Abstract
High-amplitude penile vibratory stimulation (PVS) is recommended as the first line method for conservative sperm retrieval in anejaculatory Caucasian men with spinal cord injury (SCI). Evidence of its effectiveness in Asian population is lacking. We described the effectiveness of high amplitude PVS for conservative sperm retrieval in the anejaculatory local men with SCI. Records of all SCI patients referred for conservative sperm retrieval trial from August 2014 to August 2015 were screened. Those who failed in artificial stimulation methods for sperm retrieval including masturbation, prostatic massage and low amplitude PVS were subjected to high amplitude PVS using Viberect X3. Data pertaining to detailed neurological findings, time to ejaculate, seminal fluid volume and its gross appearance, somatic responses at ejaculation and any adverse events were retrieved. Successful outcome is defined as occurrence of antegrade ejaculation. Thirteen out of 16 patients fulfilled all study criteria. 46% of the patients had neurological level above T6 followed by 34% with neurological level between T7-T12. Preserved reflexogenic and spontaneous erection were reported by 84.6% and successful coitus was reported by 45.4% of the patients. The overall ejaculatory success using high amplitude, high-frequency vibratory stimulation in our study was 46.15%. Among the patients with lesion at T6 and above, the ejaculatory success rate was 66.7% while for the study subjects with lesions below T6 was 33.3%. In conclusion, PVS outcome for sperm retrieval in asian population is comparable to that of Caucasian population. Its use is highly applicable in local population.
Similar content being viewed by others

Spinal cord injury (SCI) is usually associated with sexual impairment affecting reproductive function. Although spinal injury rehabilitation is well established in most centers, sexual education is often poorly integrated into the rehabilitation process,1,2 even though the people with SCI do have sexual interest both from recreational and reproductive point of view.3 The effect of SCI on sexual response depends not only on the level and severity of injury, but also contributed by personal factors such as partnership status, pre-morbid sexual experiences and attitudes and openness to sexual experimentation.4,5
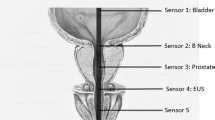
Although normal sexual and reproductive functions depends largely on intact neurological mechanisms6, SCI in men, induces a disruption to the nerve supply responsible for erection and ejaculation, which commonly causes both erectile dysfunction (ED) and impairment in ejaculation process.6,7 The basic mechanisms for erection are however preserved in most men with SCI; hence the same treatments used for the management of ED in non-injured men can be applied in men with SCI. Oral phosphodiesterase-5 inhibitors, penile injection therapy with vasoactive agent and vacuum device are a few methods that can be employed to assist in obtaining sustainable erection.8 Meanwhile, the ejaculatory reflex is coordinated by the spinal cord assisted by thoracolumbar sympathetic fibers from segments T10–L2 and somatic fibers from segments S2–S4. Stimulation at the glans penis will activate the dorsal nerve of the penis to relay somatic input to activate the ejaculatory reflex. Furthermore, neurons in the cortex, thalamus, hypothalamus, midbrain and pons, also has a role in ejaculation.9,10
In SCI men, there is usually complete malfunction of the ejaculatory reflex, hence, medications will, of course, have little effect. Studies also reported that only ~9% of men with SCI can ejaculate through masturbation or intercourse. As the result, most men with SCI require some form of medical assistance to obtain sperm for insemination. Penile vibratory stimulation (PVS) and electro ejaculation are the most common techniques used for sperm procurement, failing which; surgical sperm retrieval can be done.8 Although the use of vibratory stimulation for sperm retrieval is well established in the Caucasian population, to our knowledge, there is a dearth of evidence to support its application involving Asian population.
This retrospective case series was collected over a year, from August 2014 to August 2015. This study was conducted in the Department of Rehabilitation Medicine, Hospital Sungai Buloh, Malaysia. Records of all SCI patients referred for conservative sperm retrieval trial at our centre during the study period were screened. The inclusion criteria were (i) patients with confirmed spinal cord injury of traumatic etiology (ii) complete lesions (iii) duration of injury of >2 years (iv) had never ejaculated (v) failed masturbation, prostatic massage and low amplitude vibratory stimulation trial to induce ejaculation and (v) consented to the study. The exclusion criteria were (i) uncontrolled medical problems (ii) anatomical and structural deformities of the genital tract (iii) genitalia wounds/infections and (iv) non consenting patients.
