Key Points
-
Recent research has revealed an alteration of the oral microcirculation in patients with BMS.
-
Acupuncture influences oral microcirculation, resulting in a significant variation of the vascular pattern associated with a significant reduction of the burning sensation after three weeks of therapy.
-
Reduction of the burning sensation was permanent for the 18 months following the acupuncture therapy.
Abstract
Background Burning mouth syndrome is a chronic pathology of unknown ethiopathogenesis. The aim of this study was to evaluate whether acupuncture can produce a reduction of the burning sensation by influencing the oral microcirculation.
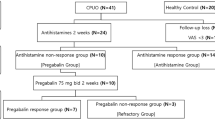
Methods Thirty patients (10 male and 20 female; mean age ± SD = 65.4 ± 2.17) and 30 healthy subjects (10 male and 20 female; mean age ± SD = 62.06 ± 6.72) were recruited for the study. The patients were treated with acupunctural techniques based on traditional Chinese medicine. Microcirculation was observed in vivo using videocapillaroscopy at three different times: t0) in the absence of acupuncture; t1) 1 minute after the insertion of the needles; and t2) 5 minutes after the insertion of the needles and following their stimulation.
Results The capillaroscopic observation revealed a significant increase of the capillary tortuousness and density, a reduction of the arborescence and a reduction of burning sensation in such patients.
Conclusion The study shows that acupuncture influences oral microcirculation, resulting in a significant variation of the vascular pattern to which is associated a significant reduction of the burning sensation after three weeks of therapy. Such reduction of the burning sensation has been permanent for the 18 months following the acupuncture therapy. Acupuncture appears a valid therapeutic choice in the management of such patients.
Similar content being viewed by others
Introduction
Burning mouth syndrome (BMS) is a painful syndrome whose frequency in the general population is quite significant. According to recent studies, the syndrome affects 3.7% of the general population and is more common in women (5.5%) – particularly after menopause – than in men (1.6%).1
The disorder is characterised by a burning or itching sensation preferentially located at the tip and sides of the tongue, lips and anterior palate, in the absence of evidence of oral mucosal pathology, and sometimes associated with taste alterations and dry mouth.2 The syndrome is more common in women than in men, with the peak prevalence corresponding to females in the fourth to sixth decades of life. Several studies indicate that BMS is fairly common, which explains the increased attention that the condition has received in the recent literature.3
The aetiology of BMS is poorly understood and considered multifactorial, being associated with various local, systemic, psychogenic and neurological causes.4,5 Therapy is empiric and without evidence of efficacy, leaving the condition with no recognised treatment.6 The disorder, often of an unknown ethiopathogenesis, still presents substantial clinical, diagnostic and therapeutic problems. Due to the absence of a clear clinical objective assessment for this disorder and the lack of a definite understanding of its ethiopathogenesis, the clinical interpretation and treatment of BMS remains problematic. Among the possible risk factors of BMS are numerous physiopathological situations where the microcirculatory mechanisms are involved in pain generation. Recent research has revealed an alteration of the oral district microcirculation in patients with BMS.
The vasomodulatory effect of acupuncture has been proven through elegant thermographic methods that show how acupuncture is able to operate a microcirculatory modification. In addition, it has also been documented that the action of acupuncture on microcirculation is not carried out only at a cutaneous level but also in deeper areas.7,8 Examinations conducted through the spectroscopy and through fluxometry using laser Doppler has supplied evidence on how acupuncture can increase the speed of the blood flow and modulate the perfusion in the microcirculation. The aim of the study was to evaluate whether acupuncture can influence the oral microcirculation and consequently bring about a reduction of the symptoms of BMS.
Materials and methods
Sixty subjects were recruited for the study and were divided in two groups. The case group included 30 consecutive BMS patients (10 male and 20 female; age range 57-77 years, mean ± SD 65.4 ± 2.17) and the control group comprised 30 healthy subjects (10 male and 20 female; age range 52-70 years, mean ± SD 62.06 ± 6.72) (Table 1). All subjects were treated with acupuncture based on traditional Chinese medicine.9
The BMS diagnosis was made analysing the clinical history of the patient from a medical, pharmacological and dental point of view and attentively examining the mucosa. The diagnostic criteria included the absence of lesions in the oral mucosa and the exclusion of all the factors that can determine oral burning, such as the use of medicines such as anti-hypertensives etc, the presence of oral (Candida) or gastrointestinal infections (Helicobacter pylori), allergy to dental materials, metals or foods, incongruous prosthetic products, seric vitamin alteration or the presence of antibodies typical of autoimmune pathologies such as Sjögren's syndrome. All subjects recruited to the control group were free of oral lesions, systemic pathologies or pain sensation. They were taking no drugs that could influence oral microcirculation and were non-smokers.
