Abstract
Measures of clinical incidence are necessary to help estimate the burden of a disease. Incidence is a metric not commonly measured in malariology because the longitudinal surveys required are costly and labour intensive. This database is an effort to collate published incidence records obtained using active case detection for Plasmodium falciparum and Plasmodium vivax malaria. The literature search methods, data abstraction procedures and data processing procedures are described here. A total of 1,680 spatio-temporally unique incidence records were collected for the database: 1,187 for P. falciparum and 493 for P. vivax. These data were gathered to model the relationship between clinical incidence and prevalence of infection and can be used for a variety of modelling exercises including the assessment of change in disease burden in relation to age and control interventions. The subset of data that have been used for such modelling exercises are described and identified.
Design Type(s) | observation design • epidemiological study • data integration objective |
Measurement Type(s) | infectious disease incidence |
Technology Type(s) | Epidemiology |
Factor Type(s) | |
Sample Characteristic(s) | Plasmodium falciparum • Plasmodium vivax • anthropogenic habitat |
Machine-accessible metadata file describing the reported data (ISA-Tab format)
Similar content being viewed by others
Background & Summary
The global clinical burden of malaria has proven difficult to enumerate. Previous efforts have estimated the clinical incidence of Plasmodium falciparum malaria using adjusted case reports1,2, modelling based on study-level incidence and mortality rates3 and cartographic modelling techniques4–6. All of these methods require malaria incidence measures in some part of their estimation or validation procedures. The surveillance-based approach relies on routinely reported case numbers, which are adjusted by country to account for incomplete reporting, the proportion of cases confirmed with routine diagnostics, and health facility use and access1. The Global Burden of Disease (GBD) study uses an amalgam of three methods to estimate case incidence. First, reported cases are used from a small subset of countries deemed to have reliable reporting. Second, corrected reporting (similar to the surveillance-based approach methods) is applied to a larger set of countries. And third, study-level incidence, such as the records reported here, along with mortality rates and a variety of parameters such as age and detection methods are used to model country-level incidence3. The cartographic approach, employed by the Malaria Atlas Project (MAP), also uses a tiered approach. Case estimates from countries with reliable estimate are used directly. Regions designated as unstable transmission regions6,7 are assigned an incidence of 0.1 cases per 1,000 per year. For regions without accurate reporting in areas stable malaria transmission, a modelled relationship between study-level measures of incidence matched in space and time to prevalence surveys is applied to a smooth endemicity (prevalence) surface7 and multiplied by a global population grid4. Such matched incidence and prevalence data are presented here.
Whilst approximations of ‘non-P. falciparum’ malaria exist, the burden of Plasmodium vivax malaria is considered to be largely unknown8–10. The primary reason for these knowledge gaps is that measures of malaria incidence are rarely undertaken as they are logistically demanding and thus expensive. To accurately measure clinical incidence of malaria, longitudinal studies must be conducted that include regular visits made to communities to check for symptomatic individuals through active case detection (ACD)11. The database described here aimed to compile as many ACD studies for P. falciparum and P. vivax as possible from 1985 to 2013 and represents a significant expansion upon previously published assemblies of incidence data5.
A more commonly measured malaria metric is prevalence, also known as parasite rate (PR)12. As demonstrated by Patil et al.5, Cameron et al.13 and Battle et al.14, ACD incidence records can be matched to PR measures to model the relationship between prevalence of infection and incidence of clinical disease. These models then have the potential to transform existing endemicity maps7,15 into global burden estimates with known precision5. For this purpose, each ACD observation in this database has been matched to a concurrently measured PR value or an extracted spatially and temporally matched modelled PR7,15.
All data curation and abstraction procedures to obtain the 1,680 incidence records, including geo-positioning and prevalence matching, are described here. The structure of the final database and technical validation efforts are also described along with notes to facilitate the replication of the analyses in Cameron et al.13 and Battle et al.14 Such validation yields a powerful mathematical tool supporting efforts to reliably estimate global burdens of disease imposed by the parasites causing human malaria.
