Abstract
Introduction
We present a small case series for the rare U-shape sacral fracture. The U-shape sacral fracture is characterised by bilateral longitudinal sacral fractures and a transverse sacral fracture through the S2 vertebral body. Historically it has been described following falls from a height and a high velocity mechanism is often required for this injury. We also describe a surgical technique for fixation of U-shape sacral fractures and subsequent implant removal 6 months post-operatively.
Case Presentation
We present the cases of three patients who presented to our institution with this injury. All patients were treated with minimally invasive, lumbo-sacro-pelvic (LSP) fixation. One patient was lost to follow-up. The remaining two patients had complete resolution of neurological function. These two patients had restoration of lumbosacral motion after removal of implants and had returned to pre-injury function.
Discussion
We describe a new technique for treating U-shape sacral fractures which reduces the morbidity associated with surgery and maintains lumbosacral motion.
Similar content being viewed by others
Introduction
The U-shape sacral fracture is a rare and often unrecognized, unstable fracture pattern. It is an injury characterized by bilateral longitudinal sacral fractures and a transverse sacral fracture through the S2 vertebral body. This fracture configuration results in a dissociation between the lumbosacral spine and the pelvis. For this reason, it is also termed as a spino-pelvic dissociation. The dissociation causes the lumboscaral spine to flex in relation to the transverse axis of the pelvis, thus increasing the patient’s pelvic incidence (PI).
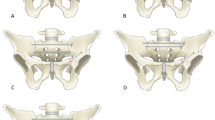
This fracture pattern is most often described following a high energy injury. Roy-Camille described it as a suicide jumper’s fracture as it is often seen in falls from a height. They classified the fracture into three types. Type 1 describes a flexion fracture with an anterior simple bending of the upper sacral fragment. Type 2 describes a flexion fracture with a posterior displacement of the superior fragment that becomes more or less horizontal and settles itself on the fractured surface of the lower fragment. Type 3 describes an extension fracture with anterior displacement of the upper fragment. The fracture pattern often results in a kyphotic deformity.1
We describe a percutaneous approach for Lumbo-Sacro-Pelvic (LSP) fixation. To our knowledge, this has not been previously described in the literature. We routinely remove the hardware at 6 months post injury to maintain lumbosacral motion.
Case presentation
Case 1
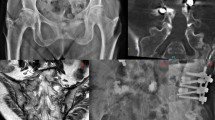
A 22 year old male, was a front seat passenger in a high speed MVA. He suffered multiple skeletal injuries, including a right calcaneus fracture, right tibial plateau fracture, L1, L4 and L5 transverse process fractures, as well as the U-shaped sacral fracture (Figure 1). He suffered neurological deficits as a result of the sacral fracture including saddle anaesthesia and bowel and bladder dysfunction. He had the LSP surgery performed on Day 1 (Figure 2). Post-operatively the patient had ongoing urinary retention and the in-dwelling catheter was left in for a total of 6 weeks. Due to the concomitant injuries, mobility was severely limited post-operatively. Removal of spinal and pelvic fixation was performed 8 months post-operatively after fracture union was confirmed on CT imaging (Figures 3 and 4). At 3 year follow-up he regained full neurological recovery and had unrestricted mobility, however an Oswestry Disability index was performed at this time which scored 23/50, which was severe disability. In light of the full neurological recovery it is noted that the patients’ chief complaints were concomitant limb injuries.
Case 2
A 25 year old female with a background history of Osteogenesis Imperfecta Type 1, sustained an U-shaped sacral fracture and left superior and inferior pubic ramus fractures, following a fall from standing height. Pre-operatively the patient had paraesthesia in L5,S1 and S2 distribution but was otherwise neurologically intact. The patient was transferred from a peripheral hospital. LSP surgery was performed on day 7 post injury. Sensory symptoms completely resolved post-operatively. The patient was mobilized whilst in hospital and discharged to a rehabilitation facility. Spinal and pelvic implants were removed 7 months post initial surgery. At 12 months follow-up she had unrestricted mobility.
Case 3
A 37-year-old male presented to the emergency department with sacral U-shape fracture following a fall from a warehouse roof. His associated injuries were vertebral body fractures to T8, T9, T12 and L1, right calcaneus fracture, right distal radius fracture and right triquetrum fracture. Neurologically, he had altered sensation to all right lower limb dermatomes in association with an L1 burst fracture. The patient suffered from urinary retention post-injury, however he had normal lower limb sensation post-operatively. LSP surgery was performed on Day 1 post injury and the spinal fractures were managed non-operatively with a Thoracolumbar Spinal Orthosis (TLSO) brace. The in-dwelling catheter was left in situ for 6 weeks. Unfortunately, MW was lost to follow-up as he was sent to jail before the surgical implants could be removed.
Surgical technique
The patient is positioned prone on a radiolucent Jackson table. The chest, pelvis and legs are supported by appropriate padded boards. If there is concern of a neurological injury the patient is initially transferred onto a flat top Jackson table in the supine position using standard spinal precautions. The patient is then sandwiched firmly between the two halves of the Jackson table and turned prone.
