenopausal hormone replacement therapy on dental outcomes: systematic review of the literature and pharmacoeconomic analysis. J Periodontal 1999; 70: 982–991.
Elders P, Habets L, Netelenbos J, Van der Linden L, Van der Steld P . The relation between periodontitis and systemic bone mass in women between 46 and 55 years of age. J Clin Periodontal 1992; 19: 492–496.
Von Wowern N, Klausen B, Kollerup G . Osteoporosis: a risk factor in periodontal diease. J Periodontal 1994; 65: 1076–1084.
Streckfus C F, Johnson R B, Nick T, Tsao A, Tucci M . Comparison of alveolar bone loss, alveolar bone density and second metacarpal bone density, salivary and gingival crevicular fluid interleukin-6 concentrations in healthy premenopausal and postmenopausal women on oestrogen therapy. J Gerontol A Biol Sci Med Sci 1997; 52: M343–M51.
Reinhardt R, Payne J, Maze C, Patil K, Gallaher S, Mattson J . Influence of oestrogen and osteopenia/osteo-porosis on clinical periodontitis in postmenopausal women. J Periodontal 1999; 70: 823–828.
Michalowicz B, Diehl S, Gunsolley J et al. Evidence of a substantial genetic basis for risk of adult periodontitis. J Periodontal 2000; 71: 1699–1707.
Croucher R, Marcenes W, Torres M . The relationship between life events and periodontitis: a case control study. J Clin Periodontal 1997; 24: 39.
Emrich L, Shlossman M, Genco R . Periodontal disease in non-insulin dependent diabetes mellitus. J Periodontal 1991; 62: 123–131.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Darcey, J., Devlin, H., Lai, D. et al. An observational study to assess the association between osteoporosis and periodontal disease. Br Dent J 215, 617–621 (2013). https://doi.org/10.1038/sj.bdj.2013.1191
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2013.1191
This article is cited by
-
Repercussions of osteoporosis on the maxillofacial complex: a critical overview
Journal of Bone and Mineral Metabolism (2021)
-
Initial changes in alveolar bone volume for sham-operated and ovariectomized rats in ligature-induced experimental periodontitis
Clinical Oral Investigations (2016)
-
Low bone mineral density in young individuals is associated with greater gingival inflammation and recession
Rheumatology International (2014)