Methods
Data collection
Here we provide additional detail on methodology to that provided in Cameron et al.13 and Battle et al.14, which utilize only a subset of the data presented here. PubMed (http://www.ncbi.nlm.nih.gov/pubmed) was searched on 27 November 2013 using the following search string: ((malaria[MeSH Terms]) AND (‘Incidence’ [Mesh] OR ‘Epidemiology’ [Mesh] OR ‘epidemiology’ [Subheading])) AND (‘1985/01/01’[Date—Publication]: ‘3000’[Date—Publication]). This selected references published after 1 January 1985 and the Medical Subject Headings (MeSH; http://www.ncbi.nlm.nih.gov/mesh) ensured that all pseudonyms were included in the search. The cut off of 1985 was used to match the year range of PR records included in the MAP database16. The literature search returned 11,272 citations and was augmented with a further 25 references from previously published analyses5,17. A total of 15 search strings were tested varying the terms used and application of MeSH terms. The number of references returned ranged from 58 (((malaria[MeSH Terms]) AND ‘active case detection’) AND (‘1985/01/01’[Date—Publication]: ‘3000’[Date—Publication])) to 1,291,787 (((((malaria[MeSH Terms]) AND incidence[MeSH Terms]) OR epidemiology[MeSH Terms]) OR epidemiology[MeSH Subheading]) AND (‘1985/01/01’[Date—Publication]: ‘3000’[Date—Publication])). The search string used was chosen because it was a reasonable number of titles for a small team to sort through, while still capturing the majority (87%, 55/63) of the references used in a previously published collection5.
Abstracts were reviewed to determine if the reference might contain P. falciparum or P. vivax incidence data. References excluded at this stage included reviews, case studies, vector-only, reports on animal or non-P. falciparum or P. vivax malaria, reports of imported malaria and technical articles including mathematical modelling and genetic analyses. The full list of 11,297 references was narrowed down to 898 references for full text review. Seventy-eight references known to contain incidence data from the work by Patil et al.5 and Griffin et al.17 were also set aside.
Full texts were obtained for the 976 references identified for review. The criteria for inclusion were: (i) longitudinal studies using ACD, (ii) symptomatic/clinical cases were the subjects of detection, (iii) studies were conducted in the general community (not patient sub-groups or hospital-based studies), and (iv) diagnosis using microscopy or rapid diagnostic test (RDT). Studies done only on pregnant women were excluded due to their increased susceptibility to malaria18. Conversely, studies using only infants aged less than three months were excluded due to their potential temporary immunity to P. falciparum from maternal antibodies19. Plasmodium vivax has been shown to cause significant morbidity in young infants20,21, however none of the studies conducted on infants measured P. vivax incidence. In-house language skills only allowed for the inclusion of articles written in English, French, Portuguese and Spanish. Twelve publications out of the 976 identified for review were in other languages (one Turkish and 11 Chinese) and therefore excluded. Articles that did not have enough information to determine the number of cases and the person-time observed (length of follow up for each cohort member) were excluded. Initially, there were no restrictions placed on the length or frequency of follow up, as long as it was explicitly reported. Based on the above criteria, data were abstracted from a total of 230 references, the majority of which measured incidence of P. falciparum malaria. Data on P. falciparum and P. vivax incidence were identified in 226 and 99 of these references, respectively. Literature review procedures are outlined in Fig. 1.
Geo-positioning
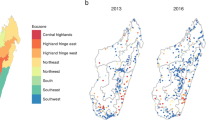
All available location information was extracted from the published sources. Incidence records were first positioned to a MAP region: Africa+ (Africa plus Saudi Arabia and Yemen), the Americas, and Central and Southeast Asia (CSE Asia). The number of records by species and region are shown in Table 1. Next, they were assigned to a country (based on 2013 boundaries) and place. The place was considered the location of the study and latitude and longitude coordinates for each site were found using values given in the paper (converting to decimal degrees where necessary) or where this was unavailable, manually digitized using Google Maps22 or Microsoft Encarta23. Contextual information from the paper was used to differentiate when two places with the same name were within one country or to narrow down a region to be scanned for names that could be different spellings or translations of the site name (for example, Sissé rather than Cisse). If the site was a village, town or city, the latitude and longitude were taken from centre, unless a specific part of the town or city were specified as the study site. If the only location information given was a larger area such as a district administrative unit, as defined by the Food and Agriculture Organization (FAO) Global Administrative Unit Layers (GAUL) coding24, the centroid of the region was found using geographic information systems (GIS) software25. If the location could not be determined by any of these means, the authors were contacted for further information. The locations of each record are shown in Fig. 2 and the distribution of the data records over time are shown by country in Fig. 3. Records were also matched to zoo-epidemiological zones originally defined by Macdonald26 and modified by Battle et al.27 to describe the geographic variation observed in P. vivax relapse phenotypes (Fig. 4). These classifications enable the relationship between prevalence and incidence to be modelled separately by region.