All BMS patients responded to a specific questionnaire in which they reported on burning sensation. BMS patients numerically reported the burning sensation using a scale from 0 to 10 comparing the sensation to the burning feeling caused by the ingestion of red chilli peppers (capsaicin). After having signed the informed consent form allowing the researchers to proceed with the acupunctural technique, the videocapillaroscopic examination and the use of personal data, the patients were submitted to a complete study of labial and ventral surface of the tongue microcirculation under acupuncture. The study was conducted in three phases:
-
t0 – capillaroscopic study of the oral microcirculation in the absence of acupuncture (this represents the basis for comparison to record every definite variation of the microcirculatory system)
-
t1 – capillaroscopic study following the introduction of the needles in the pre-established points around 1 minute following the insertion and stimulation of the needles
-
t2 – capillaroscopic study after a second stimulation 5 minutes after the insertion of the needles.
For all BMS patients and healthy subjects we observed the mucosa of the lower lip (frenulum), where the vascular bed is easily visible owing to the considerable thinness of the mucosal lining and the ventral surface of the tongue. The control group was analysed in the same phases and under the same conditions as the BMS group to control for the effects of phases, position and breeze in the room. Acupuncture was administered on a monthly basis for six months.
Acupuncture
The acupuncture technique employed in the study is based on traditional Chinese medicine (TCM). Ten sterile, disposable, slender needles with a steel body and a copper head were applied through a guide tube. The dimensions of the chosen needles were 0.26 mm in diameter and 25 mm in length with a positioning time from 15 to 20 minutes. The acupuncture points stimulated were: SI 1 (small intestine – Shaoze) unilateral; TE 1 (triple riscaldatore – Guanchong) unilateral; LI 4 (large intestine – Hegu) unilateral; TE 21 (triple riscaldatore – Ermen) bilateral; ST 5 (stomach – Daying) bilateral; ST 6 (stomach – Jiache) bilateral; and CV 24 (Renmai chengjiang). The elicited response was of the type 'de qi' accompanied by redness and a feeling of numbness around the needles. The operator (FP) had a specific experience in the clinical application of acupuncture in the field of dentistry and particularly in the integrated therapy of temporomandibular dysfunctions and in atypical facial pain.10
Videocapillaroscopy
Oral videocapillaroscopy is a simple, repeatable, non-invasive, panoramic technique that is performed in vivo and is well-tolerated by the patient. This computerised technique is used with specific software (DS Medigroup, Milan, Italy) that allows the acquisition and the elaboration of the data. The videocapillaroscope is made up of a central unit, a fibre optic probe with video-optic terminal and a high resolution colour monitor. The lens has a focal spot of 1.811 mm and magnification which varies from 10 to 1,000×. For the study in question, a 200× magnification was used. The morphofunctional evaluation of microcirculation is based on specific parameters: length of the capillary loop, diameter of the loop, diameter of afferent and efferent loops, capillary tortuousness and density. The videocapillaroscopic investigation was always performed with the same light source, at the same room temperature (23°C), in the morning, with the same operator and repeated many times for every area under investigation.11
Statistical analysis
Statistical analysis was conducted using the Mann-Whitney U test. The significance level was set at p <0.05. The collected data was analysed with StatView 5.0.1 (SAS Institute Inc., Cary, NC). The acquired data refer to the mean values of the measurements for every pre-established parameter. The values of the phases of the study t0-t1, t0-t2, and t1-t2 were compared.