Patients enrolled in this study were admitted and subjected to full neurological assessment including per rectal examination; conus medullaris reflexes evaluation; and cremasteric, abdominal and spinal withdrawal reflexes assessments. Quality of erection was graded based on description by patients using Erection Hardness Score. The Erection Hardness Score is a simple, valid and reliable one-item questionnaire that assesses rigidity on a 4-point scale.11 Spasticity evaluation was also performed and its severity was graded using Modified Ashworth Scale. Modified Ashworth Scale is commonly used in grading spasticity and it is an acceptable tool for assessing overall muscular tone in spinal cord population.12 The artificial stimulation methods tried for the patients include use of low amplitude, low frequency vibratory stimulation and prostatic massage. Low amplitude vibratory stimulation device used in this study involved the use of muscle massager device to deliver amplitude of 1.5 mm when applied to the penis. Stimulation is performed over the glans of penis either at the frenulum or dorsum for continuous 2 min with 1 min rest in between until ejaculation occurred or completed five cycles. For the prostatic massage, a gloved index finger is inserted into the patient's rectum and gentle pressure was applied to the prostate gland to mechanically push the seminal fluid out of the ejaculatory ducts and urethra. This procedure is performed repetitively until ejaculation occurred or completed five attempts. If both procedures failed, a specifically designed high-amplitude penile vibratory stimulation device to induce ejaculation in anejaculatory men following SCI, the Viberect X3 is used. The amplitude is preset at 4 mm and the frequency is adjusted to 110 Hz. Stimulation is performed simultaneously over the dorsum and ventral of the glans penis for continuous 2 min with 1 min rest in between until ejaculation occurred or completed five cycles. Successful outcome is considered if antegrade ejaculation occurred. Time to ejaculate, seminal fluid volume and its gross appearance, somatic response at ejaculation and any adverse events were all recorded.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this review.
The baseline demographic and clinical characteristic such as age, etiology, level and severity of spinal cord injury, duration of the injury of the participants were recorded. Detailed neurological evaluation as described in the methodology section were recorded and analyzed. Frequency and descriptive analyses were performed for all numerical and categorical data. The results were presented in Table 1.
Out of a total of 16 patients referred for fertility intervention during the study period, 13 fulfilled all study criteria. With reference to Table 1, the average age of the patients with traumatic SCI was 36.46 years (range 26–50 years). Motor vehicle accident was the common cause of injury (84.6%), followed by fall from height (15.4%). The time since injury was 10.07 years (range 2–20 years). Forty six percent of the patients had neurological level of T6 and above followed by 34% with neurological level between T7–T12. Preserved reflexogenic and spontaneous erection were reported by 84.6% of the patients, out of which 72.7% had had previous experience with the use of Sildenafil Citrate to improve their erectile function. Successful coitus was reported by 45.4% of the patients. The overall ejaculatory success using high amplitude, high-frequency vibratory stimulation in our study was 46.15%. Among the study patients with lesion at T6 and above, the ejaculatory success rate was 66.7% while for the patients with lesions below T6 was 33.3%. It was observed that all patients with successful ejaculation have intact conus medullaris reflexes with presence of significant abdominal and lower limb spasticity. Most ejaculation occurred in <3 min of vibratory stimulation, only one patient achieved ejaculation following 10 min stimulation. Out of six ejaculation fluids collected, only one sample is observed to be dark brown colour (‘rusty pipe syndrome’) while the rest are either thick or thin cloudy fluids as illustrated in Figures 1 and 2. The somatic responses observed pre-ejaculation include mild erection, increasing abdominal and lower limbs spasticity and spinal withdrawal reflex response. Adverse event observed in this study was symptomatic autonomic dysreflexia and penile edema in one (7.6%) of the study subjects.
