Key Points
-
Serves as a reminder of a rare but significant complication.
-
Highlights timing and presentation of the event.
-
Summarises potential risk factors and measures to minimise them.
-
Describes the treatment options.
-
Illustrates the role of the dentist in the management.
Abstract
Immediate and late mandibular fractures are a rare complication of third molar removal. We analysed 130 cases of mandibular fractures following removal of impacted third molars reported in the literature, including four managed in the maxillofacial unit and identified potential risk factors. Its occurrence is likely to be multi-factorial, with age, gender, angulation, laterality, extent and degree of impaction and associated pathologies contributing to the risk of fracture. Postoperative fractures were more common than intra-operative fractures (2.7:1) and occurred most frequently in the second and third weeks (57%). A 'cracking' noise was the most frequent presentation (77%). Intra-operative fractures were more frequent among females (M:F – 1:1.3), and differed from postoperative fractures (M:F – 3.9:1). This study analyses the results, providing suggestions to minimise the risk and to manage a mandibular fracture following removal of a third molar.
Similar content being viewed by others
Introduction
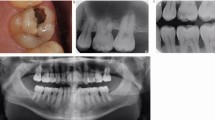
Removal of third molars is a common surgical procedure carried out by a dental surgeon and can result in a variety complications, which include dry socket, bleeding, infection, trismus and nerve damage.1,2,3 Mandibular fracture is rare, but a very serious complication following third molar removal with a reported incidence of 0.0033% to 0.0049%.4,5,6 These fractures could occur in the intra-operative or postoperative period and can cause significant distress to the patient and the practitioner (Figs 1,2). Most publications in the literature are in the form of isolated case reports and small case series,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22 which makes the evaluation of potential risk factors difficult. In this study, we analysed 130 cases of mandibular fractures following third molar removal reported in the literature, including 4 cases managed in the local maxillofacial unit, and seek to identify potential risk factors and preventive measures.
Materials and methods
We undertook a Medline search covering the period 1970–2011 and identified English articles in the literature, which reported the occurrence of mandibular fractures following removal of third molars. The search terms and strategy is documented in Table 1. We selected articles which documented original patient data and included four patients treated in the maxillofacial unit, which together form the basis of this analysis.
Titles and abstracts of all relevant articles published in the literature were screened. Full text analysis of potentially relevant publications was performed and included a hand search of their bibliography. Articles providing original patient information were selected for analysis.
The factors analysed were the demographic details of the patients, side of fracture, extent of impaction (Pell and Gregory),23 angulation (vertical, horizontal, mesioangular, distoangular), degree of impaction (partial/full),23 associated pathologies, type of anaesthesia employed for tooth removal, presentation of fracture, time to fracture and management of fracture.
Results
The search strategy identified 113 potential articles, which were analysed further to see if they conformed to the inclusion criteria (Table 1). A total of 18 articles, which reported original patient data on 126 cases were identified and listed in Table 2.5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22 The details of the four patients treated in our unit are presented in Table 3. A summary of all post- and intra-operative mandibular fractures following wisdom tooth removal is presented in Table 4.
Demographic details
The age and sex of the patient were documented in 123 and 129 cases respectively.
There was an overall male predominance, with a male:female ratio of 2.4:1. Intra-operative fractures were more common among females (M:F – 1:1.3) and postoperative fractures were more common among males (M:F – 3.9:1). The age range of subjects was from 19 to 79 years of age, with a peak incidence in the 36 to 60-year age group. Intra-operative fractures occurred over the age range of 26 to 79 years, with a peak incidence in the 36 to 45-year age group. Postoperative fractures occurred between 20 and 78 years of age, with a peak incidence in the 36 to 60-year age group.
Side of fracture
Details of the side of fracture were documented in 53 cases. Postoperative fractures occurred more frequently on the right side (right:left – 1.9:1) and intra-operative fractures were more common on the left side (right:left – 1:1.6). Three fractures were bilateral.
Angulation (vertical, horizontal, mesioangular and distoangular)
The angulation of the tooth was documented in 101 cases. Fractures occurred most frequently in the mesioangular (32.6%) and least frequently in the distoangular (12.8%) group.
Degree of impaction (partial/full)
The degree of impaction was noted in 92 cases. Mandibular fractures occurred most frequently following removal of fully impacted teeth (72%).