Results
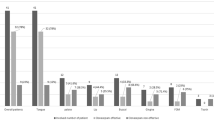
In all the cases and during all the phases of the study, the visibility of microcirculation during the capillaroscopic examination was clear and focusing simple and immediate (Fig. 1). The direction of the capillaries of the labial mucosa in the patients suffering from BMS was parallel to the surface where the probe was set during the examination and no variations in direction were recorded during all the phases of the study. The typical capillaroscopic picture in BMS is characterised by the presence of arborescent loops, dilation and a marked tortuousness. We focused our investigation on the mucosa of the lower lip and the mucosa of the tongue and the results are shown in Tables 2 and 3. The measurements were taken at the last administration of acupuncture. The statistical analysis was conducted comparing the mean values of the measurements and revealed significant values (p <0.05) for the following parameters in lower lip:
-
Increase in tortuousness comparing phases t0 (mean ± SD: 1.98 ± 0.017) to t1 (mean ± SD: 5.04 ± 0.044); p <0.05
-
Increase in tortuousness comparing phases t0 (mean ± SD: 1.98 ± 0.017) to t2 (mean ± SD: 3.9 ± 0.030); p <0.05
-
Increase in density comparing phases t0 (mean ± SD: 31.6 ± 1.30) to t1 (mean ± SD: 43.5 ± 1.73); p <0.05
-
Reduction of the number of arborescent loops (Figs 2, 3, 4).
Figure 2 Figure 3
Evaluation of burning sensation
At the beginning of the study, BMS patients reported a mean value of burning sensation of 8. After three weeks of acupuncture therapy, burning sensation values reported by BMS patients decrease to a mean of 2. After six months the burning sensation was at value 3. After 18 months the burning sensation reported had stabilised at the same value. Healthy subjects reported a mean burning sensation value of 0 in all the phases of the study.
The quality of life of the BMS patients after acupuncture therapy had evidently improved. These improvements are associated with the restoration of the microcirculation. The increase in tortuosity in BMS patients results in an improvement of perfusion and a decrease of the number of arborescent capillaries.
Discussion
Burning mouth syndrome (BMD) is a chronic, intraoral burning sensation occurring in the absence of identifiable oral lesions or laboratory abnormalities. Patients usually describe the sensation as a burning, tingling, or numbness of some part of the oral cavity, and often describe it as a feeling that the mouth has been burnt by hot tea or coffee. Among the possible risk factors for BMS are numerous physiopathological situations, where the circulatory mechanisms are involved in pain generation.12,13 A local circulatory disturbance of the areas affected by BMS could contribute to the burning sensations described by patients. Hechmann et al.14 investigated the mucosal blood flow in areas typically affected in patients with BMS. Their most interesting observations included relatively higher vasoreactivity following application of dry ice in patients with BMS compared to healthy individuals, and notably stronger reactions on the hard palate in BMS patients when compared to their control group. No significant differences were found in other examined areas, the vestibule and tongue. The stimulation with dry ice significantly altered the heart rate, and pCO2 was not different between the two groups. Therefore these parameters can be excluded as causes for the altered blood flow and consequently these changes seem to be linked to the symptoms of BMS, implying a disturbed vasoreactivity in patients with this disorder. Other authors described a lower tongue temperature in patients with BMS, which could also indicate alterations of the autonomic functions. Finally, other researchers found parafunctional habits in patients with BMS, such as teeth grinding and/or bruxism, or habitual pressing of the tongue against the teeth, which could lead to changes in the intra-oral blood flow.15,16 Summed up, these results seem to suggest that a disturbed regulation of the mucosal blood circulation plays a part in the symptomatology of BMS; in other words, it seems that BMS results from, or affects, the neurovascular microcirculatory unit (microcirculatory control of the sensory and autonomic innervation).
Studies on inflammatory disease point toward the presence of disturbance in the mucosal circulation, probably due to local inflammation.17,18 The vascular inflammation develops mainly in correspondence with the periphery of the blood microcirculation. This process can be described as a sequence of the following events: vascular modifications of the microcirculation, in particular variations in the vascular diameter and haematic flow; alterations of the blood-interstitial fluid exchange that leads to the formation of exudates; and migration of leukocytes from the blood vessels toward the interstitial space. These vascular modifications during vascular inflammation determine an active hyperaemia, which is caused by an increase in the blood flow in the capillaries and is evident in the typical symptoms of calor and rubor.
