Key Points
-
Highlights the difficulties in undertaking research in prisons.
-
Screening prisoners for dental conditions in 'high turnover' prisons is not effective.
-
Details the reasons why prisoners are a high need, difficult to engage population.
Abstract
Objective To compare the performance of a questionnaire-based assessment of dental pain delivered by non-dental prison nursing staff against a clinical examination performed by an experienced prison dentist (gold standard).
Setting The research fieldwork took place in the healthcare department at HMP Brixton located in South London.
Methods The cohort were those who had complained of dental/facial pain to the prison authorities and were therefore placed on the waiting list for emergency dental care. Subjects were asked to complete the screening test and were then clinically examined by trained and calibrated dentists. The screening test was in the form of a 12-item questionnaire designed to categorise a population reporting dental pain into one of three groups. The screening test results were compared with the diagnosis of a clinical examination.
Results Ninety-six subjects were recruited during the 16-week study period. Of the 96 prisoners recruited, 27 of those failed to complete the screening test and/or the diagnostic examination even though they had reported pain previously. When sensitivity and specificity values were calculated for the 96 prisoners recruited, the sensitivity was fairly high (81%) and the specificity was poor (33%). However, when these values were calculated for the sub–population, those that completed both the screening test and diagnostic examination (n = 69), the sensitivity did not improve particularly (83%) but the specificity value fell substantially to 13%.
Conclusions This study highlighted the problems of conducting research in the prison environment, for example increased security preventing researchers from gaining access into the prison and general pressures on prison staff. Additionally, the study demonstrated that screening is not effective in local prisons with a high turnover of prisoners.
Similar content being viewed by others
Introduction
In 2003 the responsibility for funding prison health services in England was transferred from the Home Office to the Department of Health. This was the first step in a process of integrating prison health services into the mainstream National Health Service (NHS). To support this process, in April 2006 primary care trusts (local NHS bodies) were given responsibility for commissioning prison health services and are now expected to ensure that prison health care is equivalent to mainstream NHS services.1,2
Many prison dental services are overstretched and this service is a significant concern for PCTs and providers of prison healthcare. Prisoners have high levels of untreated dental disease3,4,5,6 and extensive oral neglect is common in newly admitted prisoners.2 Due to the extensive and unpredictable mobility of remand and short stay prisoners and the restricted provision of dental services in prisons, patients with toothache can experience difficulties in gaining rapid access to dental care.1 One possible solution to this problem is to screen new prisoners on entry to the prison for urgent dental treatment needs and provide fast track access to dental services for those screened positive. There are 24 and 48 hour general health checks for newly admitted prisoners performed by a nurse but there is no standardised dental component to these assessments.
A simple-to-complete questionnaire (Dental Pain Questionnaire (DePaQ)) has been developed and tested in the NHS.7 This screening instrument classifies patients with dental pain into three groups of common dental pain conditions:
-
Group 1 (acute periapical periodontitis and irreversible pulpitis)
-
Group 2 (reversible pulpitis and dentine hypersensitivity)
-
Group 3 (pericoronitis).
In a population attending an NHS dental teaching hospital, the DePaQ was capable of correctly classifying 89.7% of dental pain cases initially categorised by clinical diagnoses. The respective sensitivity and specificity values of the questionnaire were Group 1: 0.80, 0.83, Group 2: 0.85, 0.89, and Group 3: 0.59, 0.90. If this tool can perform to a similar level in a prison population it has the potential to rapidly identify prisoners reporting pain who have an urgent treatment need without the need for all prisoners to see a dentist. This possibility could improve the lives of prisoners and help PCT and prison healthcare mangers plan dental service resources more efficiently.
The aim of this study was to assess the performance of the DePaQ in identifying prisoners with an urgent need for dental care when compared against clinical diagnoses.
Methods
The study population was composed of male prisoners providing informed consent on the urgent treatment list of HMP Brixton in London. All of these prisoners had complained of toothache to the prison authorities previously and were listed to have rapid access to the dental service in prison, which provided dedicated sessions to see prisoners complaining of pain. The prisoners were invited to participate by a trained member of the healthcare team when they arrived at the dental department. HMP Brixton serves a number of courts in the London conurbation and houses a mixture of male remand and sentenced prisoners.8 This prison houses up to 798 prisoners at any one time, with an a high turnover of prisoners, many staying just 35 days on average.9
Ethical approval was granted by South Essex Local Research Ethics Committee. Prisoners are considered a vulnerable group. The NHS ethical review process is in place to protect research participants and the researchers. The conduct of the study ensured that prisoners were neither coerced nor offered any incentive to participate.