The geographic locations of the incidence records for P. falciparum (top panel) and P. vivax (bottom panel) are shown over the model-based geostatistics (MBG) point estimates of the annual mean PfPR2-10 and PvPR1-99 for 2010 within the spatial limits of stable limits of transmission (annual parasite index (API) ≥0.1 per 1,000 per annum (p.a.)), displayed on a continuum from blue (0% PR) to red (70% PR for P. falciparum and >7% PR for P. vivax). Dark grey areas were predicted to be unstable (API ≤0.1 per 1,000 p.a.) and light grey areas were classified as risk free. Areas in which Duffy negative allele frequency is predicted to exceed 90% (ref. 29) are shown in hatching for additional context in the P. vivax map. Study sites used in the P. falciparum (Cameron et al.13) and P. vivax (Battle et al.14) models are shown as yellow stars and other sites included in this dataset not used in the cited analyses are shown as purple points.
Plasmodium falciparum (left panel) and P. vivax (right panel) records are shown as points along an axis of the study start year. The points vary in colour and size based on the number of person-years observed in each study, such that studies with smaller sample sizes are small dark purple points and larger studies are large light blue points. The points are jittered so that overlapping points can be seen.
Calculating incidence
Incidence describes the number of events that occur within a specified time period. In this context, the events are symptomatic cases (fever cases confirmed by RDT or microscopy) of P. falciparum or P. vivax identified within a study population. Cases of P. vivax may arise from new mosquito-borne infections, recrudescence from treatment failure or relapses from hypnozoites (the dormant liver stage). Because there is no reliable way to differentiate relapses from new infections or recrudescence, the incidence of P. vivax reported here includes the cases from all origins.
Values for the number of cases and time period the study population was observed (recorded in person-years) were needed for modelling purposes and every effort was therefore made to extract or derive those values. If incidence was given, then the number of cases or person-time was derived from other information provided in the publication. In the few studies that provided age-specific data without age-specific population data, a general population structure was applied28 to the whole population to determine the size of the composite age groups. Where person-time was not explicitly reported, this was calculated by multiplying the population number by the length of the study period. This was necessary for the majority of studies for both P. falciparum (61%, 722/1187) and P. vivax (77%, 378/493).
Matching prevalence to incidence
So that the data may be used to model the relationship between prevalence (PR) and incidence of clinical disease, an estimate of prevalence was spatially and temporally matched to each incidence record in the database. If the incidence publication source contained empirical prevalence data, this was abstracted to provide a space-time match between PR and incidence. Averages were taken for those studies that reported more than one cross-sectional survey (XSS) for the same community. The number and timing of each survey was recorded where available. Half of the records had PR data available from the same reference (840/1680). Some additional space-time prevalence matches were added using the MAP PR database16 if a separate publication measured PR in the same community and year as the incidence data (6%, 97/1680). For the remaining 44% of the data (743/1680) without concurrent prevalence data, PR values were extracted for all incidence records using 2010 point estimates of the annual mean modelled P. falciparum7 and P. vivax15 endemicity values (shown in Fig. 1) using GIS software25. For P. vivax, areas where Duffy negative allele frequency was predicted to exceed 90% (ref. 29) is shown in hatching and P. vivax PR was predicted at <1% in those areas. The PR values for P. falciparum were predicted for two to ten year-olds, whereas for P. vivax, the predictions were made for all ages (one to 99 years). Because these age ranges did not always correspond to age groups in the incidence data, these data were age standardized using a bespoke model parameterized for P. falciparum30 and P. vivax15. The age standardization model was also applied as needed to PR values obtained from publications, as not all prevalence records had matching age ranges to the incidence data. The number of parasite positive individuals was then adjusted to match the age-standardized prevalence value. See results in Data Citation 1. A schematic illustration the process of matching prevalence and incidence data is shown in Fig. 5.