PVS is recommended as the first line treatment for seminal ejaculation in men with SCI because of its safety profile, reliable and cost-effective compared with other methods.7–9 PVS involves placing a vibrator on the dorsum or frenulum of the glans penis. Mechanical stimulation produced by the vibrator recruits the ejaculatory reflex to induce ejaculation. The procedure of PVS has been well described in previous publications. PVS is more effective in men with an intact ejaculatory reflex (level of injury T10 or higher) as ejaculatory success requires an intact dorsal penile nerve terminating in sacral spinal cord segments S2–S4.8,13
The average age in our study subjects was 36.46 years with reported reserved reflexogenic and spontaneous erection in 84.6%. Successful coitus was reported by 45.4% of the study subjects. These findings were in keeping with many other western literatures, of which most SCI men are usually younger than 45 years and with reported frequency of erection in 54–95% of them. Successful coitus ranges from 5 to 75%, and ejaculation ranges from 3 to 20% of them.13,14
Many studies have reported that factors that determine the ejaculatory success rate in PVS trials are the vibrator’s amplitude15 and the level of SCI. High-amplitude vibrators yield higher success rates compared with low-amplitude vibrators (54.5% versus 39.9%, respectively). In addition, the higher the level of injury the better the ejaculatory success rate of PVS regardless of the type of the vibrator used (high or low amplitude).16 The results of previous PVS trials show an overall success rate of ejaculation of 49.8% (ref. 17) or higher (54%) if men injured below T10 are excluded.18 The thoracolumbar emission center is located between T10 and L3 levels. Thus, a higher lesion spares the ejaculatory reflex arc.
In comparison, the overall ejaculatory success using high amplitude, high-frequency vibratory stimulation in our study was 46.15%. Among the study patients with lesion at T6 and above, the ejaculatory success rate was 66.7% while for the study subjects with lesions below T6 was 33.3%.
The authors observed that all patients with successful ejaculation has intact conus medullaris reflexes, presence of significant abdominal and lower limb spasticity and positive spinal withdrawal reflex in either side of the lower limbs. The somatic responses observed pre-ejaculation include mild erection, increasing abdominal and lower limbs spasticity and spinal withdrawal reflex response. Dimitriadis et al.7 reported similar findings that somatic responses are observed in 100% of trials that result in ejaculation. These responses may involve: contraction of the abdominal muscles, spasticity below the level of injury, knee flexion, hip flexion and abduction of the thighs. Periurethral muscle contractions may be felt in most of the trials in which ejaculation has occurred. Other prognostic factors for ejaculatory success in PVS reported in literature include SCI lesion above T10, triple flexion response involving the hip, knee, ankle to plantar stimulation19–21 and presence of bulbocavernosus reflex.21 Stopping the anti-spasticity medications before using PVS to enhance reflexes that may be aiding ejaculation is commonly practice in many fertility clinics for men with SCI.22 Some sympathomimetic agents such as ephedrine, midodrine may also be used to facilitate ejaculation.23
In conclusion, the effectiveness of PVS for sperm retrieval in asian population is comparable to that of Caucasian population. Thus, its use is highly applicable for SCI rehabilitation in our local context. In our experience, lesions above T6; intact conus medullaris reflexes; significant abdominal and lower limb spasticity; and positive spinal withdrawal reflexes in either lower limb are highly predictive of ejaculatory success with PVS.
References
Tepper MS . Sexual education in spinal cord injury rehabilitation: Current trends and recommendations. Sex Disabil 1992; 10: 15–31.
McAlonan S . Improving sexual rehabilitation services: the patient’s perspective. Am J Occup Ther 1996; 50: 826–834.
Alexander MS, Brackett NL, Bodner D, Elliott S, Jackson A, Sonksen J et al. Measurement of sexual functioning after spinal cord injury: preferred instruments. J Spinal Cord Med 2009; 32: 226.
Kreuter M, Sullivan M, Siösteen A . Sexual adjustment and quality of relationships in spinal paraplegia: a controlled study. Arc Phys Medi Rehabil 1996; 77: 541–548.