Extent of impaction (Pell and Gregory classification)23
The extent of impaction was documented in 41 cases. Mandibular fractures were more common in the Class II/III and Type B/C compared to Class I and Type A impactions. Intra-operative and postoperative fractures were more common following the removal of Class II and Type C impactions.
Associated pathologies
Pre-operation infective episodes associated with the wisdom tooth were documented in 63 cases. The others pathologies included cysts (10 cases), enlarged follicle (14 cases) and postoperative infection (4 cases).
Type of anaesthesia employed for tooth removal
The type of anaesthesia employed to remove the wisdom teeth was documented in 37 cases and was distributed between general (17) and local (20) anaesthesia.
Presentation of fracture
The mode of presentation of the fracture was documented in 88 cases. Sixty-eight patients (77%) noted a 'cracking' noise at the time of fracture. Ten patients presented with a history of pain/swelling (11%), five patients with a history of trauma (5%), four with malocclusion (4.5%) and two with numbness (2%).
Time of fracture
The time of fracture was documented in 118 cases and occurred postoperatively in 86 cases and intra-operatively in 32 cases (postoperative:intra-operative – 2.7:1). Postoperative fractures occurred between the following 1 and 70 days and were most frequent in the second and third weeks (57%).
Treatment of fracture
The management of the fractured mandible was noted in 92 cases and included a range of modalities. Thirty-nine cases (42%) were treated by closed reduction/intermaxillary fixation (IMF), 28 (30%) by open reduction and internal fixation (ORIF), 9 (10%) by ORIF + IMF and 16 (17%) by soft diet.
Discussion
Fracture of the mandible is a rare but recognised complication following lower third molar removal. Accurate estimates are difficult to ascertain, though questionnaire reports suggest an incidence of between 0.0033% and 0.0049%.4,5,6 Various factors have been implicated in the increased frequency of mandibular fractures.5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,24
Our case series and those reported in the literature confirm increasing age as a predictor of mandibular fractures, with a peak incidence in the 36–60 year age group.5,6,9,10,21 Wisdom teeth were most frequently removed in patients below 25 years of age,1,2,25 whereas mandibular fractures in this age group were not the most common. The decreased elasticity, risk of osteoporosis, bone atrophy, greater potential of tooth ankylosis, higher incidence of pathologies, postoperative complications and the prolonged healing phase, have all been considered to contribute to the increased risk of mandibular fractures in the older age group.9,10,11,19,26,27 Though the total number of fractures in the above 60 year age group was small (15 patients, 12%), the relative frequency of fracture is likely to be much higher, as only a small proportion of patients have their wisdom teeth removed in this age group (5–10%).28,29 There was a higher frequency of fractures among males which is thought to be secondary to the increased masticatory forces generated5,6,30 and the increased risk of trauma.
Mandibular fractures were more common following removal of mesioangular, vertical, horizontal and distoangular teeth respectively and were similar to the relative frequency of these impactions in the general population (mesioangular (45%), vertical (40%), horizontal (10%) and distoangular (5%)).31 The angulation of the wisdom tooth has been reported as a factor determining the difficulty of removal, with mesioangular, horizontal/vertical and distoangular impactions considered to be progressively more difficult.31 This review does not support a direct relationship between the presumed difficulty of removal based on angulation and the risk of mandibular fracture. The relatively increased risk of fractures associated with horizontal impactions could be related to the need for additional bone removal and deeper point of application often required.32
Mandibular fractures were in general, more common following removal of right sided wisdom teeth (right:left – 1.8:1), though interestingly intra-operative fractures were more common following removal of left sided teeth (right:left – 1:1.6). It is difficult to explain the association between laterality and the risk of mandibular fractures.
The degree (partial/complete) and the extent (Pell and Gregory)23 of impaction were found to be predictors of mandibular fractures.5,6,9,10,13,21 Fully impacted and Class B/C and Type II/III impactions were more frequently associated with mandibular fractures. These teeth proportionally occupy a greater volume of the mandibular bone and their extraction is likely to necessitate more bone removal, resulting in a reduction in the remaining bone stock and weakening of the mandible, predisposing it to fractures.5,6,9,10,13 Buccal bone, especially along the external oblique ridge, provides significant strength to the mandibular angle and its removal to facilitate extraction further weakens the mandible. Awareness of these factors and attempts to minimise the amount and location of bone removed by judicious tooth/root division can potentially reduce the risk of fractures. Garcia et al.33 did not find Pell and Gregory classification to be useful in predicting the difficulty of wisdom teeth removal and Renton et al.32 found patient factors also played an important role in determining the difficulty of removal.