Code availability
All age standardisation routines were implemented in an open-source software package ageStand31, implemented in the R statistical programming environment32. The package contains one function, convertPrevalence, which simplifies the conversion of prevalence estimates between age bounds. Five arguments were specified for the function. The first, prevalence, is a vector specifying the prevalence, or which PR field in this case, to convert from. Next, age_min_in and age_max_in, are vectors that specify the minimum and maximum ages associated with the estimates given in prevalence. age_min_out and age_max_out are vectors that provide the lower and upper bounds of the age range that the prevalence is to be converted to. Finally, the parameters argument specifies a set of parameters to be used in the model and was set to ‘Pf_Smith2007’ for all P. falciparum conversions and ‘Pv_Gething2012’ for all P. vivax conversions, referring the papers where the models were originally published for each species30,33.
Data Records
Data on each species was abstracted separately and data were disaggregated by age groups where possible. Values were input into a spreadsheet containing 63 fields:
1. Identification
ENL_ID. Data source identification number.
PI_ID. Unique identifier for each record.
INC_AUTHOR. First author surname of incidence data publication.
INC_PUBYEAR. Publication year of incidence data publication.
GRIFFIN. Identifies a record used in the analysis by Griffin et al.17
CAMERON. Identifies a record used in the analysis by Cameron et al.13
BATTLE. Identifies a record used in the analysis by Battle et al.14
EXCLUSION. Potential exclusion criteria as described in Table 2.
SPECIES. P. falciparum (Pf) or P. vivax (Pv).
2. Geo-positioning
REGION. MAP regions are America, Africa+ and CSE Asia.
COUNTRY. Country where ACD was conducted.
ACD_LOCATION. The town/village/district where the ACD was conducted.
LAT. Latitude in decimal degrees (WGS1984 datum).
LONG. Longitude in decimal degrees (WGS1984 datum).
LATLONG_SOURCE. Source of the coordinates: Paper (from the publication), Google22, Encarta23, Other (other online sources or databases), Pers. Comm. (personal communication, usually reporting GPS-read coordinate), GIS (centroid of administrative unit found using ArcGIS)25, or Combination (a combination of the aforementioned methods).
GEOPOS_NOTES. Further information about how geo-positioning was carried out.
EPIZONE. Numerical code for geographic epidemiological zones as defined in Battle et al.27 and as shown in Fig. 4.
BATTLEZONE. The full name of the EPIZONE described above.
3. Incidence time
START_MONTH. Survey starting month.
START_YEAR. Survey starting year.
END_MONTH. Survey ending month.
END_YEAR. Survey ending year.
TIME. Number of years of observation, using fractions to represent <1 year (1 for 12 months, 0.67 for 8 months, 1.33 for 16 months, etc.)
TIME_CAT. Categorizes the TIME column into six categories for the purpose of further exclusion if needed (<6 months, 6–11 months, 12 months, 13–23 months, 24 months, >24 months).
FREQ_ACD. Frequency of ACD written as text (every 2nd day, weekly, fortnightly, etc.). Weekly* indicates a record where the frequency of ACD was not explicitly reported in the study and assumed to be one week.
FREQ_ACD_NUM. This will express the frequency of ACD numerically should scaling be applied downstream. Records the number of days between each visit (every 2nd day=2, every fortnight=14, every month=30).
PCD. Passive Case Detection. Yes/No for if Passive Case Detection was conducted alongside the ACD.
POP. Number of people observed for TIME; the study population.
d. The number of positive species-specific clinical cases. Asymptomatic and mixed infections were not included. Mixed infections were often a negligible proportion of the total infections and present a challenge because it is not possible to determine the parasite that caused the symptomatic episode.
PYO. If person-time is specifically reported in the paper, that value was used after converting to person-years. If person-time was not explicit, the length of the study period (TIME) was multiplied by the study population (POP) such that PYO=TIME * POP.
PYO_APPR. PYO approximated. This is a binary entry to indicate if the PYO was approximated or if an exact PYO was provided in the paper. If PYO=POP*TIME then it was approximated (value 1), and if PYO was reported in the paper (even if it is converted to years from days/weeks/months), then it was exact (value 0).