Percutaneous LSP fixation
Percutaneous pedicle screws are inserted into the L5 and S1 pedicles bilaterally using intra-operative Fluoroscopy (Figure 5).
A 2 cm incision is made obliquely over the posterior inferior iliac spine. A mini open technique is used to cannulate the iliac wing through this incision (Figure 6). A sub-muscular passage is made medially through this incision to gain access to the lateral rods inserted in the sub-muscular plane through the L5/S1 screws from cephalad to caudal direction. With a wide pelvis a side connector may need to be used to connect the lateral rods to the iliac wing screws.
A midline decompression of the S2/S3 level should be performed through a separate midline mini open incision if the patient has a neurological deficit in the S2/3 innervation.
Percutaneous technique pedicle screw insertion technique
With the use of intra-operative fluoroscopy, identify the lateral aspect of the pedicle on an AP radiograph, mark this position on the skin and make a skin incision slightly lateral to this point. Place a Jamshadi needle (JN) through the stab incision and onto the lateral aspect of the pedicle in the 3 o’clock position using fluoroscopy. Pass the needle 10 mm into the pedicle. Confirm that the tip of the JN has now progressed midpoint of the pedicle on the Postero Anterior (PA) view. Advance the JN a further 10 mm in the same trajectory and confirm that the tip of the JN is just medial to the medial wall of the pedicle at the 9 o’clock position on PA fluoroscopy. Then advance the JN another 10 mm and check the position of the tip of the JN which should now be medial to the medial wall of the pedicle on a PA fluoroscopy view. Pass the guide wire through the JN and advance it a further 5 mm beyond the JN into the vertebral body cancellous bone. Insert guide wires into all 4 pedicles and check their position using a lateral fluoroscopic image. Once the guide wire positions have been confirmed on the lateral view, tap the pedicles with a cannulated tap over the guide wires using lateral fluoroscopy as this is done. Then the appropriate length definitive cannulated screws are inserted under lateral fluoroscopy.
The rods are passed in a cephalad to caudal direction in the sub-muscular plain between the reduction tabs of the L5/S1 screws. The caudal end of the rod is then visualized in the mini open incision made to insert the iliac wing screws and connected to it either directly or with a short side connector. The reduction can be achieved by both indirect and direct methods. A closed indirect reduction is achieved using under contoured rods and reduction screws in L5 and S1 to reduce the kyphotic deformity and anterior translation. The direct technique is used when the deformity cannot be reduced closed or when an open approach is required for decompression of the sacral nerve roots. This is done through a separate mini open incision over the S2 fractures site. A bristow or appropriate size cob elevator is used between the nerve roots to lever the anteriorly displaced proximal S2 body fragment back in line with the rest of the distal S2 body.
Iliac wing screw insertion
An oblique 2 cm skin incision is made centered over the Posterior Superior Iliac Spine (PSIS). A longitudinal incision is made into the fascia overlying the PSIS and the tendonous insertions are lifted off the PSIS as a single flap. The rounded surface of the PSIS is flattened using a rongeur. A straight blunt pedicle probe is then passed inferiorly towards the roof of the acetabulum ensuring it remains within the cortices of the ilium at all times. The screw is then measured, tapped and the definitive screw inserted.
Percutaneous transiliac–transsacral screw
Prior to surgery, the sacrum is assessed to ensure a transiliac-transsacral screw can be safely inserted cranial to the transverse limb of the sacral U fracture. This screw is placed through the S1 vertebral body, unless the presence of sacral dysmorphism precludes transsacral S1 fixation. In this situation, the transiliac-transsacral screw can usually be placed safely at the S2 vertebral level, ensuring that the transverse limb of the U fracture is caudal to the S2 body. The safe zone for the placement of the transiliac-transsacral screw can be relatively narrow. We pass this screw prior to inserting the iliac screws. After positioning the patient and confirming the initial fracture reduction, the screw is placed using pelvic inlet/outlet and direct lateral views. A k-wire is used to find the entry point on the inlet and outlet view of the pelvis. The k-wire is then exchanged for a 3.2 mm guide wire. The guide wire is tapped into the cortex of the ilium with a mallet. The wire is then advanced using a power wire driver. After drilling through the lateral cortex of the ilium, the k-wire is advanced if the trajectory and position are perfect as confirmed on inlet and outlet fluoroscopy. If fine adjustments to the trajectory or position are required, then the 5 mm cannulated drill is advanced over the k-wire. The position of the wire or drill is checked on both the inlet and outlet views as it is advanced to ensure adequate cranio-caudal and anterior-posterior positioning. When the wire or drill is positioned at the lateral edge of the upper sacral nerve root tunnel, a true lateral sacral view is obtained. The iliac cortical densities (ICDs) and greater sciatic notches should be superimposed. If the guide wire or drill is caudal and posterior to the ICD and cranial and anterior to the nerve root tunnel, the drill is then advanced once again using the inlet and outlet views on fluoroscopy. The drill is advanced using the oscillate function to reduce risk of injury to nerve roots. This is continued until the drill has breached the iliac cortex on the contralateral side. The tunnel is probed with the blunt end of a k-wire to ensure that the tunnel is within bone. The screw is measured, and a fully threaded 7.0 mm cannulated screw is inserted to prevent overcompression of the fracture.