Drench ME . Impact of altered sexuality and sexual function in spinal cord injury: A review. Sex Disabil 1992; 10: 3–14.
Fode M, Krogh-Jespersen S, Brackett NL, Ohl DA, Lynne CM, Sonksen J . Male sexual dysfunction and infertility associated with neurological disorders. Asian J Androl 2012; 15: 61–68.
Dimitriadis F, Karakitsios K, Tsounapi P, Tsambalas S, Loutradis D, Kanakas N et al. Erectile function and male reproduction in men with spinal cord injury: a review. Andrologia 2010; 42: 139–165.
Giuliano F, Clement P . Neuroanatomy and physiology of ejaculation. Annu Rev Sex Res 2005; 16: 190–216.
Coolen LM, Allard J, Truitt WA, McKenna KE . Central regulation of ejaculation. Physiol Behav 2004; 83: 203–215.
Brackett NL, Ibrahim E, Iremashvili V, Aballa TC, Lynne CM . Treatment for ejaculatory dysfunction in men with spinal cord injury: an 18-year single center experience. J Urol 2010; 183: 2304–2308.
Mulhall JP, Goldstein I, Bushmakin AG, Cappelleri JC, Hvidsten K . Validation of the erection hardness score. J Sex Med 2007; 4: 1626–1634.
Tederko P, Krasuski M, Czech J, Dargiel A, Garwacka-Jodzis I, Wojciechowska A . Reliability of clinical spasticity measurements in patients with cervical spinal cord injury. Ortop Traumatol Rehabil 2007; 9: 467–483.
Bors E, Comarr AE . Neurological disturbances of sexual function with special reference to 529 patients with spinal cord injury. Urol Surv 1960; 10: 191–222.
Biering-Sørensen F, Sønksen J . Penile erection in men with spinal cord or cauda equina lesions. Semin Neurol 1992; 12: 98–105.
Brackett N . Penile vibratory stimulation for men with spinal cord injury. Hum Reprod 1999; 5: 551–552.
Brackett NL . Semen retrieval by penile vibratory stimulation in men with spinal cord injury. Hum Reprod 1999; 5: 216–222.
Brackett NL, Ferrell SM, Aballa TC, Amador MJ, Padron OF, Sonksen J et al. An analysis of 653 trials of penile vibratory stimulation in men with spinal cord injury. J Urol 1998; 159: 1931–1934.
Nehra A, Werner MA, Bastuba M, Title C, Robert D . Vibratory stimulation and rectal probe electroejaculation as therapy for patients with spinal cord injury: semen parameters and pregnancy rates. J Urol 1996; 155: 554–559.
Brindley G . The fertility of men with spinal injuries. Spinal Cord. 1984; 22: 337–348.
Ohl DA, Menge AC, Sønksen J . Penile vibratory stimulation in spinal cord injured men: optimized vibration parameters and prognostic factors. Arc Phys Medi Rehabil 1996; 77: 903–905.
Bird V, Brackett N, Lynne C, Aballa T, Ferrell S . Reflexes and somatic responses as predictors of ejaculation by penile vibratory stimulation in men with spinal cord injury. Spinal Cord. 2001; 39: 514–519.
Gilja I, Parazajder J, Radej M, Cvitković P, Kovacić M . Retrograde ejaculation and loss of emission: possibilities of conservative treatment. Eur Urol 1993; 25: 226–228.
Riley A, Riley E . Partial ejaculatory incompetence: the therapeutic effect of midodrine, an orally active selective alpha-adrenoceptor agonist. Eur Urol 1981; 8: 155–160.
Acknowledgements
We would like to thank the Director General of Health Malaysia for his permission to publish this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zamli, A., Ismail, N. & Ong, K. Retrospective review on effectiveness of high-amplitude penile vibratory stimulation for conservative sperm retrieval in anejaculatory men with spinal cord injury: an Asian case series. Spinal Cord Ser Cases 2, 15038 (2016). https://doi.org/10.1038/scsandc.2015.38
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2015.38