INC. Incidence=(d/PYO)*1,000. Incidence may have been explicitly reported in the paper. However, the likelihoods are derived from d and PYO and therefore if incidence was provided, the PYO and d were calculated from INC.
INC_NOTES. Description for how incidence values were obtained or derived from information given in the publication.
DIAGNOSTIC. Diagnostic technique used (Microscopy or RDT). Data based on serology or PCR were not included.
CLINICAL_DEF. Clinical Definition. The definition of a clinical case as given in the paper: fever+any parasitaemia or fever+parasitaemia within a fixed or age-dependent threshold (fixed was used if the study reported both).
CASE_DENS_THRESH. Case definition parasite threshold. Some publications specified a minimum parasite load for a patient to be considered a positive case. If any parasite density was permitted, a threshold of 1 was entered, otherwise the value specified in the paper was entered.
4. Incidence population
INC_LAR. Incidence lower age range. If there were multiple age groups studied in one paper, they were entered as separate rows. If no lower age was given, it was assumed to be zero.
INC_UAR. Incidence upper age range. If no upper age was given, it was assumed to be 85.
EIR. Entomological inoculation rate. This was recorded if given in the reference to provide a measure of transmission intensity.
INTERVENTION. Any interventions taking place in the study population. Control and intervention arms should be entered in different rows. For control groups or if there was no intervention, None was entered.
5. Prevalence data
PR_AUTHOR. The author of the source of the parasite rate (PR) data. If the data was found in the same paper as the incidence data, it was entered as Same.
PR_PUBYEAR. The year that the reference that cites the parasite rate was published. If it is the same paper as the incidence paper, it was entered as Same.
PR_MONTH. The month prevalence that the survey was conducted. If not provided, NA was recorded.
PR_YEAR. The year that the prevalence survey was conducted.
N_SURVEYS. This refers to the number of prevalence surveys (XSS) included in the PR estimate reported. Several studies reported PR values that are averaged from more than one survey.
PR_LAR. Lower age range of individuals tested in XSS. If no lower age was given, it was assumed to be zero.
PR_UAR. Upper age range of individuals tested in XSS. If no upper age was given, it was assumed to be 85.
AGE_MATCH. If the PR age range was the same as the incidence age range, the value was 1. If they did not match, the value was 0. If there was no PR value from the paper, the value was 99.
N. Number of individuals examined in the prevalence survey, or if slide positivity rate was reported, the number of slides examined was used.
N_POS. Number of individuals positive for parasite in question.
N_POS_ADJ. Adjusted number positive based on age-standardized prevalence value (PapPR_Stand or PR_Stand below).
PR. Calculated parasite rate=(N_POS/N).
PR_NOTES. Description of how a concurrent PR estimate was obtained.
PR_DIAGNOSTIC. Diagnostic technique used to identify P. falciparum or P. vivax prevalence within the population (microscopy or RDT). Data based serology or PCR were not included.
6. Matched prevalence data
PfPR2_10. Predicted PfPR values from the P. falciparum MAP endemicity surface7.
PvPR1_99. Predicted PvPR values from the P. vivax MAP endemicity surface15.
MAPPR_Stand. Estimate from the P. falciparum or P. vivax MAP surface age-standardized to the age-range used in the incidence data.
PapPR_Stand. Concurrent PR estimate age-standardized to the incidence age-range.
PR_Stand. If a concurrent PR estimate was available, the age-standardized one is used here, if not, the age-standardized MAP estimate is used.
7. Citations
REF_ACD. Reference for the incidence data.
PMID. PubMed identification number for ACD reference. Unpublished sources were left blank, but the type of source (e.g. thesis or conference proceedings) was noted in the full reference given in REF_ACD.
REF_PR. Reference for the PR data (if available).
PMID_PR. PubMed identification for PR reference. Unpublished sources were left blank, but the type of source (e.g. thesis or conference proceedings) was noted in the full reference given in REF_PR. If no concurrently measured PR was found, this was field also left blank.