The screening test was in the form of a 12-item questionnaire designed to categorise a population reporting dental pain into three groups:
-
1
Irreversible pulpitis and acute periapical periodontitis (dental abscess)
-
2
Reversible pulpitis and dentine hypersensitivity
-
3
Pericoronitis (inflammation connected to a partially erupted tooth, classically a wisdom tooth).
Those subjects that had no pain, or the questionnaire was incomplete or they did not complete a clinical examination, were classified into a separate group (group 4). Subjects categorised into groups 1 (irreversible pulpitis, acute periapical periodontitis) and 3 (pericoronitis) were adjudged to have an urgent need of treatment, while those in the group 2 and group 4 were defined as having non-urgent treatment need.
Due to the high levels of literacy problems among prisoners,10 the questionnaire was read out to prisoners by the nurse who normally undertakes the 48 hour general assessment of new prisoners. The language used to introduce the questionnaire and used in the questionnaire itself was piloted with nursing staff and prisoners in HMP Brixton. The prison nurse recorded the prisoner's response to each question on the questionnaire, which took approximately five minutes to complete.
The diagnostic test consisted of a history and clinical examination defined by a diagnostic protocol. Two experienced prison dentists were trained in the diagnostic protocol and performed the diagnostic examinations blind to the outcomes of the questionnaire screening test. A training exercise was carried out in which two of the authors (LZ & AP) agreed the examination protocol and diagnostic criteria for the common dental pain conditions using case scenarios in a classroom context. This was followed by a calibration exercise in which 25 patients were examined and diagnosed prior to the start of the study and there was 100% agreement between the dentists. The outcome of each diagnostic examination was recorded on a simple clinical data collection form. The dentists categorised the study population into the same clinical groupings as the screening test.
Analysis included simple frequency distributions and cross tabulations. Responses to the questionnaire were entered into classification equations from a previous study using a dental hospital setting. Using these classification equations, each prisoner was assigned to one of the three groups of clinical conditions and then recategorised into urgent or non-urgent groups. Cross-tabulations between questionnaire classification and clinical diagnosis were carried out to compute sensitivity and specificity values for:
-
The whole population, that was all individuals consented into the study
-
A subpopulation, which comprised all subjects who completed each stage of the testing process, that is consent, screening questionnaire and diagnostic examination.
Results
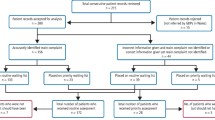
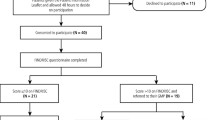
In total 96 subjects were recruited and consented. Figure 1 presents a flow diagram summarising the number of subjects at each stage of the fieldwork. Five subjects admitted that they had no pain prior to administering the screening questionnaire, even though they had reported that they were suffering toothache within the previous 24 hours. A further seven subjects could not complete the questionnaire even though a nurse was reading the questions to them and filling in the questionnaire on their behalf. Following completion of the screening test, 15 subjects admitted that they had not been experiencing pain once they had access to the examining dentists. They then made requests for other forms of non-urgent dental treatment. This left 69 patients who had reported pain over the last 24 hours and completed both a screening test and diagnostic examination.
Table 1 shows the distribution of subjects screened positive and diagnosed positive according to the clinical categories. Irreversible pulpitis or periapical periodontitis were most commonly screened positive and diagnosed, whereas periocoronitis was rarely screened or diagnosed. There were large discrepancies between the outcomes of the screening and diagnostic tests in the categories irreversible pulpitis or acute periapical periodontitis and dentine hypersensitivity or reversible pulpitis. These differences were evident in the sensitivity and specificity values of the screening test.
Table 2 compares the outcome of the screening test with the outcomes of the diagnostic test for the whole population. Approximately three quarters of the population was screened positive. Sensitivity was relatively high (81%) but specificity was poor (33%), with large numbers of subjects wrongly identified to the screening test as having an urgent treatment need. When the sub-population that excluded individuals who failed to complete a questionnaire or admitted to falsely reporting dental pain was examined, there was little improvement in performance of the test. Sensitivity increased marginally (85%) but specificity fell substantially to 13% (Table 3), with large numbers of false positives being detected.
Discussion
The fieldwork of this study illustrated some of the difficulties in conducting research in a prison environment. The research was initially scheduled to take place in two prisons, Brixton and Belmarsh. However, before the fieldwork could begin, security in Belmarsh was significantly tightened and fieldwork in this prison had to be abandoned as security clearance for fieldworkers could not be obtained. Staff at Brixton were confident that they could recruit sufficient subjects to complete the project within the planned timescales. We planned to recruit 200 subjects over a six week period. It transpired that we recruited 96 subjects after four months. The fieldwork of the project was stopped as the prison could not recruit the necessary adequately trained staff with the correct security clearance to go into the prison and escort prisoners to the healthcare facility for enrolment onto the project.