Scardina et al. in a capillaroscopic study on BMS patients, observed an increased total diameter of the capillary loops, as well as a dilatation of the afferent and efferent loop in patients with BMS. These alterations are compatible with the inflammatory picture.19
In our opinion, acupuncture lends itself to influencing microcirculation in patients with BMS, determining a smaller supply and passage of inflammatory products and therefore a remission of the symptomatological picture. From a point of view of traditional Chinese medicine, BMS has been evaluated only in a study that observed the millimeter wave therapy responses in patients with burning mouth syndrome. The results of this study demonstrated that the irradiation of holographic point by millimeter wave can improve the patients' pain, extravasated blood level and autonomic nerve system condition. It proposed acupuncture as a new treatment method for burning mouth syndrome.20
Several studies have demonstrated the vasomodulatory effect of acupuncture. Acupuncture stimulation and phototherapy have been reported to have analgesic effects and to improve the microcirculation. Komory et al. studied the vasomodulatory effect of acupuncture on rabbit arterioles under a dissecting microscope. The results of this study showed a significant increase in arteriolar diameter in the acupuncture group. Blood flow velocity and blood flow rate showed similar trends to arteriolar diameter. According to these results, acupuncture stimulation and phototherapy were directly confirmed to increase the diameter and blood flow velocity of the peripheral arterioles. Acupuncture stimulation and phototherapy, associated with minimal systemic and local side effects, can enhance the microcirculation and may be a useful treatment for diseases caused by poor peripheral blood flow.21
Hsiu et al. investigated the vasomodulatory effects of acupuncture stimulation on the microcirculation using spectral analysis with laser Doppler signal. Spectral analysis of the flux signal revealed that one of the major microcirculatory differences between acupoints and non-acupoints was in the different myogenic responses of their vascular beds. The results of these studies designate acupuncture as a non-invasive method to influence sympathetic control of peripheral vascular activity.22,23
Dong et al. studied effects of acupuncture and electro-acupuncture (EA) on blood perfusion in the stomach of rabbits, and the application of laser Doppler blood perfusion imaging (LDPI) in the study of the effect of acupuncture. The blood LDPI could clearly display changes of blood flow distribution in the stomach before and after acupuncture. Acupuncture and EA can increase blood perfusion in the stomach.24
In the odontostomatological field, acupuncture has proven to be effective in the therapy of oro-facial pain stemming from disorders of the trigeminal endings and has also shown a marked anaesthesiological capacity.25 Our research has therefore evaluated the oral microcirculation of patients with BMS under acupuncture. From the capillaroscopic point of view, the effects of the stimulation of specific acupuncture points appeared extemporaneously and evidently during the examination itself. From the symptomatological point of view, the first results were evident from the third session of acupuncture in which the patients declared a significant reduction of the pain and of the burning sensation. In the six months following the study, the results appeared unchanged and the symptoms were considerably attenuated with a monthly boost of therapy.
The in vivo observation of microcirculation revealed that by modification of the vascular pattern with a diminution of the arborescent loops and an increase of vascular density, acupuncture can result in a vascular pattern compatible to the physiology of microcirculation and a consequent reduction of BMS symptoms. The tendency, however, to return to a vascular pattern which is characteristic for these patients makes it essential to undergo monthly sessions of acupuncture with the aim of restoring the normal circulatory microparameters. Such results are clearly significant but need to be re-evaluated over time with the aim of understanding whether such encouraging effects are caused by the strong psychological impact of the technique, therefore having only a temporary effect, or by a vasostabilising effect that would result in a reduction of the pro-inflammatory metabolites and would interrupt the negative loop which is at the base of the chronic process of the illness.
Conclusion
The study shows that acupuncture influences oral microcirculation, determining a significant variation of the vascular pattern to which is associated a significant reduction of burning sensation after three weeks of therapy. Such reduction of the burning sensation has been permanent for the 18 months following the acupuncture therapy. Acupuncture appears, in light of these data, a valid therapeutic choice in the management of BMS patients.
References
Bergdahl M, Bergdahl J . Burning mouth syndrome: prevalence and associated factors. J Oral Pathol Med 1999; 28: 350–354.
Brufau-Redondo C, Martín-Brufau R, Corbalán-Velez R, de Concepción-Salesa A. Burning mouth syndrome. Actas Dermosifiliogr 2008; 99: 431–440.
Palacios Sanchez M F, Jordana Comin X, Garcia Sivoli C E . Sindrome de boca ardiente: Estudio retrospectivo de 140 casos en una muestra de la poblacion catalana. Med Oral Patol Oral Cir Bucal 2005; 10: 388–393.
Maltsman-Tseikhin A, Moricca P, Niv D . Burning mouth syndrome: will better understanding yield better management? Pain Pract 2007; 7: 151–162.
Scardina G A, Ruggieri A, Messina P . Neurologic inflammation and oral disease. An aetiopathogenic hypothesis. Recenti Prog Med 2007; 98: 653–658.