Technical Validation
There were 1,680 rows of incidence data following initial data extraction (Data Citation 1). All records were entered by one team member and checked by a second. Cells where there was disagreement were highlighted and checked by a third person where possible. Checking was done to ensure that entries were accurate and that the inclusion criteria outlined above were met. Some exceptions to inclusion criteria described were made to allow for studies used in previous analyses5,17 to be added to the database.
To record any exceptions to the inclusion criteria used in the Cameron et al.13 and Battle et al.14 studies and to flag other records for potential exclusion in future analyses, an additional field was added to the database (see EXCLUSION field above). The first exclusion, which applied to both P. falciparum and P. vivax data, was to remove records from different studies that reported the same data (same population at the same time). The records prioritized for inclusion were those that had been included in previous analyses5,17. Next, studies that measured both symptomatic and asymptomatic cases that passed the first inclusion stage, but found during validation, were marked for potential exclusion as the incidence measure would not be specific to clinical cases. Studies with unclear methods, such as un-specified frequency of detection or the number of cases or person-time could not be derived, were also marked for potential exclusion. For P. falciparum, the remaining potential exclusion criteria based on the analysis by Cameron et al.13 was to not include studies that (i) had fewer than four age-specific estimates from the same population during the same time to remove studies under-powered for inference of the P. falciparum age-incidence relationship and or (ii) where the population were treated presumptively at the start of the transmission season. There were only six P. falciparum records excluded from the Cameron et al. analysis for presumptive treatment, but it was noted in INTERVENTION field for other records that had been flagged for potential exclusion for other reasons. For the P. vivax analysis by Battle et al.14, studies that made ACD visits more than one month apart were excluded, as were studies conducted prior to 1985. Incidence reports from retrospective analyses or passive case detection (PCD)-only were marked in the EXCLUSION field, as were XSS because they are not longitudinal and measure both symptomatic and asymptomatic cases. The records flagged as PCD and XSS had originally been abstracted because they were used in previous analyses5,17.
A summary of the exclusion criteria described above is shown in Table 2 and a schematic of the exclusion procedures is shown in Fig. 1. Table 3 shows the regional distribution of the 328 P. falciparum and the 152 P. vivax records remaining after the species-specific exclusions described above were applied. The study by Cameron et al.13 was restricted to Africa, but the lack of data in Africa in the P. vivax analysis conducted by Battle et al.14 represents a genuine absence of P. vivax data in the region. Note that all 1,680 records originally abstracted remain in the database so that customized exclusions can be applied for any future analyses using this data.
Usage Notes
This dataset was generated for the purpose of modelling the relationship between incidence of clinical malaria and the more commonly measured PR. This database has been directly applied to the models described in Cameron et al.13 and Battle et al.14, and is similar to the smaller dataset published by Patil et al.5, with the intention of developing species-specific global burden maps for P. falciparum and P. vivax malaria. Those in turn directly inform global estimates of the burden of clinical disease attributable to each species. This information is critical to efficiently allocate resources and direct efforts to combat these illnesses.
As described above, this database reports incidence of all infections, not only new infections, and therefore include relapses (P. vivax only), recrudescences and reinfections in both the prevalence and incidence measures27,34,35. For P. vivax in particular, these data could be used in conjunction with data on patients who have received radical cure treatment (with either primaquine or tafenoquine) or treatment without primaquine to determine the incidence of new infections or relapses, respectively. This would be done by taking the overall incidence in a location, as reported here, and subtracting the incidence of new infections from patients treated with a radical cure or without a radical cure. This would be essential data for determining sporozoite- and hypnozoite-specific attack rates, the relative proportions of which may directly inform the character of interventions against endemic malaria.
It has been hypothesised that a key driver of relapse in P. vivax is infection with P. falciparum. To allow for investigation of the potential interactions between the endemicity of one species on the incidence of another, a prevalence measure for both P. vivax and P. falciparum is provided for each entry.
This database may also be of use for other analyses of clinical burden. Where possible, data has been disaggregated by age. This allows for studies of how burden of disease changes with age, as was done by Griffin et al. using a smaller dataset of P. falciparum in children in Africa12. The database also contains incidence data from intervention studies with data from both intervention and control arms entered. This would offer insight into the impact of control on incidence of disease as compared to prevalence of infection. Finally, the collection of data from 1985 until the present may improve our understanding in the change of malaria burden over time.