Additional problems were encountered, such as prison officers unilaterally deciding to stop a research session due to security concerns, and failure of prisoners to attend recruitment sessions. This latter difficultly was surprising as all prisoners scheduled for these visits had complained of toothache. Prison staff reported that some prisoners were reluctant to attend the healthcare facility due to fears about being attacked during transfers, and that other prisoners failed to attend because they did not feel like attending the dental surgery that day. However, the principal problem hindering and ultimately preventing completion of the planned fieldwork was intermittent staffing problems in the prison throughout the whole of the study period. This problem was not due to lack of funding but due to the shortage of individuals with the necessary training and experience to supervise the transfer of prisoners from the prison to the healthcare facility. There is no consensus in the literature on required sample sizes for psychometric validation of screening tests11,12,13 and although we fell short of our target recruitment for the study, the study provided interesting data.
The problems encountered during the study period are problems that are often encountered daily in many healthcare departments across prisons in England. All of the issues mentioned above cause difficulties in the day to day running of healthcare departments and ultimately hinder the smooth delivery of healthcare services to this high need population.
Analysis of the whole population (n = 96) showed that the test had good sensitivity but poor specificity. Having high sensitivity means that the instrument was able to identify correctly a high proportion of those prisoners who were screened as needing urgent treatment. Therefore the instrument would have some value if we are interested to ensure that those with urgent need are identified in the screening process. A low specificity means that those subjects identified as not needing urgent treatment were classified by the questionnaire as needing urgent treatment. The implication of this is that it may lead to inappropriate scheduling of appointments for prisoners needing dental care.
Seven subjects were unable to complete the questionnaire even though the questions were read out to all participants and the responses recorded on their behalf by a nurse. This may have been due to the failure to comply completely with the process because subjects were not experiencing pain but wanted access to the dentist for other reasons. This problem was illustrated by the fact that 19 subjects said they had pain, but then at the screening test (n = 4) or prior to the diagnostic examination (n = 15) admitted they were not experiencing pain but wanted access to the dentist to ask for some other form of treatment, usually of a cosmetic nature, for example a scale and polish or a crown.
When the 27 subjects who confessed to not having pain or could not complete the questionnaire were excluded from the analysis, the specificity remained high but the sensitivity dropped to 13%. This could be attributed to subjects 'gaming' the screening test, providing untruthful answers to again ensure that they gained access to the dentist. For example, some of the questions in the screening test were related to duration of pain. Many subjects reported that they experienced pain over long periods, perhaps to misleadingly convey the impression that they needed urgent access to a dentist. This lay perception of the clinical presentation of dental pain is at odds with the actual presentation of irreversible pulpitis or dental abscess. This pain is very severe but comparatively short lasting, therefore the screening test would tend to categorise subjects reporting that pain had been present for a long period as having non-urgent treatment needs. Another interpretation of the findings could be that the prisoners tended, in the questionnaire, to overestimate the severity of their pain in order perhaps to obtain rapid care, rather than necessarily offering untruthful answers. This inaccuracy in pain self-reporting has been observed by others.14,15 Also, it could be that the examining dentists underestimated the severity of the prisoners' pain experience or underestimated the prisoners' inability to cope and therefore assessed them as not needing urgent treatment.
Assessing the performance of a screening test is complicated in this population by difficulties of making an accurate diagnosis. Untreated dental disease is almost ubiquitous in UK prison populations16,17,18 and correct diagnosis of the cause of dental pain requires the taking of an adequate history. The high prevalence of untreated dental disease and some subjects providing misleading histories would hamper accurate diagnosis. Provision of disingenuous answers to the screening test and uncertainty of diagnosis are likely to lead to haphazard outcomes, resulting in some false negative and some false positive results. The low literacy levels10 may compound the haphazard nature of the outcomes of screening and diagnostic tests in this population.
Although the screening tool demonstrated excellent results in a population attending an NHS dental teaching hospital,7 it performed poorly in the prison setting. Prior to undertaking this study, many experienced dentists working in the prison service warned the research team that prisoners would be untruthful and claim that they were in pain just to have time outside their cell or gain access to the dentist. This study quantifies this issue and strongly suggests that screening is inappropriate for a local prison with a high turnover population. It should be remembered that screening is a process that includes screening, referral, diagnosis and provision of appropriate treatment, and the screening test is usually the easiest part of the process to get right. Even if a screening test produced high levels of sensitivity and specificity, screening could easily fail at other points in the process due to a highly mobile population and the part-time nature of prison dental services.