Pre-operative infections associated with the impacted tooth have been suggested to predispose to postoperative fractures.5,9,12,21 All patients in our series had episodes of infection before tooth removal. In the United Kingdom, where only symptomatic wisdom teeth are currently considered for removal in line with the NICE guidelines,34 it is interesting that only two previous reports of fractures have been recorded in the last 29 years.7,8 Large cysts can cause 'significant' reduction in the bone volume and predispose to fractures, though this should be obvious pre-operatively. Severe postoperative infections and osteomyelitis can similarly cause bone resorption and result in a pathological fracture.5,15 The use of pre- or postoperative antibiotics and their relationship to mandibular fractures was not always available in the reported articles.
Postoperative fractures were much more frequent than intra-operative fractures (postoperative:intra-operative – 2.7:1) and the magnitude of this discrepancy has not always been highlighted in the previous reports. Postoperative fractures occurred most frequently (57%) in the second and third week following tooth removal.5,6,20 Most patients reported a crack (77%), history of trauma or pain/swelling before the fracture. This period would be consistent with the predominantly osteoclastic phase of bone healing.26 In these circumstances, excessive masticatory forces and relatively minor trauma could precipitate a fracture and account for the increased frequency in this postoperative period.5,6,20 Al-Belasy et al., however, did not find any relationship between masticatory forces and mandibular fractures following removal of wisdom teeth.35
Intra-operative fractures were more common in the 26-45 year age group and differed from postoperative fractures, which were more common in the 36–60 year age group. Intra-operative fractures were more common in females (M:F – 1:1.3), and markedly differed to the male predominance of postoperative fractures (M:F – 3.9:1). This has not been reported in the previous studies and highlights the merit of analysing a large group of patients. Some authors have suggested that intra-operative fractures are subsequent to improper instrumentation, excessive use of force and poor technique.9,20 Though it has been suggested that poor technique is a potential cause of iatrogenic mandibular fracture, there is little information about the specific techniques used in these reports. In current practice, the bone removal and tooth division is performed by high speed surgical handpieces and the tooth/root fragments extirpated with fine elevators. Grau–Monclas et al. reported that the use of the Winter's elevator was associated with intra-operative fractures.21 These large, thick elevators allow the application of significant force and their use should be avoided whenever possible and if necessary, should be restricted to experienced clinicians. Intra-operative fractures were more frequent following removal of complete, Class II/III and Type C impactions, which often require more bone removal and do not afford the margin for poor technique before a fracture. Poor technique along with the thinner mandible in females might contribute to the increased frequency of fractures in this group. Minimal bone removal with greater reliance on appropriate tooth division and gentle elevation, using 'finger' pressure, should be the norm for the removal of all wisdom teeth and 'difficult' wisdom teeth in particular.
Diagnosis of postoperative fractures can be difficult, with only a small minority presenting with obvious malocclusion. Initial radiographs can fail to reveal a fracture and a high index of suspicion and repeat imaging a few days later may be necessary to visualise the fracture line.13,20 This could account for some of the delayed 'presentation' in the postoperative group.
Mandibular fractures following wisdom teeth removal were treated by differing modalities. Interestingly, the majority of fractures (58%) were managed 'conservatively' with soft diet, IMF/closed reduction. Open reduction internal fixation (30%) and additional intermaxillary fixation (10%) were utilised in the remaining cases. The reasons for this discrepancy is not obvious in the reported cases, but could include the obvious diagnosis and configuration of the fracture, easier access to instrumentation, personnel and theatre time in the case of intra-operative fractures and the relative lack of symptoms, malocclusion and delayed presentation in the case of postoperative fractures.
The risk of fractures can be minimised by accurate diagnosis, thorough assessment of the difficulty of extraction, identifying high risk patients and formulating a comprehensive treatment plan, which includes the most appropriate surgical approach, extent and location of bone removal, sectioning of the tooth and the necessity for prophylactic plating. A sensitive surgical technique is mandatory and in the case of deeply impacted/displaced teeth, consideration should be given to prophylactic plating or an extra-oral approach.36,37 Coronectomy, which has principally been evaluated in relation to minimising the risk of damage to the inferior dental nerve,38 might have a role in decreasing the risk of mandibular fracture associated with deeply impacted teeth. Postoperative care should include a soft diet and avoidance of trauma/contact sports for at least four weeks.