Additional Information
How to cite this article: Battle, K. E. et al. Global database of matched Plasmodium falciparum and P. vivax incidence and prevalence records from 1985–2013. Sci. Data 2:150012 doi: 10.1038/sdata.2015.12 (2015).
References
References
Cibulskis, R. E., Aregawi, M., Williams, R., Otten, M. & Dye, C. Worldwide incidence of malaria in 2009: estimates, time trends, and a critique of methods. PLoS Med. 8, e1001142 (2011).
WHO. World Malaria Report 199 (World Health Organization, 2013).
Murray, C. J. et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 1005–1070 (2014).
Hay, S. I. et al. Estimating the global clinical burden of Plasmodium falciparum malaria in 2007. PLoS Med. 7, e1000290 (2010).
Patil, A. P. et al. Defining the relationship between Plasmodium falciparum parasite rate and clinical disease: statistical models for disease burden estimation. Malar. J. 8, 186 (2009).
Hay, S. I. et al. A world malaria map: Plasmodium falciparum endemicity in 2007. PLoS Med. 6, e1000048 (2009).
Gething, P. W. et al. A new world malaria map: Plasmodium falciparum endemicity in 2010. Malar. J. 10, 378 (2011).
Mendis, K., Sina, B. J., Marchesini, P. & Carter, R. The neglected burden of Plasmodium vivax malaria. Am. J. Trop. Med. Hyg. 64, 97–106 (2001).
Mueller, I. et al. Key gaps in the knowledge of Plasmodium vivax, a neglected human malaria parasite. Lancet Infect. Dis. 9, 555–566 (2009).
Price, R. N. et al. Vivax malaria: neglected and not benign. Am. J. Trop. Med. Hyg. 77, 79–87 (2007).
Snow, R. W., Menon, A. & Greenwood, B. M. Measuring morbidity from malaria. Ann. Trop. Med. Parasitol. 83, 321–323 (1989).
Hay, S. I., Smith, D. L. & Snow, R. W. Measuring malaria endemicity from intense to interrupted transmission. Lancet Infect. Dis. 8, 369–378 (2008).
Cameron, E. et al. Defining the relationship between infection prevalence and clinical incidence of Plasmodium falciparum malaria. Nat. Commun. 6:8170 doi: 10.1038/ncomms9170 (in the press).
Battle, K. E. et al. Defining the relationship between Plasmodium vivax parasite rate and clinical disease. Malar. J. 14, 191 (2015).
Gething, P. W. et al. A long neglected world malaria map: Plasmodium vivax endemicity in 2010. PLoS Negl. Trop. Dis. 6, e1814 (2012).
Guerra, C. A. et al. Assembling a global database of malaria parasite prevalence for the Malaria Atlas Project. Malar. J. 6, 17 (2007).
Griffin, J. T., Ferguson, N. M. & Ghani, A. C. Estimates of the changing age-burden of Plasmodium falciparum malaria disease in sub-Saharan Africa. Nat Commun 5, 3136 (2014).
Rogerson, S. J., Hviid, L., Duffy, P. E., Leke, R. F. & Taylor, D. W. Malaria in pregnancy: pathogenesis and immunity. Lancet Infectious Diseases 7, 105–117 (2007).
Hviid, L. & Staalsoe, T. Malaria immunity in infants: a special case of a general phenomenon? Trends Parasitol. 20, 66–72 (2004).
Baird, J. K. Evidence and implications of mortality associated with acute Plasmodium vivax malaria. Clin Microbiol. Rev. 26, 36–57 (2013).
Poespoprodjo, J. R. et al. Vivax malaria: a major cause of morbidity in early infancy. Clinical Infectious Diseases 48, 1704–1712 (2009).
Google Maps www.google.co.uk/maps/ (Google, Mountain View, CA, 2013).
Microsoft. Encarta Reference Library. (Microsoft Corporation, 2007).
FAO. The Global Administrative Unit Layers (GAUL): Technical Aspects. (Food and Agriculture Organization of the United Nations, EC-FAO Food Security Programme (ESTG, 2008).
ESRI. ArcGIS Desktop 10.0. (Environmental Systems Resource Institute, 2010).