Screening may work in a less mobile, long-stay, convicted population of prisoners. This study shows that the questionnaire is of little help in providing efficient access to care for newly admitted individuals with acute dental pain in high turnover local prisons. The National Screening Committee (NSC)19 acknowledges that screening is not the answer to certain problems and that before a screening programme is introduced, 'all other options for managing the condition should have been considered (eg improving treatment, providing other services), to ensure that no more cost effective intervention could be introduced.' For this population of newly admitted short-stay and remand prisoners, it may be more appropriate to provide a clearly defined symptomatic, pain relief-only service in line with the guidance by the Department of Health.1 However, prison healthcare managers must accept there will always be inefficiencies in providing services to this difficult but high need population and plan accordingly. It is nevertheless important that we continue to work to find a workable solution for this difficult to engage, high need population.
This study has highlighted the problems of conducting research in the prison environment. There are a number of reasons for difficulties encountered, for example, increased security preventing researchers from gaining access into the prison and general everyday pressures on prison staff due to the shortage of staff. Additionally, the study demonstrated that screening is not effective in local prisons with a high turnover of prisoners.
References
Department of Health, HM Prison Service. Strategy for modernising dental services for prisoners in England. London: Department of Health, 2003.
Harvey S, Anderson B, Cantore S et al. Reforming prison dental services in England – a guide to good practice. Health Educ J 2005; 64(Suppl. 4): ii–iii, 1–39.
Lunn H, Morris J, Jacob A, Grummitt C . The oral health of a group of prison inmates. Dent Update 2003; 30: 135–138.
Naidoo S, Yengopal V, Cohen B . A baseline survey: oral health status of prisoners – Western Cape. SADJ 2005; 60: 24–27.
Osborn M, Butler T, Barnard P D . Oral health status of prison inmates – New South Wales, Australia. Aust Dent J 2003; 48: 34–38.
Jones C M, Woods K, Neville J, Whittle J G . Dental health of prisoners in the north west of England in 2000: literature review and dental health survey results. Community Dent Health 2005; 22: 113–117.
Pau A, Croucher R, Marcenes W, Leung T . Development and validation of a dental pain-screening questionnaire. Pain 2005; 119: 75–81.
HM Prison Service website. Brixton webpage. http://www.hmprisonservice.gov.uk/ prisoninformation/locateaprison/prison.asp?id=284,15,2,15,284,0 (accessed 8 October 2008).
Heidari E, Dickinson C, Wilson R, Fiske J . Oral health of remand prisoners in HMP Brixton, London. Br Dent J 2007; 202: E5.
The Home Office. Freedom of information release: literacy and numeracy levels of prisoners. 25 January 2005. Available at http://www.homeoffice.gov.uk/about-us/ freedom-of-information/released-information/foi-archive-offender-management/200-literacy-numeracy-prisoners?view=Html (accessed 8 October 2008).
Hapak L, Gordon A, Locker D, Shandling M, Mock D, Tenenbaum H C . Differentiation between musculoligamentous, dentoalveolar, and neurologically based craniofacial pain with a diagnostic questionnaire. J Orofac Pain 1994; 8: 357–368.
Galer B S, Jensen M P . Development and preliminary validation of a pain measure specific to neuropathic pain: the Neuropathic Pain Scale. Neurology 1997; 48: 332–338.
Thomas R J, McEwen J, Asbury A J . The Glasgow Pain Questionnaire: a new generic measure of pain; development and testing. Int J Epidemiol 1996; 25: 1060–1067.
Kikuchi H, Yoshiuchi K, Miyasaka N et al. Reliability of recalled self-report on headache intensity: investigation using ecological momentary assessment technique. Cephalagia 2006; 26: 1335–1343.
Broderick J E, Schwartz J E, Vikingstad G, Pribbernow M, Grossman S, Stone A A . The accuracy of pain and fatigue items across different reporting periods. Pain 2008; 139: 146–157.
Bolin K, Jones D . Oral health needs of adolescents in a juvenile detention facility. J Adolesc Health 2006; 38: 755–757.
Young D S . Health status and service use among incarcerated women. Fam Community Health 1998; 21: 16–31.
Walsh T, Tickle M, Buchanan K, Milsom K, Zoitopoulos L . An investigation of the nature and quality of research into dental health in prisons: A systematic review. Br Dent J 2008; 204: 683–689.
UK National Screening Committee. Criteria for appraising the viability, effectiveness and appropriateness of a screening programme. National Screening Committee, 2003. Available at http://www.nsc.nhs.uk/pdfs/criteria.pdf
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Buchanan, K., Milsom, K., Zoitopoulos, L. et al. The performance of a screening test for urgent dental treatment need in a prison population. Br Dent J 205, E19 (2008). https://doi.org/10.1038/sj.bdj.2008.950
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2008.950
This article is cited by
-
Summary of: The performance of a screening test for urgent dental treatment need in a prison population
British Dental Journal (2008)