Mandibular fractures following third molar removal should be in large part predictable, even if not preventable. Informed consent for patients with a risk of fracture is mandatory. Patient education as regards to its likely timing (2–3 weeks), presenting characteristics ('cracking noise', pain/swelling, altered bite) and the necessity to seek immediate help is essential and in keeping with good clinical practice.
Finally, the maintenance of accurate and contemporaneous notes cannot be overstressed. The patient should be fully informed of the events and arrangements made for immediate transfer to the maxillofacial unit, in case of the fracture occurring/presenting to a dental practitioner. In the case of the event occurring/presenting in the hospital, arrangements must be made for the patient to be evaluated by a senior practitioner and decisions made of the most appropriate management. In both circumstances, it is also prudent to inform and seek advice from the dental/medical insurance provider (Table 5).
References
Goldberg M H, Nemarich A N, Marco W P . Complications after mandibular third molar surgery: a statistical analysis of 500 consecutive procedures. J Am Dent Assoc 1985; 111: 277–279.
Osborn T R, Frederickson G Jr, Small I A, Torgerson T S . A prospective study of complications related to mandibular third molar surgery. J Oral Maxillofac Surg 1985; 43: 767–769.
Bouloux G F, Steed M B, Perciaccante V J . Complications of third molar surgery. Oral Maxillofac Surg Clin North Am 2007; 19: 117–128.
Alling C C, Alling R D . Indications for management of impacted teeth. In Alling C C, Helfrick J F, Alling R D (eds) Impacted teeth. pp 46–64. Philadelphia: W B Saunders, 1993.
Perry P A, Goldberg M H . Late mandibular fracture after third molar surgery: a survey of Connecticut oral and maxillofacial surgeons. J Oral Maxillofac Surg 2000; 58: 858–861.
Libersa P, Roze D, Cachart T, Libersa J C . Immediate and late mandibular fractures after third molar removal. J Oral Maxillofac Surg 2002; 60: 163–165.
de Silva B G . Spontaneous fracture of the mandible following third molar removal. Br Dent J 1984; 156: 19–20.
Dunstan S P, Sugar A W . Fractures after removal of wisdom teeth. Br J Oral Maxillofac Surg 1997; 35: 396–397.
Iizuka T, Tanner S, Berthold H, Mandibular fractures following third molar extraction. A retrospective clinical and radiological study. Int J Oral Maxillofac Surg 1997; 26: 338–343.
Krimmel M, Reinert S . Mandibular fracture after third molar removal. J Oral Maxillofac Surg 2000; 58: 1110–1112.
Wagner K W, Otten J E, Schoen R, Schmelzeisen R . Pathological mandibular fractures following third molar removal. Int J Oral Maxillofac Surg 2005; 34: 722–726.
Werkmeister R, Fillies T, Joos U, Smolka K . Relationship between lower wisdom tooth position and cyst development, deep abscess formation and mandibular angle fracture. J Craniomaxillofac Surg 2005; 33: 164–168.
Komerik N, Karaduman A I . Mandibular fracture 2 weeks after third molar extraction. Dent Traumatol 2006; 22: 53–55.
Kunkel M, Kleis W, Morbach T, Wagner W . Severe third molar complications including death-lessons from 100 cases requiring hospitalization. J Oral Maxillofac Surg 2007; 65: 1700–1706.
Wagner K W, Schoen R, Wongchuensoontorn C, Schmelzeisen R . Complicated late mandibular fracture following third molar removal. Quintessence Int 2007; 38: 63–65.
Woldenberg Y, Gatot I, Bodner L . Iatrogenic mandibular fracture associated with third molar removal. Can it be prevented? Med Oral Patol Oral Cir Bucal 2007; 12: E70–E72.
Khan A A, Banerjee A, Mbamalu D . Mandibular fracture caused by mastication. Emerg Med J 2009; 26: 153.
Valiati R, Ibrahaim D, Poli V D, Heitz C, Pagnoncelli R M, Silva D N . Mandibular fracture during mandibular third molar extraction. Internet J Dent Sci 2009; 6(2). Online article available at http://www.ispub.com/journal/the-internet-journal-of-dental-science/volume-6-number-2/mandibular-fracture-during-mandibular-third-molar-extraction.html (accessed January 2012).
Kao Y H, Huang I Y, Chen C M, Wu C W, Hsu K J, Chen C M . Late mandibular fracture after lower third molar extraction in a patient with Stafne bone cavity: a case report. J Oral Maxillofac Surg 2010; 68: 1698–1700.