Mínguez Serra M P, Salort Llorca C, Silvestre Donat F J . Pharmacological treatment of burning mouth syndrome: a review and update. Med Oral Patol Oral Cir Bucal 2007; 12: 299–304.
Cui S Y, Tang C Z . Progress in the research of neuroendocrine-immunological mechanism of acupuncture in regulating blood pressure and protecting target organs in hypertension. Zhen Ci Yan Jiu 2008; 33: 208–212.
Litscher G. Bioengineering assessment of acupuncture, part 2: monitoring of microcirculation. Crit Rev Biomed Eng 2006; 34: 273–294.
Scardina G A, Ruggieri A, Provenzano F, Messina P . The effect of acupuncture on oral microcirculation in healthy volunteers: an exploratory study. Acupunct Med 2009; 27: 114–117.
Prady S L, Macpherson H . Assessing the utility of the standards for reporting trials of acupuncture (STRICTA): a survey of authors. J Altern Complement Med 2007; 13: 939–943.
Scardina G A, Ruggieri A, Messina P . Oral microcirculation observed in vivo by videocapillaroscopy: a review. J Oral Sci 2009; 51: 1–10.
Scardina G A, Pisano T, Messina P . Burning mouth syndrome. Recenti Prog Med 2007; 98: 120–128.
Lauria G, Majorana A, Borgna M et al. Trigeminal small-fiber sensory neuropathy causes burning mouth syndrome. Pain 2005; 115: 332–337.
Heckmann S M, Haeckmann J G, Hilz M J et al. Oral mucosal blood in patients with burning mouth syndrome. Pain 2001; 90: 281–286.
Chimenos-Kustner E, Marques-Soares M S. Burning mouth and saliva. Medicina Oral 2002; 7: 244–253.
Femiano F, Gombos F, Scully S . Burning mouth syndrome: the efficacy on subgroups. J Eur Acad Dermatol Venereol 2004; 18: 676–678.
Scardina G A, Messina P . Microvascular periodontal alterations: a possible relationship between periodontitis and rheumatoid arthritis. Clin Haemorheol Microcirc 2007; 37: 229–235.
Scardina G A, Picone V, Cacioppo A, Messina P . Study of microcirculation in oral lichen planus by video-capillaroscopy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: e30–e34.
Scardina G A, Pisano T, Carini F, Valenza V, Messina P . Burning mouth syndrome: an evaluation of in vivo microcirculation. J Am Dent Assoc 2008; 139: 940–946.
He Y, Lin M, Li B Q, Xia J, Zeng G M . Effect of millimeter therapy in burning mouth syndrome. Zhonghua Kou Qiang Yi Xue Za Zhi 2003; 38: 89–92.
Komori M, Takada K, Tomizawa Y et al. Microcirculatory responses to acupuncture stimulation and phototherapy. Anesth Analg 2009; 108: 635–640.
Hsiu H, Huang S M, Chao P T . Study on the microcirculatory blood velocity of acupoint monitored by laser Doppler signal. Conf Proc IEEE Eng Med Biol Soc 2007; 2007: 959–962.
Hsiu H, Huang S M, Chao P T . Microcirculatory characteristics of acupuncture points obtained by laser Doppler flowmetry. Physiol Meas 2007; 28: N77–N86.
Dong Z, Shun-Yue L, Shu-You W, Hui-Min M. Evaluation of influence of acupuncture and electro-acupuncture for blood perfusion of stomach by laser Doppler blood perfusion imaging. Evid Based Complement Alternat Med 2009 Jun 16; 10.1093/ecam/nep050 [Epub ahead of print].
Goddard G. Short term pain reduction with acupuncture treatment for chronic orofacial pain patients. Med Sci Monit 2005; 11: 71–74.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Scardina, G., Ruggieri, A., Provenzano, F. et al. Burning mouth syndrome: is acupuncture a therapeutic possibility?. Br Dent J 209, E2 (2010). https://doi.org/10.1038/sj.bdj.2010.582
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2010.582
This article is cited by
-
Complementary treatments and dental indemnity
BDJ In Practice (2020)
-
Management of Pain Associated with Selected Conditions in Dermatology
American Journal of Clinical Dermatology (2016)
-
Burning Mouth Syndrome: A Review of Recent Literature
Current Pain and Headache Reports (2013)