Macdonald, G. . The Epidemiology and Control of Malaria. (Oxford University Press, 1957).
Battle, K. E. et al. Geographical variation in Plasmodium vivax relapse. Malar. J. 13, 144 (2014).
OpenMalaria. ModelDemography: Human population demographics 2014).
Howes, R. E. et al. The global distribution of the Duffy blood group. Nature Commun. 2, 266 (2011).
Smith, D. L., Guerra, C. A., Snow, R. W. & Hay, S. I. Standardizing estimates of the Plasmodium falciparum parasite rate. Malar. J. 6, 131 (2007).
Golding, N. ageStand R package. GitHub https://github.com/SEEG-Oxford (2014).
Core Team., R . R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2013).
Gething, P. W. et al. A long neglected world malaria map: Plasmodium vivax endemicity in 2010. PLoS Negl. Trop. Dis. 6, e1814 (2012).
Imwong, M. et al. The first Plasmodium vivax relapses of life are usually genetically homologous. J. Infect. Dis. 205, 680–683 (2012).
Imwong, M. et al. Relapses of Plasmodium vivax infection usually result from activation of heterologous hypnozoites. J. Infect. Dis. 195, 927–933 (2007).
Data Citations
Battle, K. E. et al. Dryad https://doi.org/10.5061/dryad.j0kv0 (2015)
Acknowledgements
S.I.H. is funded by a Senior Research Fellowship from the Wellcome Trust (095066), which also supports K.E.B., C.A.G., K.A.D. and R.E.H. N.G. is funded by a grant from the Bill & Melinda Gates Foundation (OPP1053338). J.K.B. is supported by Wellcome Trust grant (B9RJIXO). I.R.F.E. is funded by a Public Health and Tropical Medicine Fellowship of the Wellcome Trust (B9RZGS0). P.W.G. is a Medical Research Council Career Development Fellow (K00669X) and receives support from the Bill and Melinda Gates Foundation (OPP1068048), which also supports E.C. D.L.S. is funded by a grant from the Bill & Melinda Gates Foundation (OPP1110495), which also supports R.C.R. R.C.R., D.L.S. and S.I.H. also acknowledge funding support from the RAPIDD program of the Science & Technology Directorate, Department of Homeland Security, and the Fogarty International Center, National Institutes of Health. The authors also thank Joshua Longbottom his for proof-reading and comments.
Author information
Authors and Affiliations
Contributions
K.E.B. drafted the manuscript with editing and approval of all authors. K.E.B. and R.E.H. developed data search and abstraction protocols. K.E.B., C.A.G. and K.A.D. compiled the data records. K.E.B. and C.A.G. performed the technical validation. N.G. wrote statistical software to process and standardise data. E.C. lead the model development. I.R.F.E. and J.K.B. provided data. R.C.R. and J.K.B. provided feedback on data implementation and D.L.S. provided the age-standardization model and feedback on modelling procedures. S.I.H. and P.W.G. conceived the database design and advised on data abstraction and validation procedures.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Additional information
Supplementary Information accompanies this paper at (http://www.nature.com/scidata)
ISA-Tab metadata
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0 Metadata associated with this Data Descriptor is available at http://www.nature.com/sdata/ and is released under the CC0 waiver to maximize reuse.
About this article
Cite this article
Battle, K., Guerra, C., Golding, N. et al. Global database of matched Plasmodium falciparum and P. vivax incidence and prevalence records from 1985–2013. Sci Data 2, 150012 (2015). https://doi.org/10.1038/sdata.2015.12
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/sdata.2015.12
This article is cited by
-
Changing epidemiology of Plasmodium vivax malaria in Nouakchott, Mauritania: a six-year (2015–2020) prospective study
Malaria Journal (2023)
-
Molecular identification of vivax malaria relapse patients in the Yunnan Province based on homology analysis of the Plasmodium vivax circumsporozoite protein gene
Parasitology Research (2023)
-
A dataset of distribution and diversity of blood-sucking mites in China
Scientific Data (2021)
-
Defining the relationship between Plasmodium vivax parasite rate and clinical disease
Malaria Journal (2015)
-
Defining the relationship between infection prevalence and clinical incidence of Plasmodium falciparum malaria
Nature Communications (2015)