Discussion
Management of sacral U-shape fractures has been evolving since it was first described. Initially, non-operative management was described for the treatment of minimally displaced fractures without neurological involvement. This involved a period of immobilization with skeletal traction.1 However, the unstable nature of the fracture and dissociation meant that often there would be progressive worsening of the kyphotic deformity and late onset neurological sequelae. In the past 15 years, numerous authors have described percutaneous iliosacral screw fixation with varying levels of success.2,3 The drawbacks of this technique are the ability of a single screw to control the sagittal plane deformity and the inadequate screw purchase if there is significant S1 body comminution.3,4
Triangular osteosynthesis is a form of LSP fixation described by Schildhauer et al.5,6 for the management of a broad group of unstable sacral fractures. They describe pedicle screw insertion into either L4 or L5 as well as an iliac screw with a connecting rod between the two screws secured, once reduction is achieved. In addition one or two percutaneous iliosacral screws are inserted. This study showed that this construct is biomechanically superior to iliosacral screws alone and therefore allows early mobilization. However, they acknowledge that it is major surgery. In their series, they mention that this injury pattern is often associated with significant soft tissue injury. They acknowledge that an extensive approach would be contraindicated in the setting of significant soft tissue injury, although no patients were excluded in their study for this reason. We believe that a percutaneous approach is even more beneficial in this setting.
Studies have shown that minimally invasive spine surgery is associated with reduced blood loss and a decreased requirement for post-operative narcotic analgesia, when compared with open surgery.7,8 The traditional approach is done using a long posterior midline incision and dissection of the Para spinal muscle off the spinous processes to gain access for pedicle screw placement. This approach involves significant muscle stripping that can be associated with destabilizing the midline structures, increased operating time, significant blood loss and increased morbidity for the patient. We believe that this is a significant advantage of the percutaneous approach, especially in the setting of the multi-trauma patient.
Due to the high velocity nature of this fracture pattern, the injury more commonly occurs in a younger age group.1 Therefore we hypothesise that in the long term, maintenance of lumbosacral range of motion is an important factor determining patient outcome. Early implant removal has been shown to maintain lumbosacral motion across the instrumented segments, while minimizing early degenerative changes.9,10 This was demonstrated in our study.
Percutaneous minimally invasive LSP and SI screw fixation can be a safe and viable approach for the treatment of sacral U-shape fractures, particularly in the setting of a multi-trauma patient. Removal of spinal implants once the fracture has healed has the potential advantage of preserving lumbosacral motion especially in the young patient.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Roy-Camille R, Saillant G, Gagna G, Mazel C . Transverse fracture of the upper sacrum. suicide jumper’s fracture. Spine 1985; 10: 838–845.
Konig MA, Seidel U, Heini P, Orler R, Quraishi NA, Boszczyk BM . Minimal-invasive percutaneous reduction and transsacral screw fixation for U-shaped fractures. J Spinal Disord Tech 2013; 26: 48–54.
Nork SE, Jones CB, Harding SP, Mirza SK, Routt ML Jr . Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma 2001; 15: 238–246.
Vilela MD, Jermani C, Braga BP . Arq Neuropsiquiatr. Lumbopelvic fixation and sacral decompression for a U-shaped sacral fracture: case report. Arq Neuropsiquiatr 2007; 65: 865–868.
Schildhauer TA, Josten Ch, Muhr G . Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma 2006; 20 (1 Suppl): S44–S51.
Schildhauer TA, Bellabarba C, Nork SE, Barei DP, Routt ML Jr, Chapman JR . Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma 2006; 20: 447–457.
Peng CW, Yue WM, Poh SY, Yeo W, Tan SB . Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine 2009; 34: 1385–1389.
Lee KH, Yue WM, Yeo W, Soeharno H, Tan SB . Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J 2012; 21: 2265–2270.
Eichinger JK, Arrington ED, Kerr GJ, Molinari R . Bony flexion-distraction injury of the lower lumbar spine treated with instrumentation without fusion and early implant removal: a method of treatment to preserve lumbar motion: two-year follow-up of a teenage patient. J Spinal Disord Tech 2007; 20: 93–96.
Kim HS, Kim SW, Ju CI, Wang HS, Lee SM, Kim DM . Implant removal after percutaneous short segment fixation for thoracolumbar burst fracture: does it preserve motion? J Korean Neurosurg Soc 2014; 55: 73–77.
Author information
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gray, R., Molnar, R. & Suthersan, M. A minimally invasive surgical technique for the management of U-shape sacral fractures. Spinal Cord Ser Cases 3, 17045 (2017). https://doi.org/10.1038/scsandc.2017.45
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2017.45