Chrcanovic B R, Custódio A L . Considerations of mandibular angle fractures during and after surgery for removal of third molars: a review of the literature. Oral Maxillofac Surg 2010; 14: 71–80.
Grau-Manclús V, Gargallo-Albiol J, Almendros-Marqués N, Gay-Escoda C . Mandibular fractures related to the surgical extraction of impacted lower third molars: a report of 11 cases. J Oral Maxillofac Surg 2011; 69: 1286–1290.
Cankaya A B, Erdem M A, Cakarer S, Cifter M, Oral C K . Iatrogenic mandibular fracture associated with third molar removal. Int J Med Sci 2011; 8: 547–553.
Pell G J, Gregory B T . Impacted mandibular third molars: Classification and modified techniques for removal. Dent Digest 1933; 39: 330–338.
Bodner L, Brennan P A, McLeod N M . Characteristics of iatrogenic mandibular fractures associated with tooth removal: review and analysis of 189 cases. Br J Oral Maxillofac Surg 2011; 49: 567–572.
Scottish Intercollegiate Guidelines Network. Management of unerupted and impacted third molar teeth. A national clinical guideline. SIGN 43. Edinburgh: SIGN, 2000. Online article available at http://www.sign.ac.uk/pdf/sign43.pdf.
Amler M H . The age factor in human extraction wound healing. J Oral Surg 1977; 35: 193–197.
Bruce R A, Frederickson G C, Small G S . Age of patients and morbidity associated with mandibular third molar surgery. J Am Dent Assoc 1980; 101: 240–245.
Haug R H, Perrott D H, Gonzalez M L, Talwar R M . The American Association of Oral and Maxillofacial Surgeons age-related third molar study. J Oral Maxillofac Surg 2005; 63: 1106–1114.
Chuang S K, Perrott D H, Susarla S M, Dodson T B . Age as a risk factor for third molar surgery complications. J Oral Maxillofac Surg 2007; 65: 1685–1692.
Miyaura K, Matsuka Y, Morita M, Yamashita A, Watanabe T . Comparison of biting forces in different age and sex groups: a study of biting efficiency with mobile and non mobile teeth. J Oral Rehabil 1999; 26: 223–227.
Miloro M, Ghali G E, Larsen P E, Waite P (eds). Peterson's principles of oral and maxillofacial surgery. 2nd ed. USA: PMPH-USA, 2004.
Renton T, Smeeton N, McGurk M . Factors predictive of difficulty of mandibular third molar surgery. Br Dent J 2001; 190: 607–610.
Garcia A G, Sampedro F G, Rey J G, Vila P G, Martin M S . Pell–Gregory classification is unreliable as a predictor of difficulty in extracting impacted lower third molars. Br J Oral Maxillofac Surg 2000; 38: 585–587.
NICE. Guidance on the extraction of wisdom teeth, TA1 2000. London: National Institute for Health and Clinical Excellence, 2000.
Al-Belasy F A, Tozoglu S, Ertas U . Mastication and late mandibular fracture after surgery of impacted third molars associated with no gross pathology. J Oral Maxillofac Surg 2009; 67: 856–861.
Abu-El Naaj I, Braun R, Leiser Y, Peled M . Surgical approach to impacted mandibular third molars – operative classification. J Oral Maxillofac Surg 2010; 68: 628–633.
Pippi R, Solidani M, Broglia S, Cristalli M P . Prevention of mandibular fractures caused by difficult surgical extractions: report of a borderline case. J Oral Maxillofac Surg 2010; 68: 1162–1165.
Renton T, Hankins M, Sproate C, McGurk M . A randomised controlled clinical trial to compare the incidence of injury to the inferior alveolar nerve as a result of coronectomy and removal of mandibular third molars. Br J Oral Maxillofac Surg 2005; 43: 7–12.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Ethunandan, M., Shanahan, D. & Patel, M. Iatrogenic mandibular fractures following removal of impacted third molars: an analysis of 130 cases. Br Dent J 212, 179–184 (2012). https://doi.org/10.1038/sj.bdj.2012.135
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2012.135
This article is cited by
-
Bucco alveolar bone thickness of mandibular impacted third molars with different inclinations: a CBCT study
Surgical and Radiologic Anatomy (2020)
-
Potentially disastrous
British Dental Journal (2012)